Year: 2012 Vol. 78 Ed. 1 - (10º)
Artigo Original
Pages: 62 to 67
Correlation between vestibular test results and self-reported psychological complaints of patients with vestibular symptoms
Author(s): Léia Gonçalves Gurgel1; Michelle Ramos Dourado2; Taís de Campos Moreira3; Adriana Jung Serafini4; Isabela Hoffmeister Menegotto5; Caroline Tozzi Reppold6; Cristina Loureiro Chaves Soldera7
Keywords: electronystagmography, speech, language and hearing sciences, psychopathology, vertigo.
Abstract:
Cognitive and emotional factors may affect balance; psychiatric conditions are a common component in patient dizziness. The treatment of patients with vertigo may be affected to a greater degree by the suffering due to this disease than by the severity of organic changes.
OBJECTIVE: This study aimed to investigate associations between vestibular test results and self-reported psychological complaints in patients evaluated during 2009 in an audiology unit at a hospital in Porto Alegre.
METHODS: We conducted a retrospective, descriptive-exploratory study of data taken from a database of the software VecWin® and VecWin® 2, developed by Neurograff®. We investigated vestibular test results, reports of psychological symptoms reported spontaneously, and information such as age, sex and the presence of vertigo and/or dizziness. This study consisted of three steps: clustering, exclusion/inclusion and quantification.
CONCLUSION: Age and gender and the presence or absence of vertigo and/or dizziness were not variables that influenced the outcomes of vestibular testing. There was a significant association between the presence of self-reported psychological complaints and normal vestibular test results. Thus, it is crucial that professionals pay attention to psychological issues reported by patients when the vestibular history is taken.
![]()
INTRODUCTION
Otoneurology is the study of the auditory and vestibular systems and their relationship with the central nervous system (CNS)1. Vestibulometry is a set of procedures for evaluating bodily balance. Computed vectoelectronystagmography (VENG) is a step in vestibulometry; it is a method for recording ocular movements that are directly or indirectly related with vestibular function2. VENG establishes the direction of nystagmus and calculates the velocity of its slow component, a fundamental parameter for assessing the function of the labyrinth2.
Vestibular disorders significantly hamper individuals; they may require assistance for even the simplest tasks that previously were part of their normal lives3. Vestibular disorders include peripheral vestibular diseases (comprising diseases of the inner ear and/or the vestibular branch of the eight cranial nerve) and central vestibular diseases (involving structures, nuclei, pathways, and vestibular interrelationships within the central nervous system)4.
Manifestations of vestibular diseases include dizziness and/or unbalance, which affect about 10% of the world population3. Dizziness and unbalance are considered the most common complaints after 65 years of age and comprise 5% to 10% of medical visits per year3. One of the reasons that dizziness is such a common symptom is its diverse etiology, which may include diseases of the labyrinth, cardiovascular conditions, neurological diseases (multiple sclerosis, tumors, epilepsy, ischemic attacks, and drug intoxication), and psychogenic factors5,6. The physical and emotional conditions that cause dizziness may result in severe loss of function that compromise work, social relations, and domestic activities of patients3. Often, vestibular disorders are accompanied by hearing loss and neurovegetative disorders such as nausea, vomiting, intense sweating, and pallor1.
The relationship between anxiety and balance is based on the premise that balance disorders and anxiety share central neural circuits with monoaminergic components. These circuits are centered on a network in the parabranchial nucleus, which is a point at which the vestibular system and the area for processing visceral information converge; this network also involves symptoms of avoidance, anxiety, and fear7.
It should be noted that a complain t is the first moment of contact between a patient and a healthcare professional; this moment concerns the manifest and conscious contents of the symptom. An initial interview for examining the vestibular system should offer a space for listening and care, so that the patient may speak not only of the symptom, but of his or her suffering as related to it8. Therapy may be more influenced by the suffering and behavior of the disease than by the severity of organic findings3. Thus, this study is relevant because a high proportion of otoneurologic patients present psychological disorders3. The purpose of this study was to investigate associations between the results of vestibular testing and self-reported psychological symptoms in individuals seen at an audiology unit in a hospital in the city of Porto Alegre, RS, from January to December 2009.
