Year: 2010 Vol. 76 Ed. 5 - (3º)
Artigo Original
Pages: 552 to 556
Obstructive sleep apnea syndrome (OSAS) in mouth breathing children
Author(s): Suemy Cioffi Izu1, Caroline Harumi Itamoto2, Márcia Pradella-Hallinan3, Gilberto Ulson Pizarro4, Sérgio Tufik5, Shirley Pignatari6, Reginaldo Raimundo Fujita7
Keywords: sleep apnea, children, polysomnography, prevalence, mouth breathing, snoring.
Abstract:
It is well known that mouth breathing is associated with adenotonsillar hypertrophy - which is the main cause of obstructive sleep apnea among children. Despite the importance of this matter, there are only a handful of studies showing the relationship between OSAS and mouth breathing. Aim: to determine the prevalence of obstructive sleep disorders in mouth breathing children and study its correlation with otorhinolaryngological findings. Study design: Retrospective cohort study. Method: Data analysis from 248 medical charts of mouth breathing children seen at the Pediatric Otolaryngologic Division of a large medical institution between the years of 2000 and 2006. All patients had nasofibroscopy and or Cavum radiographs and polysomnographic exams. According to the Apnea index, patients were classified as primary snorers (AI<1); and as OSAS (AIIA>11). Results: From 248 patients included in the study, 144 (58%) were primary snorers and 104 (42%) had OSAS. The most prevalent otorhinolaryngological findings were adenotonsillar hypertrophy (n=152; 61.2%), tonsilar hypertrophy (n=17; 6.8%), adenoid hypertrophy (n=37; 14.9%), rhinitis (n=155; 62.5%) and secretory otitis (n=36; 14.5%). Conclusions: primary snoring and OSAS are frequent findings in mouth breathing children. The most frequent otorhinolaryngological disorder in children with OSAS is adenotonsillar hypertrophy with or without rhinitis.
![]()
INTRODUCTION
Snoring and oral breathing are frequent complaints which make the parents of children with these symptoms to take them to otorhinolaryngologists. The prevalence of habitual snoring in children between 3 and 13 years varies between 5.2 and 34.45%1-4, while the prevalence of oral breathing is of 26.8% according to a large study with 661 children aged between 6 and 12 years5.
Chronic mouth breathing in children is usually associated with palatine and pharyngeal tonsils hypertrophy,4 with or without allergic rhinitis. Its incidence peak happens in pre-school aged children6,7. At this stage, besides the natural growth of the soft palate and pharyngeal tonsils, there are repetition infections which cause tonsillar lymphoid tissue hypertrophy, changing the breathing of children to a chronic obstructive pattern. A consequence of this in the long run has been craniofacial changes8 which maintain the mouth breathing pattern, besides causing postural9 and hearing10 disorders. Among mouth breathers, it is also common to find the Obstructive Sleep Apnea Syndrome (OSAS)11,12, a potentially severe clinical situation, as well as primary snoring.
Primary snoring is noise produced by breathing, caused when air passes through the upper airway without, however, causing changes to sleep, alveolar ventilation and oxygenated hemoglobin saturation. It is common during childhood, happening from 7 to 10% of the children between 1 and 10 years17 . Obstructive Sleep Apnea Syndrome (OSAS) in children is a disease characterized by partial prolonged and/or complete obstruction of the upper airways, impairing normal ventilation. The signs and symptoms of this syndrome include the common snoring, interrupted sleep, neurocognitive and behavioral disorders such as learning disorders13,14, behavioral changes, attention deficit and hyperactivity13,14. The major complications of the OSAS include growth and development delays15, mental retardation15 and cor pulmonale16 . The gold standard test used to diagnose OSAS is Polysomnography18, since it enables us to differentiate OSAS from primary snoring19. Its high cost and difficulty in performance in children are, however, important limitations and also reasons to explain why only a few centers can count on this exam for most of its patients.
Given the importance of OSAS in children and the scarcity of studies correlating this disease to mouth breathing in children, we designed this study with the goal of determining OSAS prevalence in mouth breathing children and check its correlation with otorhinolaryngological findings.
