Year: 2010 Vol. 76 Ed. 5 - (14º)
Artigo Original
Pages: 618 to 622
Prognostic value of sinus CT scans in hematopoietic stem cell transplantation
Author(s): Erica Ortiz1, Érika Nakamura2, Rodrigo Magalhães3, Cármino Antonio de Souza4, Carlos Takahiro Chone5, Afonso Celso Vigorito6, Eulalia Sakano7
Keywords: sinusitis, x-ray computed, tomography scanners.
Abstract:
Hematopoietic Stem Cell Transplant (HSCT) causes immunosuppression and predisposition to sinusitis. CT scans are complementary exams used in the diagnosis of sinusitis; however, its use in every patient is questionable. Aim: to check the usefulness of ordering a CT scan prior to HSCT and to study the relationship between anatomical variations and sinusitis. Method: prospective study in which we performed paranasal CT scans before and after HSCT, using the Lund and Mackay score. Results: 77.5% and 61% of CT scans showed no evidence of sinus disease before and after HSCT. CT staging was not associated with sinusitis after HSCT. Anatomical variations were related to radiographic disease severity, but not to development of sinusitis after HSCT. There was no relation between pre-CT staging and sinusitis after BMT. Conclusion: CT scans are not useful for all patients before HSCT. Anatomical variation is not a predictive feature to sinusitis but it can determine its severity.
![]()
INTRODUCTION
Hematopoietic stem-cell transplantation (HSCT) is a reality in tertiary hospitals at present. The number of transplants has increased gradually in Brazil during the past six years; over seven thousand transplants were carried out during this period. The number of HSCT in 2008 increased by 37% according to the National Transplant Unit of the Brazilian Ministry of Health.1
HSCT patients are previously immunosuppressed because of whole body chemotherapy or radiotherapy. They therefore are at a higher risk for viral, bacterial or fungal infection, in particular upper airway infections, because of direct contact with the environment.2-7 Other complicating factors for respiratory infection are prolonged hospital stay, graft versus host disease, and corticosteroid therapy.2-7 These patients have a 37% risk for developing rhinosinusitis after transplantation, compared to a 15% rate in patients with normal immune status.3,8
Several laboratory tests are required by the hematology unit before HSCT, including paranasal sinus radiography, done in all patients to investigate possible sinus disease. Some authors advocate doing computed tomography of the paranasal sinuses before transplantation in all patients, aiming at avoiding post-HSCT rhinosinusitis because of immunosuppression.5,7,9,10
According to the Brazilian rhinosinusitis guidelines, the diagnosis of this condition is not based only on paranasal sinus radiograms, which is insufficiently specific (79%) or sensitive (76%).11,12 At present, recommendations include a detailed clinical history and physical examination, and nasal endoscopy, which jointly enable a diagnosis of rhinosinusitis. Paranasal sinus computed tomography (CT) is done only if symptoms persist after treatment, or if the disease recurs or complicates.12 Thus, the physical examination and nasal endoscopy are effective for assessing patients before HSCT. However, some authors have defended carrying out paranasal sinus CT in all patients before HSCT, arguing that signs suggesting rhinosinusitis in this exam - and their intensity - are effective prognostic factors.5,6,7,9,10
Carrying out CT in all patients before transplantation may increase costs and the preparation time, as radiology units are under great demand for routine exams. Thus, the purpose of this study was to verify the need for paranasal sinus CT in all patients before HSCT and the relation between tomography findings of prior nasosinusal disease and the development of rhinosinusitis after HSCT.
METHOD
A prospective pilot study was carried out in the Rhinology Unit of the Otorhinolaryngology Discipline. The institutional review board approved the study (protocol no. 088-2002). Thirty-one HSCT patients from the Bone Marrow Transplant Unit (2003-2004) were assessed. All patients underwent a clinical evaluation, nasal endoscopy, and paranasal sinus CT before and after HSCT. No patient had undergone nasal surgery before.
Patients with predisposing factors such as smoking, asthma, and nasal polyposis were excluded, as were patients in which CT was not done before or after transplantation.
