Year: 2012 Vol. 78 Ed. 2 - (3º)
Artigo Original
Pages: 11 to 15
Result on speech perception after conversion from Spectra® to Freedom®
Author(s):
Ana Tereza de Matos Magalhães1; Maria Valéria Schmidt Goffi-Gomez2; Ana Cristina Hoshino3; Robinson Koji Tsuji4; Ricardo Ferreira Bento5,; Rubens Brito6
Keywords: adult, audiometry, cochlear implants, speech discrimination tests, speech perception.
Abstract:
New technology in the Freedom® speech processor for cochlear implants was developed to improve how incoming acoustic sound is processed; this applies not only for new users, but also for previous generations of cochlear implants.
AIM: To identify the contribution of this technology - the Nucleus 22® - on speech perception tests in silence and in noise, and on audiometric thresholds.
METHODS: A cross-sectional cohort study was undertaken. Seventeen patients were selected. The last map based on the Spectra® was revised and optimized before starting the tests. Troubleshooting was used to identify malfunction. To identify the contribution of the Freedom® technology for the Nucleus22®, auditory thresholds and speech perception tests were performed in free field in sound-proof booths. Recorded monosyllables and sentences in silence and in noise (SNR = 0dB) were presented at 60 dBSPL. The nonparametric Wilcoxon test for paired data was used to compare groups.
RESULTS: Freedom® applied for the Nucleus22® showed a statistically significant difference in all speech perception tests and audiometric thresholds.
CONCLUSION: The reedom® technology improved the performance of speech perception and audiometric thresholds of patients with Nucleus 22®.
![]()
INTRODUCTION
The first Brazilian multichannel cochlear implant surgeries were done in 19991, using the Spectra Bodyworn speech processor, from Cochlear Corporation®, which works well with the Nucleus 22®internal unit.
Throughout the years, new Technologies have been launched and cochlear implant companies developed speech processors for the previous internal units, avoiding the need for a new surgical procedure2-4.
In 2006, the Freedom®processor was launched, with new Technologies, among which two microphones and a new chip for signal processing, providing improvements in the processing of the input acoustic sound, not only for new users but also for patients with previous generations of cochlear implant.
In 2009, the replacement parts for the Nucleus 22®system were no longer manufactured. The Ministry of Health, then, authorized the exchange, through the Brazilian Public Health Care System (SUS), of all the Nucleus 22®speech processors for the Freedom®speech processors.
In the scientific literature, numerous studies have shown the advantage in exchanging it for more modern processors; nonetheless, the direct exchange of the Spectra®for the Freedom®was not studied, nor reported3,5.
Therefore, this study aimed at identifying the contribution of the Freedom®speech processor technology for the first generation of the Nucleus 22® multichannel cochlear implant. For that, we assessed the speech perception performance in silence and in noise and the audiometric thresholds with the Spectra®and Freedom® speech processors.
METHODS
This Project was presented to and approved by the Ethics Committee for the Analysis of Research projects of the institution under protocol number 0083/11. The patients were informed about the research and signed the informed consent form.
The study was a cross-sectional historical cohort, assessing the results obtained with the update of the speech processor technology of the Nucleus 22® cochlear implant.
We selected 43 patients implanted with the Nucleus 22®in the Cochlear Implant Group of the University Hospital of the Medical School of the University of São Paulo (USP). This way, five patients were no longer users of the cochlear implant, eight patients were already users of the Freedom®processor. The remaining 30 patients kept using the Spectra® processor and came to change the speech processor, offered by the Brazilian Government through the Ministry of Health.
In the study, we included the patients who were effectively using the implant (8 hours per day), and we took off the study those patients using it occasionally or those who did not have speech perception in the closed context. Six patients were not effective users, four patients were children and three patients did not have speech perception. Ultimately, the study included 17 patients.
The patients called followed the following protocol, broken down into three stages:
a. First stage: optimization of the current map and checking how the Spectra®processor worked
At this first stage, the last map being used by the patient with the Spectra® processor was reviewed and updated according to the programming routine with the Custom Sound 2.0®software. We studied the minimum stimulation levels (level T), in which the patient identifies 100% of the presentations; the maximum levels of stimulation (level C) for those whom the electric current presented is comfortable and the level C intensity was balanced. Before doing the tests, the Spectra®processor functioning was checked, inspecting the wires, antenna transmission and microphone, using a signal checking device and the monitoring phone. Should any fault be found, the component would be replaced before the tests.
b. Second stage: programming the Freedom processor
We exchanged the Freedom®processor, maintaining the other parameters of the original map: total stimulation velocity and stimulation mode, without a signal pre-processing strategy. We balanced the intensity of the T and C stimulation levels with the Custom Sound 2.0®software.
c. Third stage: assessing the audiometric thresholds and the speech perception tests
We carried out free field audiometry, with the Spectra®and the Freedom®speech processors. In order to do the statistical calculation, we considered the mean values of the audiometric thresholds at 500 Hz; 1,000 Hz; 2,000 Hz and 4,000 Hz6and the frequency thresholds individually.