METHOD
The data was obtained from the charts of patients who visited the pediatric otorhinolaryngology ward of a teaching hospital between 2000 and 2006. In the study we included children with ages ranging between 0 and 13 years, diagnosed by an multidisciplinary team (otorhinolaryngologists, allergists, speech and hearing therapists, orthodontists, physical therapists) as mouth breathers, using the criteria of preferentially oral breathing for more than 6 months and physical exam showing two or more signs of oral breathing (nasal obstruction, deep hard palate, maxillary atresia, open mouth, mouth muscle laxity, bite changes, posture changes and anterior flexion of the head).
Children diagnosed as mouth breathers were submitted to sleep disorder investigation by means of nocturnal polysomnography under the following protocol: in a dark and silent room and with the child's guardian present. The electrophysiological and cardio-respiratory parameters were recorded in a computerized system (Alice 3 Healthdyne/respironics, Marrieta, GA), using EEG data ( C3/A2, C4/A2, O1/A2, O2A1), submentonian and tibial electromyogram, right and left side electro-oculogram, oronasal airflow, chest and abdominal movement, laryngeal microphone (snoring), oxyhemoglobin saturation (SaO2) and position on the bed. The test was analyzed by a physician with experience with the pediatric population and it is classified according to criteria from the American Thoracic Society (1995).
We excluded those children with genetic syndromes, metabolic disorders, neurologic diseases or congenital malformations.
From each chart we analyzed the following information: gender, age at the time of the polysomnography, ENT diagnosis and polysomnographic diagnosis, hypopnea/apnea ratio (HAR) and the rate of oxygen saturation (satO2).
According to the "American Thoracic Society"19, we consider the following:
- Hypopnea/apnea index (HAI): number of obstructive and mixed apnea episodes in a minimum time span of two respiratory cycles (expressed in episodes/hour). OSAS is diagnosed in children with AI>1 / hour.
- O2 Saturation Nadir: minimum oxygen saturation during the sleep study. Values below 90% are associated with central or obstructive sleep ventilatory disorders.
The otorhinolaryngological diagnoses of each child were based on the initial otorhinolaryngological evaluation, including nasal-fibroscopy.
The data was grouped according to the results from polysomnography tests and all classifications were based on the HAI and O2 Saturation Nadir values.
The individuals were broken down into primary snorers when they had HAI < 1, and those with OSAS, when the AI was > 1. The children with OSAS were further divided into mild (1 < HAI< 5), moderate (5 < HAI < 10) and severe (HAI > 10)20OSAS. Within each subgroup, there was also one more division, according to the degree of O2 desaturation, considering the nadir (minimum level of O2 saturation). Thus, we considered four subgroups: Nadir = 80; 80 < Nadir = 85; 85 < Nadir = 90 e Nadir = 90. The data obtained was associated with patient age and gender and the findings from the evaluation and otorhinolaryngological exams.
The patients signed the free and informed consent form approved by the Ethics in Research Committee of the Federal University of São Paulo Medical School - Unifesp-EPM, protocol 171/06 approved on February 10, 2006.
For the statistical analysis we used the Chi-squared28 test.
RESULTS
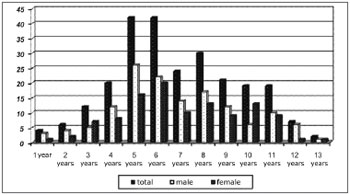
The final sample comprised 248 patients. Among them, 144 (58%) had primary snoring and 104 (42%) had OSAS. The peak occurrence of sleep disorder happened between 4 and 7 years. The prevalence of OSAS among males was 60% (62) and among females was 42% (42). Chart 1 shows the distribution of sleep respiratory disorders according to gender in the different age ranges.
Chart 1. Distribution of sleep respiratory disorders according to gender and age.
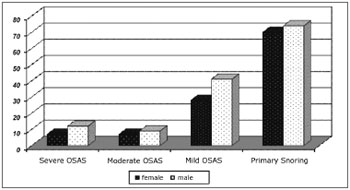
Among the 104 patients with OSAS, 69.67% had the mild type; 16.15%, had the moderate type and 19.18% had severe OSAS. Chart 2 shows that the same ratios were obtained when we break down respiratory sleep disorders according to gender.