MATERIAL AND METHODS
A retrospective and descriptive-exploratory study was made of the available data of a sample consisting of 304 subjects; data were gathered from January to July 2010. The institutional review boards of the participating entities approved this study (numbers 341/10 and 10/597). The work consisted of studying a database, which did not require subjects to sign a free informed consent form. The institutional review boards authorized the researchers to divulge the data related to the study sample.
Data was gathered by consulting the databases of the VecWin® and VecWin® 2 softwares, which are used in recording and analyzing vectoelectronystagmography tests at our institution. The computed vectoelectronystagmography unit was a Neurograff® Eletromedicina Ind. & Com. Ltd. device, which has its own software (VecWin®) and a light bar for presenting visual stimuli9. The VecWin® software is stored in the computer memory and records clinical history data as well as the vestibular-ocular-motors reflexes resulting from visual stimulation10.
The same speech therapist gathered the clinical histories and carried out the tests, which were recorded in the VecWin® or VecWin® 2 softwares. Patients were not asked directly about psychological complaints; when these were made, they were done so spontaneously; the examiner recorded these complaints when they were offered at any point during history taking or testing. For this study, age, sex, complaint of dizziness and/or vertigo, self-reported psychological complaints, and vestibular test results were recorded.
The study consisted of three steps: gathering and grouping, inclusion/exclusion, and analysis/quantification. At first, data recorded in the software was gathered and grouped into five categories: age, sex, complaint of dizziness and/or vertigo, self-reported psychological complaints, and results of vestibular testing. Psychological complaints were classified based on a previously published method and according to the words of patients themselves, as follows: anguish, depression, fear, anxiety, and memory disorders11. Other parameters were added after analyzing the database, namely: stress12, lasitude12, irritability12, panic13, insecurity14, and discomfort15; this depended on whether these self-reported complaints were present in the study sample. The latter were established by applying Bardin's analysis16, which refers to content analysis (study of figures of speech, reticence, between the lines content, manifest content, etc.) of the discourse. These are a set of communications analysis techniques that take into account human subjectivity and the meanings that research subjects attribute to content. The aim to is apply systematic and objective procedures to gather quantitative or non-quantitative measures to infer knowledge about the status of message production/reception (inferred variables)16.
Secondly, data of all subjects (315 individuals) that underwent vestibular testing from January to December 2009 were included. Eleven of these subjects were excluded from the study because their tests were inconclusive or the clinical history was incomplete. The resulting sample comprised 304 subjects.
In the last step, a statistical analysis was made of the data; the software for this purpose was the Statistical Package for the Social Science (SPSS) version 18.0. The chi-square test was applied to evaluate associations among the results of vestibular testing and the age group, sex, complaint of vertigo and/or dizziness, and self-reported psychological complaints; the significance level was 5% (p = 0.05). Abnormal vestibular tests were those that yielded the following results: deficient peripheral vestibular syndrome (DVPS), irritative peripheral vestibular syndrome (IVPS), including patients in which the only abnormality was a positive result to positioning tests, or the central vestibular syndrome (CVS).
RESULTS
Of 304 subjects enrolled in this study, 23% were aged between 41 and 50 years. The mean age of participants was 50.77 years.
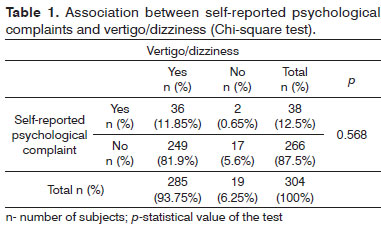
Female subjects comprised 72.7% of the sample. The complaint dizziness/vertigo was reported by 93.8% of the study sample; however, only 12.5% of subjects spontaneously reported psychological complaints. Table 1 shows that although 94.7% of subjects that spontaneously reported psychological complaints mentioned dizziness and/or vertigo, there was no significant association among these findings (p>0.05) (Table 1). Nineteen patients did not report dizziness/vertigo; they underwent vestibular testing because of other auditory complaints, such as tinnitus e hearing loss.