The criteria of the Brazilian rhinosinusitis guidelines (2008) were applied.12 Accordingly, rhinosinusitis is characterized by nasal block, coughing, fever, facial pain, rhinorrhea with discharge, a purulent discharge in the middle meatus and/or sphenoethmoidal recess upon the nasal endoscopy, and/or sinus opacification on paranasal sinus CT.12
Anatomical changes were evaluated on CT (septal deviation, an altered unciform process, a bullous middle turbinate, a paradoxal middle turbinate, Haller cells), as were signs of rhinosinusitis (partial or complete opacification of paranasal sinuses).13-15 The Lund and Mackay classification was applied for the CT staging of rhinosinusitis.13 In this approach, each paranasal sinus is scored from 0 to 2 depending on the degree of opacification. Absence of changes is scored 0, partial opacification is scored 1, and complete opacifiation is scored 2. The osteomeatal complex is also scored depending on the degree of obstruction; no obstruction is scored 0, and obstruction is scored 2. Thus, a higher score corresponds to increased severity of rhinosinusitis - paranasal sinuses are more affected. The total scores ranged from 0 to 24 points for the right and left sides.
The relation between anatomical changes and/or CT staging and the development of post-HSCT rhinosinusitis was analyzed. Fisher's test was applied in the statistical analysis of data.
RESULTS
The sample for analysis comprised 31 HSCT patients - predominantly allogenic bone marrow transplants (90%). There were 19 females (61%) and 12 males (39%). The mean follow-up time for these patients was 12 months.
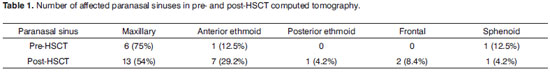
A pre-HSCT clinical diagnosis of rhinosinusitis was made in five patients (16.1%); this same diagnosis was made post-HSCT in 10 patients (32.2%), The maxillary sinus was the most frequent site, followed by the anterior ethmoid sinus (Table 1).
Only seven patients (22.5%) had prior CT staging over 1 for rhinosinusitis before HSCT; the same score was found in 12 patients (39%) after HSCT. Thus, 77.5% of CTs were within normal limits before bone marrow transplantation, and 61% were within normal limits after HSCT. Two (29%) of seven patients with positive rhinosinusitis staging before HSCT had no changes on CT after HSCT; two patients (29%) remained with the same staging score, and three patients (42%) had a worse score. Among patients with post-transplant rhinosinusitis, six (50%) had a CT stage over 2, without any change in the pre-HSCT CT.
Only six patients (19.4%) had anatomical changes or variants in the nasal cavity and/or paranasal sinuses, including septal deviation (3), bullous middle turbinate (3), and Haller cells (1).
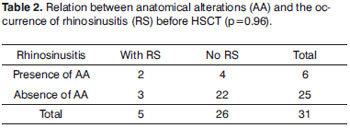
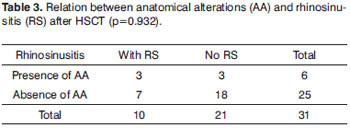
Nasal and/or paranasal sinus anatomical variants were not associated significantly with a higher occurrence of pre- or post-HSCT rhinosinusitis (Table 2 and 3).
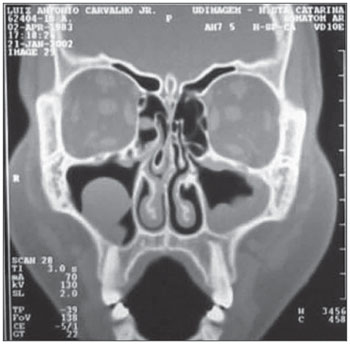
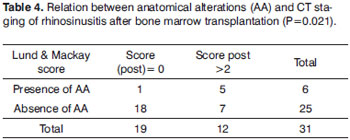
Anatomical changes were significantly associated with a higher post-transplant CT staging score for post-transplant rhinosinusitis (>2), which may be considered a complicating factor for post-transplant middle meati block (Fig. 1). Most of the group with anatomical changes - in relation to osteometal complex block - had a CT staging score of (Table 4).
Figure 1. Paranasal sinus comupted tomography showing anatomical variants in a HSCT patient: bullous turbinate and septal deviation.