Chart 2. Distribution of sleep respiratory disorders according to age and gender.
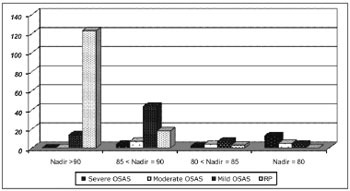
The level of O2 desaturation varied as depicted on Chart 3. The lower nadir values were found among severe and moderate OSAS.
Chart 3. O2 saturation Nadir in sleep respiratory disorder.
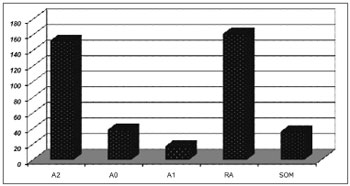
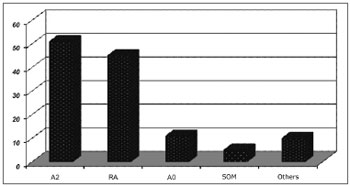
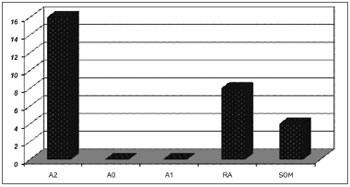
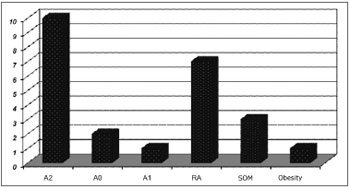
Otorhinolaryngological findings are listed on Charts 4, 5, 6 and 7, which show the distributions of the most commonly found Otorhinolaryngological disorders, according to the types and levels of sleep respiratory disorders.
Chart 4. ENT findings in patients with sleep respiratory disorders.
Chart 5. ENT findings in patients with mild OSAS.
Chart 6. ENT findings in patients with moderate OSAS.
Chart 7. Clinical and ENT findings n patients with severe OSAS.
In general, the most frequently found ENT alterations are: adenoid and tonsil hypertrophy (n=152; 61.2%), palatine tonsil hypertrophy (n=17; 6.8%); pharyngeal tonsil hypertrophy (n=37; 14.9%), allergic rhinitis (155; 62.5%) and secretory otitis media (36; 14.5%).
In all groups, adenoid and tonsil hypertrophy associated with allergic rhinitis were the most common finding.
The correlation between mouth breathing and OSAS was significant for adenoid and tonsil hypertrophy (p=0.001), and there were no significant differences concerning children with allergic rhinitis, tonsil hypertrophy, adenoid hypertrophy and nasal septum deviation.
DISCUSSION
Despite the huge attention the medical community has been paying to sleep respiratory disorders lately, the literature is still relatively poor as far as the pediatric population is concerned.
Our study was carried out with mouth breathing children whom, based on epidemiological studies, can vary between 20 and 40%7,8 of the general pediatric population. We have noticed that the frequency of these disorders, especially primary snoring and OSAS, is very significant in this particular population.
In this study, the prevalence of OSAS was higher among boys, which was not reported by prior epidemiological studies7,21-24. Nonetheless, in the adult population, males are more often affected25,26. This happens because of the influence of male sex hormones in respiratory control and/or body fat distribution.
We should bear in mind that our institution has a huge backlog of patients waiting for adenotonsillar surgery (as it happens in other large institutions). In some cases, the patients wait for more than three years. It is likely that mothers, concerned with their daughters (female snoring is more disruptive than in males) went to other institutions, and for that reason we lost follow up in our ward.
The peak of prevalence in both genders happened between 4 and 7 years, an age in which adenoid and the tonsils naturally grow. Moreover, it is possible that with children going to day-care centers and schools, a factor known to predispose children to repetitious upper airway infection, may also represent a worsening factor in the induction of adenotonsillar hypertrophy, worsening even further the respiratory condition of the children in this age range.
Although moderate and severe OSAS have been less frequent in relation to other sleep disorders, they were present in 35 (14%) children and, as expected, these were the ones who had the highest saturation drops. It is also interesting to stress that it was only in the group of severe OSAS that children were obese, although obesity is not an associated factor. This data matches sleep studies in obese children27.