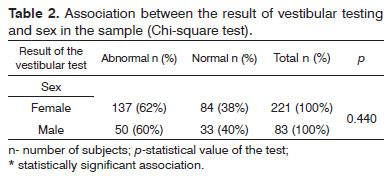
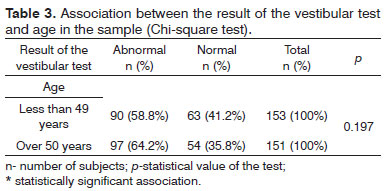
Of 304 subjects, 61.3% had abnormal vestibular tests. Table 2 shows the association between the result of vestibular testing and gender. The vestibular test was normal in 38% of females and 40% of males; there was no significant association between sex and test results (p>0.05). Ninety-seven of 187 subjects with abnormal vestibular test were aged over 50 years. Table 3 shows that there was no significant association between age and the results of vestibular testing (p>0.05).
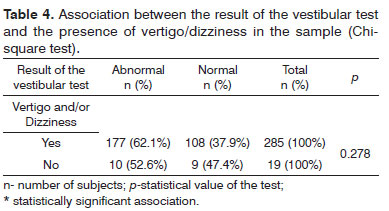
Of 285 subjects that reported dizziness and/or vertigo, 177 had abnormal vestibular tests and 108 tested normal. Again, there was no significant association between the presence of dizziness and/or vertigo and the result of the vestibular test (p>0.05) (Table 4).
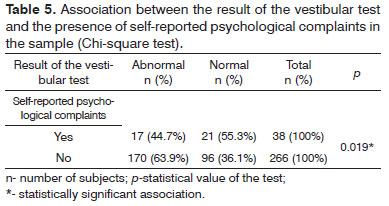
Table 5 shows that 55.3% of subjects that spontaneously reported psychological complaints had normal vestibular tests. In this case there was a significant association between the presence of self-reported psychological complaints and a normal vestibular test (p=0.019).
DISCUSSION
Studies that have related vestibular diseases with psychological complaints have noted that most such patients are aged from 41 to 50 years17-19; our data corroborates these findings. The estimated prevalence of balance disorders and vertigo comprises 5% to 10% of medical visits per year, and affect 40% of people aged more than 40 years20. There is a strong correlation between vertigo and psychological disorders among adults and elderly individuals3,21,22.
Other studies have shown that women are more susceptible to otoneurological conditions than men; our sample in which 72.7% were female was similar in this regard to previously published papers2,18,23. It is said that the prevalence of dizziness is higher in women, reaching a 2:1 ratio24. The presence of self-reported negative emotional states (especially stress) may be associated with changes of the dynamic balance in young adults, irrespective of sex and age25.
We found that 94.7% of subjects that spontaneously reported psychological symptoms also complained of dizziness and/or vertigo. Other published studies have shown that psychological symptoms occur together with vertigo and/or dizziness in 56.38% of subjects even when psychological symptoms are formally part of an evaluation protocol; in decreasing order they are anguish, anxiety, fear, depression, and memory disorders11. Psychic symptoms appear to be a current representation of past conflicts that were experienced traumatically and that may be reactivated, thereby explaining the onset of vertigo11.
A normal vestibular test associated with a complaint of dizziness and/or vertigo was seen in 37.9% of the sample. Normal results in the vestibular test together with complaints pertaining to the labyrinth may be understood when the vestibular apparatus is not affected or after it has recovered17.