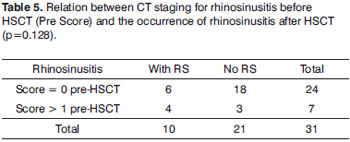
The association between CT staging of paranasal sinuses before transplantation and rhinosinusitis after bone marrow transplantation was not significant (Table 5).
DISCUSSION
A higher rate of post-HSCT rhinosinusitis is due to immunosuppression and to other aggravating factors such as prior chemotherapy and radiotherapy, viral infections, or graft versus host disease.2-7 The published estimated rate of rhinosinusitis in transplant patients is 36.9%.3 The rate found in our study (32.2%) was roughly close to this estimate.
Notwithstanding the small number of patients in our study, a normal CT exam before HSCT was rather higher (77%) compared to other published results (51-48%).5,6,9 Half of the patients in this study that presented post-HSCT rhinosinusitis had no prior CT findings or any clinical diagnosis of this condition. About 57% of patients with pre-transplantation CT findings had post-transplant rhinosinusitis, although there was not a significant correlation. Thompson et al.'s retrospective study also found no correlation between pre-transplantation CT findings and nasosinusal symptoms and post-transplant rhinosinusitis.6 Although this author's study had a larger sample - 100 pre-transplant patients during a 10-year period - only 64 post-HSCT paranasal sinus CTs were available for study.6 Shaw et al. studied 26 patients and correlated positive pre-transplantation CT findings with post-transplantation rhinosinusitis.5 The percentage rate of worsening of rhinosinusitis after bone marrow transplantation in previously affected patients (42%) was lower than that of Billings et al. (66.7%).9 Such differing results may be explained by the age range of study groups; the sample comprised only adults in Thompson's and our studies, and only children in Billings and Shaw's study. Thompson further explains this difference as due to pre-HSCT treatment of nasosinusal diseases; this was not clear in Billings and Shaw's study. All patients in the present study were treated before transplantation if they presented nasosinusal diseases.
Calculating the sample size was unnecessary, as this was a prospective pilot study to check the feasibility of carrying out paranasal sinus CT in all transplant candidates. Furthermore, the literature has no similar prospective studies corroborating CT before HSCT.
Most HSCT studies have small samples because of the paucity of transplantations. Thus, a large sample is only possible in multicentric studies. Within our study period (2003 to 2004) there were 79 allogenic HSCTs at the Bone Marrow Transplantation Unit, Hemocentro/HC-UNICAMP. The mean annual allogenic transplantation rate at our Unit from 2002 to 2004 was 40 transplants.
A lack of correlation between anatomical variants and the occurrence of rhinosinusitis before and after transplantation is in line with published studies on chronic rhinosinusitis in patients with a normal immune status.14,15 Thus, surgery before HSCT in patients with anatomical variants to prevent post-transplantation rhinosinusitis is not indicated. There was, however, a correlation between anatomical variants and post-HSCT worsening of rhinosinusitis. Larger samples may clarify this correlation.
Paranasal sinus CT in all HSCT-treated patients appears to be unnecessary because no significant correlation was found between positive nasosinusal CT findings and the occurrence of post-transplantation rhinosinusitis. A few authors have suggested carrying out paranasal sinus CT before transplantation in all patients, arguing that the severity of CT findings before HSCT would correlate with the occurrence of rhinosinusitis after HSCT.5,9
Paranasal sinus CT might be done only in HSCT candidates with clinical and endoscopic findings suggesting rhinosinusal disease.
CONCLUSION
Although the sample was small, given the paucity of transplants, paranasal sinus CT before HSCT appears not to be necessary in all patients; the exception is evidence of anterior nasosinusal disease.
Rhinosinusitis demonstrated in pre-transplant CT showing altered sinuses, as seen in this study, may be related with worsening of the rhinosinusitis after transplantation. Nasosinusal anatomical variants appear to be associated with more severe rhinosinusitis after bone marrow transplantation.
