Year: 2012 Vol. 78 Ed. 1 - (9º)
Artigo Original
Pages: 57 to 61
Risk factors for incidental parathyroidectomy during thyroidectomy
Author(s): Niklas Söderberg Campos1; Lívia Petrone Cardoso1; Ricardo Tirapelli Tanios1; Bruna Craveiro de Oliveira1; André Vicente Guimarães2; Rogério Aparecido Dedivitis3; Luiz Francisco Marcopito4
Keywords: parathyroid glands, thyroid neoplasms, thyroidectomy.
Abstract:
Incidental parathyroidectomy is a common event in thyroid surgery. The literature shows a finding of parathyroid glands ranging from 6.4% to 31% in pathological specimens of the thyroid gland.
OBJECTIVE: To collect the amount of parathyroid glands found in surgical specimens of thyroidectomy and correlate with the histopathological and demographic variables.
METHODS: Retrospective study based on pathological reports of thyroidectomy from January 2007 to December 2008.
RESULTS: 442 patients were submitted to total thyroidectomy, and 2.93% had parathyroid glands, which corresponded to 13 of this total. The presence of papillary thyroid carcinoma associated with incidental parathyroidectomy was 10.11%, compared to the benign lesion: 1.4%.
CONCLUSION: Papillary thyroid carcinoma was the variable associated with increased number of incidental parathyroidectomy.
![]()
INTRODUCTION
Accidental parathyroidectomy is a frequent occurrence during thyroidectomies. Some studies have assessed the incidence rates of accidental parathyroidectomies, which vary between 6.4% and 31.0%1-7. Most of the times, there are four parathyroid glands. Nonetheless, this number may vary, fluctuating between two and 192. The most commonly location is subcapsulary1-7. These glands develop from the third and fourth pairs of embryonic pharyngeal pockets, and its histology is made up mainly of oxyphil and parathyroid cells3. The parathyroid gland vascularization stems from branches of the upper and lower thyroidea arteries4-5. During surgery, it is essential to handle it with care, so as to preserve the vascularization of the parathyroid glands3.
The rate of complications, such as hematomas, infection, keloid and damage to the recurrent laryngeal nerve during thyroidectomies is 5%8,9. The two most common complications are described in decreasing order, such as recurrent laryngeal nerve damage and hypocalcemia1-7.
The goal of the present paper is to identify the risk variables concerning the accidental removal of the parathyroid glands during thyroidectomy.
METHODS
The present study was approved by the Ethics in Research Committee of the Institution where it was designed, under protocol # 013/2010.
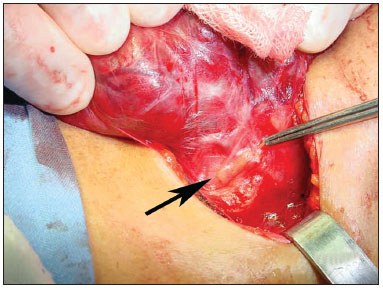
We carried out a retrospective study, in which we used 442 charts between January of 2007 and December of 2008. We assessed the demographic variables: age and gender; and the histopathological ones (thyroiditis, histopathology diagnosis, specimen weight, size in its longest axis and the presence of concurrent neck dissection). During the surgical procedure, we systematically tried to identify the parathyroid glands in the surgical field (Figure 1) and in the resected specimen.
Figure 1.Extracapsular identification of the thyroid gland in the operating field.
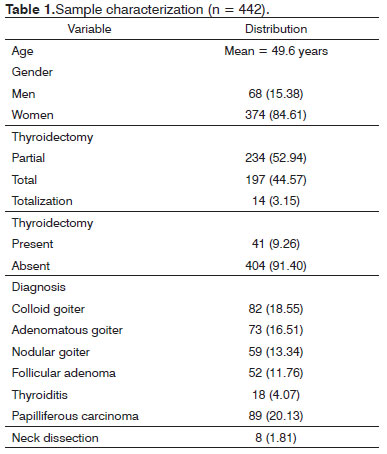
According to Table 1, we had a predominance of women (5.5 times more) among patients submitted to thyroidectomy. In relation to the type of procedure to which the patients were submitted to, partial thyroidectomy came in first place - with the largest number of cases, followed by total and, afterwards, totalization. Approximately 10% had thyroiditis. The final diagnosis of the specimen submitted to histopathology varied from colloid goiter - found in greater number, all the way to thyroiditis. Papilliferous carcinoma was present in approximately 20% of the cases. We did recurrent neck dissection in about 2% of the thyroidectomized patients.