We found a significant association between a normal vestibular test and self-reported psychological complaints in 55.3% of the study sample. If vestibular symptoms result from disorders in other organs, such as neurological conditions and/or psychological disorders, dizziness may occur without functional involvement of the vestibular system17, which may explain the normal tests. The vestibular system is unaltered in exclusively psychogenic vertigo; thus, results of VENG are normal. The diagnostic sensitivity of VENG should also be taken into account; its results may be normal in 40% with suspected labyrinth disorders26,27. Psychiatric conditions are frequent in patients with otoneurological complaints, especially anxiety disorders28. However, the presence of a psychiatric conditions does not exclude a balance disorder, which also applies inversely28. Psychological symptoms such as anxiety, depression, and fear, may be a cause or consequence of vertigo, or simply coexist with vertigo crises11,29. We found no published studies on associations between vestibular test results and self-reported psychological complaints. Balance disorders and complaints of dizziness are associated with high levels of anxiety30. The prevalence of anxiety disorders (especially panic and agoraphobia) among patients visiting specialized centers for the treatment of balance disorders is significantly higher than that in the general population30-33. Individuals with dizziness and vertigo due to vestibular disorders generally report somatic and psychic consequences, such as difficulty in concentrating, loss of memory, and fatigue. Physical insecurity because of dizziness and unbalance may result in psychic insecurity, irritability, loss of self-confidence, anxiety, depression or panic, a feeling of being out of touch with reality, and depersonalization19.
Mc Kenna et al.34 found that 42% of patients in outpatient otoneurology clinics (presenting with dizziness, tinnitus, and hearing loss) required psychological support. Jozefowicz-Korczynska et al.35 noted that psychological issues were often mentioned in the context of vestibular symptoms. Vestibular diseases may alter head and body alignment (patients attempt to avoid movements of the head or falls) and stability limits - the area within which individuals feel safer. There is often a mismatch between reality and the perception of stability limits in anxious individuals that fear falls; they may unnecessarily curtail their bodily movements36. in this context, anxiety and situational prevention approaches that characterize discomfort with movement may become a compensating strategy to avoid exposure to potentially dangerous situations7. The presence of vestibular dysfunction may cause a compensating increase in balance, and visual and proprioceptive sensitivity, which in turn may foster fear of heights and agoraphobia19.
One of the limitations of this study is that other factors not taken into account here may be related with vestibular disorders, such as use of medication (anti-inflammatory drugs, diuretics, chemotherapy, antibiotics, and psychotropic drugs), which may alter or injure the vestibular system and the cochlea; vertigo and dizziness may ensue, especially if drug dosages are high17. Metabolic, neurologic, cardiovascular, and degenerative conditions, infections and inflammation, trauma, otoneurologic symptoms (tinnitus and hypoacusis), and familial conditions, among others, may cause vertigo and/or dizziness35,37. We suggest that these issues be included in future studies. Additionally, further studies on the main psychological conditions manifesting jointly with vertigo in otoneurologic patients are needed11.
We still suggest a longitudinal study to assess the causal relationship between anxiety and vestibular symptoms; subjects may be monitored prospectively to evaluate the development of symptoms34. Depression should be investigated as a psychological condition associated with stress and dizziness, and should be taken into account in the diagnosis, therapy, and progression of otoneurologic patients12.
CONCLUSION
Age, sex, and the presence of absence of vertigo and/or dizziness in subjects of the study sample were not variables that had any influence on the results of vestibular testing. There was a statistically significant association between the presence of self-reported psychological complaints and normal vestibular tests. The results of VENG may be normal when vertigo is psychogenic only, as generally the vestibular system is not abnormal in these cases.
REFERENCES
1. Mor R, Garcia DMJ, Friedmann PSB. Análise comparativa das respostas vestibulares à prova calórica em pacientes submetidos ao exame vestibular sem e com o uso de medicação antivertiginosa. Arq Int Otorrinolaringol. 2006;10(1):22-7.
2. Bovolini A, Ganança CF, Ganança FF, Ganança MM, Caovilla HH. Prevalência de anormalidades às provas calóricas com água e com ar em vestibulopatias periféricas crônicas. ACTA ORL. 2007;25(2):165-9.
3. Moreira DA, Bohlsen YA, Momensohn-Santos TM, Cherubini AA. Estudo do Handicap em Pacientes com Queixa de Tontura, Associada ou Não ao Sintoma Zumbido. Arq Int Otorrinolaringol. 2006;10(4):270-7.