REFERENCES
1. HEMO em Revista, 2008; SNT (Serviço Nacional de Transplante).
2. Ricardo Pasquini. Fundamentos e Biologia do Transplante de Células Hematopoiéticas - Fundamentos em Hematologia, capitulo 81. p.913-934
3. Savage DG: Taylor P; Blackwell J; Chen F; Szydlo RM; Rule SAJ; Spencer A; et al. Paranasal sinusitis following allogenic bone marrow transplant - Bone Marrow Transplant. 1997;19:55-9.
4. Belinger N; Sinusitis in Immunodeficient and immunosuppressed patients. Laryngoscope. 1985;95:29-33.
5. Shaw GY, Panje WR, Corey JP. Risk factors in the development of acute sinusitis in immunocompromised patients.Am J Rhinol. 1991;5:103-8.
6. AM Thompson, M Couch, ML Zahurak1, C Johnson, GB Vogelsang. Infections post transplant - Risk factors for post-stem cell transplant sinusitis. Bone Marrow Transplant. 2002;29,257-61
7. Mirza N; Montone KT; Stadtmauer EA; Lanza DC. A schematic approach to preexisting sinus disease for the imunocompromised individual. Am J Rhinology. 1998;12:93-8.
8. Anselmo-Lima WT. Estudo da regeneração da mucosa do seio maxilar pós-cirurgia endoscópica. Tese de livre docência - USP RIBEIRÃO PRETO, 2001.
9. Billings KR, Lowe LH, Aquino VM, Biavati MJ. Screeening Sinus CT scans in pediatric bone marrow transplant patients.Int J Pediatr Otorhinolaryngol. 2000;52(3):253-60.
10. Mirza N; Lanza DC; Diagnosis and Management of Rhinosinusitis before Schedule Immunosuppression.Otolaryngol Clin North Am. 2000;33(2):313-21
11. Lanza DC; Kennedy DW. Adult rhinosinusitis defined. Otolaryngol Head Neck Surg. 1997;117:51-7.
12. Diretrizes Brasileiras de Rinossinusites. Braz J Otorhinolaryngol. 2008;74(2), supl.
13. Lund VJ; Mackay IS. Staging in rhinosinusitis. Rhinology. 1993;31:183-4.
14. Nassar Filho J. ; Anselmo-Lima WT.; Santos AC. Participação das Variações anatômicas do complexo ostiomeatal na gênese da rinossinusite crônica analisadas por tomografia computadorizada. Rev Bras Otorrinolaringol. 2001;67(4):489-95.
15. Voegels RL. ; Goto EY. ; Chung D. ; Nita LM. ; Lessa MM. ; Botugan O.Correlação Etiológica entre variações anatômicas na Tomografia Computadorizada e a Rinossinusite Crônica. Rev Bras Otorrinolaringol. 2001;67(4):507-10.
1. Physician, ENT specialist, master's degree in medical sciences - otorhinolaryngology at the FCM-UNICAMP. Collaborating otorhinolaryngologist in the Rhinology Unit, FCM-UNICAMP.
2. Physician, ENT specialist, resident in the Otorhinolaryngology Discipline, UNICAMP.
3. Medical resident, Otorhinolaryngology Discipline, UNICAMP. Otorhinolaryngologist.
4. Full professor at the Hemocentro, UNICAMP, and bone marrow transplantation at the HC-UNICAMP.
5. Professor Doutor, Head & Neck Surgery Otorhinolaryngology Discipline, UNICAMP.
6. Doctorate in hematology, medical hematologist and supervisor of the Bone Marrow Transplant Unit, Hemocentro/HC-Unicamp.
7. Doctorate in medical sciences - otorhinolaryngology. Physician of the Rhinology Unit, Otorhinolaryngology Discipline, FCM-UNICAMP.
Otorhinolaryngology - Head & Neck Discipline/Rhinology Unit, Hospital das Clínicas - UNICAMP
Send correspondence to:
Dra. Érica Ortiz
Disciplina de Otorrinolaringologia, Cabeça e Pescoço - Faculdade de Ciências Médicas/UNICAMP
Caixa Postal 6111 Campinas SP 13093-970
Phone: (0xx19) 3788-7523 - Fax: (0xx19) 3788-8763
E-mail: erica.ortiz@terra.com.br
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on October 18, 2009
and accepted on July 22, 2010. cod. 6717