RESULTS
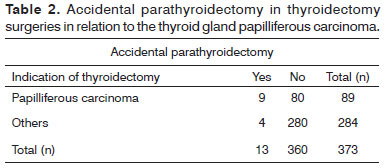
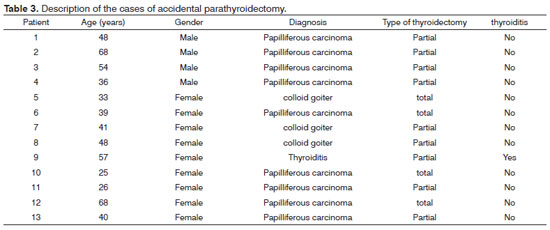
The total number of thyroidectomized patients was 442, and parathyroid glands were found in 13 of these, corresponding to 2.93% of all thyroidectomized patients who took part in the study. When broken down by gender, there were 68 males, with four cases of parathyroid glands found in the surgical specimens and, when we calculated the percentage, it resulted in 0.9% - results which were lower than those in the second group - with 9 cases from a total of 374 patients - 2.03%. The general incidence of accidental parathyroidectomies in elective thyroidectomies was 3.5% (13 in 373). Nonetheless, it reached 10.1% (nine in 89) when the indication for thyroidectomy corresponded to papilliferous carcinoma, and when compared to the other indications, which added to 1.4% (four in 284), its association was much more probable. Thus, variables such as: gender, age, having thyroiditis or not and the type of procedure carried out did not influence the finding of accidental PG in surgical specimens. For statistical purposes, we used the bicaudal Fisher's test in order to calculate the likelihood of an association between accidental parathyroidectomies and the TG papilliferous carcinoma being true. It yielded a very low probability (p = 0.0005) of such difference in percentage (10.1 versus 1.4) having occurred by chance.
As far as the topographic distribution of the parathyroid glands found in surgical specimens is concerned, results showed seven (2.93%) cases in the gland's extracapsular region, five (1.13%) in the subcapsular region and one (0.22) in the intraglandular region.
The presence of thyroid papilliferous carcinoma associated with accidental parathyroidectomy was 10.11%; compared to 1.4% of benign disease - Tables 2 and 3.
DISCUSSION
Thyroidectomy is a relatively safe surgical procedure, and its main complications include injury to the parathyroids, potentially manifested by temporary or permanent hypocalcemia4.
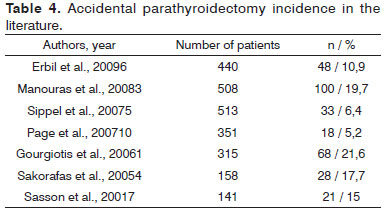
Accidental parathyroidectomy is a frequent finding, even in experienced hands. Since the XIX century, thyroid surgeries have had a reduction in the incidence of complications9. Following the literature, the incidence of accidental parathyroidectomy varies between 5.2% and 31% during thyroidectomies1-10 - Table 4. Nonetheless, surgeon experience in thyroid surgery has been a determining factor in the better identification and preservation of parathyroid glands during thyroidectomy8, minimizing such complication. Although in our clinic the surgical team is made up of residents and surgeons with 4 to 12 years of practice, our results concerning accidental parathyroidectomy was of only 2.93%.
Familiarity with the parathyroid anatomy and its blood supply system is necessary to prevent inadvertently injuring it, devascularization or resection of parathyroid parenchyma11. The variability in its location may contribute to the risk of accidental avulsion.
Most parathyroid glands have extracapsular location1-10, which enables its identification and preservation. 49% of the glands have been found inside the thyroid and, in such cases, it is impossible to spare it3.
Some authors advocate the systematic identification of the glands in the surgical field12, while others believe that the juxta-capsular dissection of the thyroid with the ligature of small vessels to be the best way to see the parathyroids and their blood supply10. Special care must be taken near the upper parathyroid, which is frequently located near the recurrent laryngeal nerve as it enters the lower thyroidea artery10.
The most relevant risk factor was the presence of thyroid papilliferous carcinoma (10.11%) against the presence of benign disease (1.4%). One possible explanation for this finding would be the need to increase the oncologic surgical margin and, sometimes, including a probable metastatic lymph node in the surgical specimen. Theoretically, the risk of accidental parathyroidectomy may increase in some situations, such as in patients submitted to extensive surgery by malignant disease, in the presence of extra-thyroid extension, or in the presence of a large lymph node metastasis in the surgical specimen. In this direction, modified radical neck dissection has been recognized as a risk factor7. Special attention when doing the dissection in the neck central compartment may reduce the risk of such complication; nonetheless, oncological procedures must not be compromised.
Thyroidectomy totalization and reoperations have been correlated with the increase in the rates of accidental parathyroidectomies, probably as a result of fibrosis, which may cause operatory difficulty. Thyroiditis may also have been described as another risk factor13.
A careful inspection of the surgical specimen in search of the normal parathyroid gland tissue is prudent, and it may lead to auto-transplant. Such practice must be routine, especially when more than two glands are identified in these conditions, or when the preservation of vascularization of the other glands is questionable. Routine auto-transplant results in less than 1% incidence of permanent hypoparathyroidism14,15. In fact, the impact on the serum levels of calcium will be lower when only one gland is resected, and the others are preserved10. The surgical field must also be carefully assessed, with the aim of certifying the feasibility of the preserved glands. Auto-transplant is also indicated in cases of persistent isquemia10.