4. Ganança MM, Caovilla HH, Ganança FF, Doná F, Branco F, Paulino CA, et al. Vertigem. Rev Bras Med. 2008;65(12):614.
5. Handa PR, Kuhn AMB, Cunha F, Schaffleln R, Ganança FF. Qualidade de vida em pacientes com vertigem posicional paroxística benigna e/ou doença de Ménière. Rev Bras Otorrinolaringol. 2005;71(6):776-83.
6. Nishino LK, Granato L, Campos CAH. Aplicação do questionário de qualidade de vida diária em pacientes pré e pós-reabilitação vestibular. Arq Int Otorrinolaringol. 2008;12(4):517-22.
7. Balaban CD, Jacob RG. Background and history of the interface between anxiety and vertigo. J Anxiety Disord. 2001;15(1-2):27-51.
8. Ieto V, Cunha MC. Queixa, demanda e desejo na clínica fonoaudiológica: um estudo de caso clínico. Rev Soc Bras Fonoaudiol. 2007;12(4):329-34.
9. Flores MR, Franco ES. Vectoeletronistagmografia computadorizada: nistagmo póscalórico à estimulação com ar em indivíduos sem queixa. Arq Int Otorrinolaringol. 2003;7(4):302-8.
10. Tomaz A, Borges FN, Ganança CF, Campos CAH, Tilbery CP. Sinais e sintomas associados a alterações otoneurológicas diagnosticadas ao exame vestibular computadorizado em pacientes com esclerose múltipla. Arq Neuropsiquiatr. 2005;63(3B):837-42.
11. Paiva AD, Kuhn AMB. Sintomas psicológicos concomitantes à queixa de vertigem em 846 prontuários de pacientes otoneurológicos do Ambulatório de Otoneurologia da Universidade Federal de São Paulo Escola Paulista de Medicina. Rev Bras Otorrinolaringol. 2004;70(4):512-5.
12. Malagris LEN, Fiorito ACC. Avaliação do nível de stress de técnicos da área de saúde. Estud Psicol. (Campinas) [online]. 2006;23(4):391-8.
13. Sullivan M, Clark MR, Katon WJ, Russo J, Dobie RA, Voorhees R. Psychiatric and otologic diagnoses in patients complaining of dizziness. Arch Intern Med. 1994;154(5):590-4.
14. Batista MA e Oliveira SMSA. Sintomas de ansiedade mais comuns em adolescentes. Psic [online]. 2005;6(2):43-50.
15. Camelo SHH, Angerami ELS. Sintomas de estresse nos trabalhadores atuantes em cinco núcleos de saúde da família. Rev LatinoAm Enfermagem [online]. 2004;12(1):14-21.
16. Bardin L. Definição e relação com as outras ciências. In: Bardin L. Análise de conteúdo. Edição revista e actualizada. Lisboa: Edição 70; 2008. p.29-48.
17. Tiensoli LO, Couto ER, Mitre EI. Fatores associados à vertigem ou tontura em indivíduos com exame vestibular normal. Rev CEFAC. 2004;6(1):94-100.
18. Simoceli L, Bittar RMS, Bottino MA, Bento RF. Perfil diagnóstico do idoso portador de desequilíbrio corporal: resultados preliminares. Rev Bras Otorrinolaringol. 2003;69(6):772-7.
19. Ganança FF, Castro ASO, Branco FC, Natour J. Interferência da tontura na qualidade de vida de pacientes com síndrome vestibular periférica. Rev Bras Otorrinolaringol. 2004;70(1):94-101.
20. Koga KA, Resende BDA, Mor R. Estudo da prevalência de tontura/vertigens e das alterações vestibulares relacionadas à mudança de posição de cabeça por meio da vectoeletronistagmografia computadorizada. Rev CEFAC. 2004;6(2):197-202.
21. Yardley L, Owen N, Nazareth I, Luxon L. Prevalence and presentation of dizziness in a general practice community sample of working age people. Br J Gen Prac. 1998;48(429):1131-5.
