Year: 2010 Vol. 76 Ed. 2 - (21º)
Relato de Caso
Pages: 272 to 272
Sclerosing Polycystic Adenosis of the minor salivary gland: case report
Author(s): Clarissa Araújo Silva Gurgel1, Valéria Souza Freitas2, Eduardo Antônio Gonçalves Ramos3, Jean Nunes dos Santos4
Keywords: salivary gland diseases, oral mucosa.
![]()
INTRODUCTION
Sclerosing Polycystic Adenosis (SPA) is a rare disease of the salivary glands, first described by Smith et al.1 in 1996, with histomorphological aspects similar to those from breast fibrocystic disorders1. Its pathogenesis is still unclear; however, it is considered a pseudo-neoplastic or reactive process1-3. Recently, Skálová et al.4 showed clonality in six SPA cases.
SPA affects mainly the parotid and submandibular glands, being much less frequent on the minor salivary glands2. Here, we report a case of SPA in a minor salivary gland and we discuss its histomorphological aspects.
CASE PRESENTATION
Female, African-Brazilian, 82 years old, came to us complaining of pain in the mouth floor when using her full mandible denture. During her intraoral exam, we noticed a misfitting of the upper and lower dentures and an ulcerated, reddish and firm nodule, measuring 2cm in its longest axis.
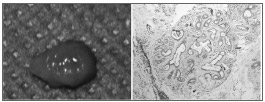
The patient was instructed to refrain from using her dentures and after 15 days she returned for nodule reassessment - which remained unaltered. With clinical suspicion of an erythroplastic lesion, we carried out an incisional biopsy and the material was then referred to the Laboratory of Surgical Pathology. The lesion was characterized by fibrous nodules permeated by interconnecting tubules, either ectasic or with apocrine metaplastia (Figure 1). Some ductal elements were hyperplastic and there wereatypic and vacuolated cells, followed by sparse mononuclear inflammatory infiltrate. Immunohistochemistry showed that the tubuloacinar elements which were positive to CKAE1/AE3, EMA, S-100, smooth muscle actin, GCDFP-15 and Ki-67 antibodies marked less than 1% of the cells. Estrogen, progesterone and CK 34?E12 were negative. SPA was diagnosed on the mouth floor, and the patient was later on submitted to total lesion exeresis. After 24 months there were no signs of recurrence.
Figure 1. Sclerosing Polycystic Adenosis - Nodular aspect of the lesion after surgical excision. In the slide, notice a fibrous nodule permeated by interconnecting tubules, sometimes ectasic.
DISCUSSION
The literature has approximately 35 cases of SPA reported so far, with only four of those involving minor salivary glands. Therefore, this is the fifth case of minor salivary gland SPA.
Since this is a rarely described lesion, there is no characteristic clinical data for it. Smith et al.1 published a series of 9 cases, in which the average age of the patients affected by this problem was 28 years, with mild predilection for females. Gneep et al.2 reported an average age of 44.5 years and a mild predilection for men. An increase in nodular volume by slow growth, as we had in our case, is one of the most common clinical aspects3.
The histomorphological aspects hereby described fit those established for SPA. The lesion was made up of fibrous nodules, permeated by interconnecting tubules, either ectasic or with apocrine metaplasia, also showing cell vacuolization and atypia1-3,5. According to Cheuk, Chan3, SPA histological aspects are still not very known and, often times, such lesion is diagnosed as a malignant neoplasia, and a highlight among them is the ductal carcinoma1,2,5, cystic-adenocarcinoma, acinar cell carcinoma and mucoepidermoid carcinoma1. Sclerosing sialoadenites has also been included1,2-5.
Immunohistochemistry for proteins S-100 and smooth muscle actin, from the case presented, showed the presence of myoepithelial cells in the tubule-acinar elements of the lesion1,2. The presence of such cells shows that despite the cell atypia seen in the SPA, the glandular ducts are functionally normal2. Gneep5 was also positive for cytokeratin and EMA in the ductal and acinar cells. Immune-staining for estrogen, progesterone and GCDGP-15 has also been described3,5,6, suggesting the participation of hormonal factors in the SPA6 pathogenesis. In this case, GCDFP-15 was positive; however, it is necessary to have the immunohistochemical study of other cases in order to establish the histogenetic profile of SPA.
SPA's treatment is based on lesion excision - with safe margins. Follow up must be careful because recurrences are common2,6.
FINAL REMARKS
SPA's diagnosis must be carefully considered, especially because of its histomorphological similarity with different malignant neoplasias of the salivary gland.
REFERENCES
1. Smith BC, Ellis GL, Slater LJ, Foss RD. Sclerosing polycystic adenosis of major salivary glands: A clinicopathologic analysis of nine cases. Am J Surg Pathol. 1996;20(2):161-70.
2. Gnepp DR, Wang LJ, Brandwein-Gensler M, Slootweg P, Gill M, Hille J. Sclerosing polycystic adenosis of the salivary gland: a report of 16 cases. Am J Surg Pathol. 2006;30(2):154-64.
3. Cheuk W, Chan JKC. Advances in salivary gland pathology. Histopathology. 2007;51(1):1-20.
4. Skálóva A, Gnepp DR, Simpson RHW, Lewis JE, Janssen D, Sima R et al. Clonal nature of sclerosing polycystic adenosis of salivary glands demonstrated by using the polymorphism of the Human Androgen Receptor (HUMARA) Locus as a marker.AmJ Surg Pathol. 2006;30(8):939-44.
5. Gnepp DR. Sclerosing polycystic adenosis of salivary gland: a lesion that may be associated with dysplasia and carcinoma in situ. Adv Anat Pathol. 2003;30(4):218-22.
6. Skálová A, Michal M, Simpson RHW, Stárek I. Sclerosing polycystic adenosis of parotid gland with dysplasia and ductal carcinoma in situ. Virchow Arch. 2002;440(1):29-35.
1. MSc., Substitute Professor.
2. MSc., Assistant Professor.
3. PhD, Adjunct Professor IV.
4. PhD, Adjunct Professor IV.
Universidade Federal da Bahia Faculdade de Odontologia Laboratório de Patologia Cirúrgica.
Send correspondence to:
Jean Nunes dos Santos Faculdade de Odontologia - UFBA
Avenida Araujo Pinho 62 Canela
Salvador BA 40110-150.
FAPESB - convęnio 200/04
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on August 24, 2007;
and accepted on December 16, 2007. cod. 4738
All rights reserved - 1933 /
2026
© - Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico Facial