CONCLUSION
Papilliferous carcinoma was the variable associated with accidental parathyroidectomy.
REFERENCES
1. Gourgiotis S, Moustafellos P, Dimopoulos N, Papaxoinis G, Baratsis S, Hadjiyannakis E. Inadvertent parathyroidectomy during thyroid surgery: the incidence of a complication of thyroidectomy. Langenbecks Arch Surg. 2006;391(6):557-60.
2. Ondik MP, McGinn J, Ruggiero F, Goldenberg D. Unintentional parathyroidectomy and hypoparathyroidism in secondary central compartment surgery for thyroid cancer. Head Neck. 2010;32(4):462-6.
3. Manouras A, Markogiannakis H, Lagoudianakis E, Antonakis P, Genetzakis M, Papadima A, et al. Unintentional parathyroidectomy during total thyroidectomy. Head Neck. 2008;30(4):497-502.
4. Sakorafas GH, Stafyla V, Bramis C, Kotsifopoulos N, Kolettis T, Kassaras G. Incidental parathyroidectomy during thyroid surgery: an underappreciated complication of thyroidectomy. World J Surg. 2005;29(12):1539-43.
5. ippel RS, Ozgül O, Hartig GK, Mack EA, Chen H. Risks and consequences of incidental parathyroidectomy during thyroid resection. ANZ J Surg. 2007;77(1-2):33-6.
6. Erbil Y, Barbaros U, Ozbey N, Aral F, Ozarmagan S. Risk factors of incidental parathyroidectomy after thyroidectomy for benign thyroid disorders. Int J Surg. 2009;7(1):58-61.
7. Sasson AR, Pingpank JF Jr, Wetherington RW, Hanlon AL, Ridge JA. Incidental parathyroidectomy during thyroid surgery does not cause transient symptomatic hypocalcemia. Arch Otolaryngol Head Neck Surg. 2001;127(3):304-8.
8. Bergamaschi R, Becouarn G, Ronceray J, Arnaud JP. Morbidity of thyroid surgery. Am J Surg. 1998;176(1):71-5.
9. Udelsman R, Chen H. The current management of thyroid cancer. Adv Surg. 1999;33(1):1-27.
10. Page C, Strunski V. Parathyroid risk in total thyroidectomy for bilateral, benign, multinodular goitre: report of 351 surgical cases. J Laryngol Otol. 2007;121(3):237-41.
11. Loré JM Jr, Pruet CW. Retrieval of the parathyroid glands during thyroidectomy. Head Neck Surg. 1983;5(3):268-9.
12. Coudray C, Lienhardt PY, Conradi A, Seghir A, Dero M, Beurier C, et al. Lhypoparathyroidie apres la chirurgie thyroidienne. Ann Otolaryngol Chir Cervicofac. 1994;111(4):189-95.
13. Lin DT, Patel SG, Shaha AR, Singh B, Shah JP. Incidence of inadvertent parathyroid removal during thyroidectomy. Laryngoscope. 2002;112(4):608-11.
14. Walker RP, Paloyan E, Kelley TF, Gopalsami C, Jarosz H. Parathyroid autotransplantation in patients undergoing a total thyroidectomy: a review of 261 patients. Otolaryngol Head Neck Surg. 1994;111(3 Pt 1):258-64.
15. Olson JA Jr, DeBenedetti MK, Baumann DS, Wells SA Jr. Parathyroid autotransplantation during thyroidectomy. Results of long-term follow-up. Ann Surg. 1996;223(5):472-8.
1. Medical Student - Medical School of the Metropolitan University of Santos - UNIMES, Santos/SP, Brazil.
2. PhD in Medicine - Graduate Program in Surgery - Medical School of the University of São Paulo- USP. (Professor of Otorhinolaryngology and Head and Neck Surgery - Metropolitan University of Santos, Santos/SP, Brazil).
3. MD. Senior Associate Professor - Fundação Lusíada UNILUS.
4. Senior Associate Professor - Federal University of São Paulo - UNIFESP, São Paulo. (Full Professor of Collective Health at the Metropolitan University of Santos - UNIMES, Santos).
Departments of Otorhinolaryngology and Head and Neck Surgery and Scientific Initiation of the Metropolitan University of Santos - UNIMES, Santos/SP, Brazil.
Send correspondence to:
André Vicente Guimarães
Rua Dr. Olinto Rodrigues Dantas, 343 conj. 92
Zip Code:11050-220. Santos - SP, Brazil
E-mail: guimaraesav@uol.com.br
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on April 17, 2011.
Accepted on June 12, 2011. cod. 7711