22. Hallam RS, Stephens SDG. Vestibular disorder an emotional distress. J Psychossom Res. 1985;29(4):407-13.
23. Mantello EB, Moriguti JC, RodriguesJúnior AL, Ferrioli E. Vestibular rehabilitations effect over the quality of life of geriatric patients with labyrinth disease. Braz J Otorhinolaryngol. 2008;74(2):172-80.
24. Campos CAH. Principais quadros clínicos no adulto e no idoso In: Ganança MM. Vertigem tem cura? São Paulo: Lemos Editorial; 1998. p.49-58.
25. Cruz IBM, Barreto DCM, Fronza AB, Jung IEC, Krewer CC, Rocha MIUM, et al. Dynamic balance, lifestyle and emotional states in young adults. Braz J Otorhinolaryngol. 2010;76(3):392-8.
26. Bergano PS, Cabete CF, Gushikem P, Uehara I, Frazza MM, Caovilla HH, et al. Achados otoneurológicos em indivíduos com migrânea. Acta AWHO. 2000;19(2):88-95.
27. Silva MLG, Munhoz MSL, Ganança MM, Caovilla HH, editores. Quadros clínicos otoneurológicos mais comuns. São Paulo: Atheneu; 2000.
28. Furman JM, Jacob RG. A clinical taxonomy of dizziness and anxiety in the otoneurological setting. J Anxiety Disord. 2001;15(1-2):9-26.
29. Paulino CA, Prezotto AO, Calixto RF. Associação entre estresse, depressão e tontura: uma breve revisão. Rev Equilíbrio Corporal e Saúde. 2009;1(1):33-45
30. Yardley L, Redfern MS. Psychological factors influencing recovery from balance disorders. J Anxiety Disord. 2001;15(1-2):107-19.
31. Clark DB, Hirsch BE, Smith MG, Furman JMR, Jacob RG. Panic in otolaryngology patients presenting with dizziness or hearing loss. Am J Psychiatry. 1994;151(8):1223-5.
32. Frommberger VH, Tettenborn B, Buller R, Benkert O. Panic disorder in patients with dizziness. Arch Intern Med. 1994;154(5):590-1.
33. Stein MB, Asmundson GJG, Ireland D, Walker JR. Panic disorder in patients attending a clinic for vestibular disorders. Am J Psychiatry. 1994;151:697-700.
34. Mc Kenna L, Hallam RS, Hinchcliffe R. The prevalence of psychological disturbance in neurotology outpatients. Clin Otolaryngol. 1991;16(5):452-6.
35. Jozefowicz-Korczynska M, Ciechomska EA, Pajor AM. ENG outcome and neuropsychological findings in tinnitus patients. Archives of Sensology and Neurootology in Science and Practice-ASN. Proceedings of XXX Congress of the GNA-NES. Portugal; 2003.
36. Ganança FF. Vestibulopatias em crianças e adolescentes: principais quadros clínicos. In: Ganança MM, Vieira RM, Caovilla HH. Princípios de otoneurologia. São Paulo: Atheneu; 1999. p.57-62.
37. Teixeira AR, Nunes MGP, Freitas CR, Gonçalves AK, Teixeira SB. Análise da Qualidade de Vida de Idosos com Sintoma de Zumbido. Arq Int Otorrinolaringol. 2010;14(1):54-9.
1. Graduate level (Speech therapist, master's degree student in the Health Science Graduate Program, UFCSPA).
2. Graduate level (Speech therapist, UFCSPA).
3. Master's degree (Speech therapist, supervisor of the VIVAVOZ unit, UFCSPA).
4. Doctoral degree (Psychologist, adjunct professor, UFCSPA).
5. Doctoral degree (Speech therapist, adjunct professor, Speech Therapy Department, UFCSPA ).
6. Doctoral degree (Psychologist, adjunct professor, UFCSPA. Productivity bursary, CNPq).
7. Master's degree (Speech therapist, assistant professor, Speech Therapy Department, UFCSPA, doctoral student in biomedical gerontology, IGG/ PUCRS. ).
Porto Alegre Federal University - Health Science.
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on February 13, 2011.
Accepted on August 16, 2011. cod. 7574