The most commonly found otorhinolaryngological disorder in patients with sleep respiratory disorder was palatine and pharyngeal tonsil hypertrophy, either with or without allergic rhinitis. Such finding coincides with data from prior studies published in the literature on OSAS etiology pointing to adenoid and tonsil hypertrophy as the main causes of OSAS in children3,5. Chronic secretory otitis media (SOM), was also a very frequent ENT disorder found in our patients. This fact is probably associated with mouth breathing10 and the presence of pharyngeal tonsil hypertrophy, a major cause of mouth breathing and Eustachian Tube dysfunction in children.
The results from our study show the importance of sleep respiratory disorders in the pediatric population by its frequency. Nonetheless, it is important to stress the major clinical relevance of such disorders which, as shown in prior studies6,7,13-16, made the children more prone to hyperactivity and attention deficit, besides impairing learning. Therefore, in regards of the child's development, the knowledge about the real incidence of apnea in the pediatric population complaining of mouth breathing is very important, because of the need for an early intervention which can prevent carriers from developing school problems and, consequently, social and psychological ones. Since the otolaryngologist and the pediatrician are the first to have contact with this type of patient, it is very important that these professionals have an eye open for the diagnosis of sleep disorders, thus making the intervention early and correct.
The follow up of these patients after clinical or surgical treatment of the associated disorders, including polysomnography, may contribute to the knowledge of the natural history of these disorders and its physiopathology.
CONCLUSIONS
1. The incidence of OSAS occurrence in the mouth breathing children of our study was 42%.
2. In these children, the OSAS prevalence peak happened between 4 and 7 years of age.
3. The most frequently found ENT disorder in OSAS children was adenoid and tonsil hypertrophy with or without allergic rhinitis.
ACKNOWLEDGEMENTS
AFIP
REFERENCES
1. Castronovo V, Zucconi M, Nosetti L, Marazzini C, Hensley M, Veglia F, et al. Prevalence of habitual snoring and sleep-disordered breathing in preschool-aged children in na italian community. J Pediatr. 2003;142:377-82
2. Supriyatn B, Deviani R, Tumbelaka AR. The prevalence and risk factors of snoring in children in Jakarta. Paediatr Respir Rev. 2006;7:S297-S298.
3. Hultcrantsz E, Löftrand-Tideström B, Ahlquist-Rastad J. The Epidemiology of sleep related breathing disorder in children. Int J Otorhinolaringol. 1995;32(Supl),S63-S66
4. Montgomery-Down HE, Gozal D. Sleep habits and risk factors for sleep-disordered breathing in infants and young toddlers in Louisville, Kentucky. Sleep Med. 2006;7(3):211-9. Epub 2006
5. Santos, D. L. Estudo da prevalência da respiração predominantemente bucal e possíveis implicações com o aleitamento materno em escolares de São Caetano do Sul - SP - Brasil. Tese (mestrado) - UNICAMP, Campinas, 2004
6. Brunetti L, Rana S, Lospalluti ML, Pietrafesa A, Francavilla R, Fanelli M, et al. Prevalence of obstructive sleep apnea syndrome in a cohort of 1,207 children of southern Italy. Chest. 2001;120:1930-5
7. Ersu F, Arman AR, Save D, Karadag D, Karacoc F, Berkem M, et al. Prevalence of snoring and symptoms of sleep-disordered breathing in primary school children in Istanbul. Chest. 2004;126:19-24
8. Caprioglio A, Zucconi M, Calori G, Troiani V. Habitual snoring, obstructive sleep apnea and craniofacial modification: orthodontic, clinical and diagnostic aspects in a case control study. Minerva Stomatol. 1999;48,125-37
9. Behlfelt K; Linder-Aronson S; Neander P. Posture of the head, the hyoid bone, and the tongue in children with and without enlarged tonsils. Eur J Orthod. 1990;12(4):458-67.