In the same session, after programming all the maps, the following free field speech perception tests were carried out in a sound-treated booth, with the material recorded in a CD, presented at 60dBSPL7:Monossylables8,9; Open phrases in the silence10; Open phrases in noise with SNR = 0dB*10
* These tests were only employed when the phrase recognition performance in silence was higher than 50%.
The order in which the tests with the Spectra®processor maps and the new maps with the Freedom®processor was randomized using the software available at www.randomizer.org
The audiometric thresholds, percentage of correct answers in the speech perception tests are presented as means and standard deviation (SD) and also as median and the percentiles 25% and 75% (P25% and P75%, respectively). Considering the small sample size, the ordinal nature and asymmetrical distributions of some variables, the Wilcoxon non-parametric test for paired data was utilized in order to compare the groups. The analysis of the parametric sensitivity utilizing the t test was carried out in all the comparisons and it did not change the results. A p < 0.05 was considered as statistically significant.
The statistical analyses were carried out using the STATA software (version 11.1).
RESULTS
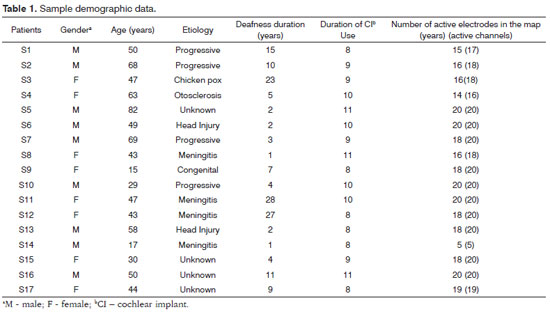
Table 1 depicts the demographic data of the sample.
Most of the sample is made up of patients with more than eight years of experience using the cochlear implant. Only two were teenagers, and one of them had congenital deafness.
When we analyzed the contribution of the Freedom® for patients using the Nucleus 22®, we noticed a statistically significant difference in all the speech perception tests and in all audiometric thresholds, both individually as in the mean, except in 8,000 Hz (Tables 2 and 3).
DISCUSSION
Exchanging the Spectra®processor for the Freedom®proved that the technology improved the speech perception of Nucleus 22®users. Even when maintaining the same parameters of the stimulation mode, the total velocity and number of active electrodes, we can see a statistical difference in all the tests and in all the audiometric thresholds (Tables 2 and 3).
The scientific literature has shown that there are advantages when the speech processor is exchanged for more modern devices. Dodd et al.3published their results concerning the exchange of the Spectra® box processor for the ESPrit®behind-the-year processor in 100 children; and they concluded that the conversion was feasible in all the cases studied, although the speech tests and audiometric thresholds did not show significant differences.
Santarelli et al.5assessed the speech perception in 17 prelingual children users of the Nucleus 24®with the SPrint®and ESPrit 3G®processors, after one month using the Freedom®processor. As results, the children had a significant improvement in the dissyllable words in the presence of noise, identification of consonants and phrase recognition. These improvements in phonemic discrimination may be explained by an increase in the input dynamic field with the new processor. They concluded that the speech perception was higher with the Freedom®, being advisable to exchange for the new generation of processors. Moreover, all the children preferred the new processor.
This shows the importance and the care taken by cochlear implant manufacturers in developing new processors, matching the internal units of previous generations, so that these patients may enjoy the new technology and, consequently, improve their performance, but also enable more flexibility in programming, keeping the characteristics and the preference of the old program used by the patient.
The possibility of keeping the same parameters of the old processor in use shows that only changes to the microphone and the signal processing have been enough to the processor's contribution in improving speech perception.
One of the parameters maintained was the stimulation mode. When one electrode is stimulated, the current flows from the active electrode to the ground one; and the broader the spacing between the electrodes the lower the necessary current.
Although the Freedom®has the BP+3 (bipolar, one active electrode and another as indifferent) stimulation mode as a standard for users of the Nucleus 22®, all the patients could maintain their modes of stimulation. With the aim of analyzing only the benefit of all the parameters studied, without harming the use of batteries, the stimulation modes utilized were maintained, i.e. BP+1 for all, except one patient who used the CG mode (common ground uses all the electrodes as different electrodes). Battery use was measured by the Custom Sound 2.0® software, finding an average of 8.6 hours for rechargeable batteries and 24.1 hours for the three 675 batteries. There were only two patients who had problems with battery consumption, with only 6 hours of battery life, which was solved by changing the power of the antenna magnet.
In this same sample, other technological resources were analyzed, as the effect of the frequency allocation table and the T-SPL effect of 25dB and that of the C-SPL of 65dB, which will be published later.
CONCLUSION
The Freedom®processor technology for users of the Nucleus 22®showed a statistically significant improvement in all speech tests in silent environments at 60 dB and in noise, with a signal/noise ratio of 0 dB, as well as in all audiometric thresholds.
REFERENCES
1. Bento RF, Brito Neto RV, Castilho AM, Goffi-Gomez MVS, Sant'Anna SBG, Guedes MC. Resultados auditivos com o implante coclear multicanal em pacientes submetidos à cirurgia no Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo. Rev Bras Otorrinolaringol. 2004;70(5):632-7.
2. Parkinson AJ, Parkinson WS, Tyler RS, Lowder MW, Gantz BJ. Speech perception performance in experienced cochlear-implant patients receiving the SPEAK processing strategy in the Nucleus Spectra-22 cochlear implant. J Speech Lang Hear Res. 1998;41(5):1037-87.
3. Dodd MC, Nikolopoulos TP, Totten C, Cope Y, O'Donoghue GM. Cochlear implants: 100 pediatric case conversions from the body worn to the nucleus esprit 22 ear level speech processor. Otol Neurotol. 2005;26(4):635-8.
4. Välimaa TT, Löppönen HJ. Comparison of the body-worn CIS-PRO and the behind-the-ear-worn TEMPO cochlear implant systems in Finnish-speaking adult CI users: any differences in results with experienced listeners? Acta Otolaryngol. 2008;128(9):984-91.
5. Santarelli R, Magnavita V, De Filippi R, Ventura L, Genovese E, Arslan E. Comparison of speech perception performance between Sprint/Esprit 3G and Freedom processors in children implanted with Nucleus Cochlear Implants. Otol Neurotol. 2009;30(3):304-12.
6. Bureau Internacional d'Audio Phonologie.Audiometric classification of hearing impairment: recommendation 02/1, 1996. Disponível em: http://www.biap.org/biapanglais/rec021eng.htm Acessado em 20 de dezembro de 2010.
7. Goffi-Gomez MVS, Guedes MC, Sant'Anna SBG, Peralta CGO, Tsuji RK, Castilho AM, et al. Critérios de Seleção e Avaliação Médica e Audiológica dos Candidatos ao Implante Coclear: Protocolo HCFMUSP. Arq Int Otorrinolaringol. 2004;8(4):303-13.
8. Pen MG, Mangabeira-Albernaz PL. Lista de monossílabos para discriminação vocal. Em: Mangabeira-Albernaz PL, Ganança MM, editores. Surdez neuro-sensorial. São Paulo: Moderna; 1976. p.20.
9. Pereira LD, Schochat E. Processamento auditivo central: manual de avaliação. 1a ed. São Paulo: Lovise; 1997.
10. Costa MJ, Iorio MCM, Mangabeira-Albernaz PL. Desenvolvimento de um teste para avaliar a habilidade de reconhecer a fala no silêncio e no ruído. Pro Fono. 2000;12(2):9-16.
1. MSc student - FMUSP (Speech and Hearing Therapist of the Cochlear Implant Team of the University Hospital - Medical School of the University of São Paulo - HC-FMUSP).
2. PhD in Sciences - Federal University of São Paulo (Speech Therapist of the Otorhinolaryngology Clinic at the University Hospital of the Medical School of the University of São Paulo - USP; Coordinator of the Speech and Hearing Therapy team of the Cochlear Implant Team of the HC-FMUSP).
3. PhD Student - Federal University of Rio de Janeiro (Speech and Hearing Therapist).
4. PhD - FMUSP (ENT physician - University Hospital - USP; Coordinator of the Cochlear Implant Team - HC-FM-USP).
5. Full Professor of the Ophthalmology and Otorhinolaryngology Department of the Medical School of the University of São Paulo (FMUSP) - Otorhinolaryngology Course (Head of the Ophthalmology and Otorhinolaryngology Department - FMUSP).
6. Senior Associate Professor of Otorhinolaryngology Program of the Medical School of the University of São Paulo (FMUSP); Assistant Physician of the Otorhinolaryngology Department of the University Hospital of the University of São Paulo).
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on June 06, 2011
And accepted on October 11, 2011. cod. 8063.