10. Van Cauwenberge P, Derycke A. The relationship between nasal and middle ear pathology. Acta Othorhinolaryngol Belg. 1983;37(6):830-41
11. Rappa M; Collop N, Kemp S, deShazo R . The nose and sleep-disordered breathing:what we know and what we do not know. Chest.2003;124(6):2309-23
12. White D, Cadieux R, Lomard R et al. The effects of nasal anesthesia on breathing during sleep. Am Rev Respir Dis. 1985;132:972-5
13. Weissbluth M, Davis AT, Poncher J, Reiff J. Signs of airway obstruction during sleep and behavioral, developmental, and academic problems. J Dev Behav Pediatr.1983;4:119-21
14. Gozal D. Sleep-disordered breathing and school performance in children. Pediatrics. 1998;102:616-20
15. Bar A, Tarasiuk A, Segev Y, Phillip M, Tal A. The effect of adenotonsillectomy on serum insulin-like growth factor-I and growth in children with obstructive sleep apnea syndrome. J Pediatr. 1999;135:76-80
16. Tal A, Leiberman A, Margulis G, Sofer S. Ventricular dysfunction in children with obstructive sleep apnea: radionuclide assessment. Pediatr Pulmonol. 1988;4:139-14
17. Anstead M. Pediatric sleep disorders: new developments and evolving understanding. Curr Opin Pulm Med. 2000;6:501-6.
18. Kirk V, Kahn A, Brouillette RT. Diagnostic approach to obstructive sleep apnea in children. Sleep Med Rev. 1998;2(4);255-69
19. American Thoracic Society. Standards and indications for cardiopulmonary sleep studies in children. Am J Respir Crit Care Med. 1996;153:866-78.
20. Harvey JMM, OCallaghan MJ, Wales PD, Harris MA, Masters IB. Etiological factors and development in subjects with obstructive sleep apnea. J Paediatr Child Health. 1999;35:140-4
21. Ali NJ, Pitson DJ, Stradling JR. Snoring, sleep disturbance and behavior in 4-5 year olds. Arch Dis Child. 1993;68:360-6
22. Gislason T, Benediktsdottir B. Snoring, apneic episodes, and nocturnal hypoxemia among children 6 months to 6 years old: an epidemiological study of lower limit of prevalence. Chest. 1995;107:963-6
23. Teculesc, DB, Cailie, I, Perrin P. Snoring in French preschool children. Pediatric Pulmonol. 1992;13:239-44
24. Corbo GM, Fuciarelli F, Foresi A, De Benedetto F. Snoring in children: association with respiratory symptoms and passive smoking. BMJ. 1989;299:1491-4
25. Larsson LG, Lindberg A, Franklin KA, Lundback B. Gender differences in symptoms related to sleep apnea in a general population and in relation to referral to sleep clinic. Chest. 2003;124:204-11
26. Strohl KP, Redline R. Recognition of obstructive sleep apnea. Am J Respir Crit Care Med. 1996;154:279-89
27. Silvestri JM, Weese-Mayer DE, Bass MT, Kenny AS, Hauptman SA, Pearsall, SM. Polysomnography in obese children with a history of sleep-associated breathing disorders. Pediatr Pulmonol. 1993;16(2):124-9
28. Patten, Mildred L. (2002). Understanding research methods: An Overview of the essentials (3rd ed.). Los Angeles: Pyrczak Publishing
1. MD. ENT Resident physician - Federal University of São Paulo - Medical School (UNIFESP-EPM).
2. MD. ENT Resident physician - UNIFESP-EPM.
3. PhD - UNIFESP-EPM, Physician at the Pediatrics Polysomnography Ward - Department of Psychobiology - UNIFESP-EPM.
4. MSc in Otorhinolaryngology - UNIFESP-EPM, ENT Physician.
5. Associate Professor of Psychobiology - UNIFESP-EPM, Full Professor and Head of the Psychobiology Department of the UNIFESP-EPM.
6. Post-Doctorate degree in ENT - UNIFESP-EPM, Adjunct Professor and Head of the Pediatric Otorhinolaryngology Program.
7. PhD in Otorhinolaryngology - UNIFESP-EPM, Adjunct Professor and Head of the Pediatric Otorhinolaryngology Program - UNIFESP-EPM.
Universidade Federal de São Paulo - Escola Paulista de Medicina
Send Correspondence to:
Rua dos Otonis 684 Vila Clementino
São Paulo SP
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) oon July 16, 2007
and accepted on July 14, 2010. cod. 4666