Year: 2010 Vol. 76 Ed. 2 - (5º)
Artigo Original
Pages: 172 to 177
Solid ameloblastomas - Retrospective clinical and histopathologic study of 54 cases
Author(s): Giovana Medeiros Fulco1, Cassiano Francisco Weege Nonaka2, Lélia Batista de Souza3, Márcia Cristina da Costa Miguel4, Leăo Pereira Pinto5
Keywords: ameloblastoma, mandible, maxilla, odontogenic tumors.
Abstract:
Recently, the World Health Organization (WHO) excluded the desmoplastic pattern from the histopathological spectrum of solid ameloblastomas and classified it as a distinct variant, named desmoplastic ameloblastoma. Aim: To perform a retrospective analysis of the clinicopathologic aspects in a case series of solid ameloblastomas. Study design: Crosssectional cohort study. Materials and methods: Data regarding age, gender, location and clinical characteristics were retrieved from patient records. Histological sections were evaluated regarding existing histological patterns and the predominant histological pattern. Cases were classified according to the study of Waldron and El-Mofty (1987) and the WHO classification of 2005. Results: A total of 54 cases were identified, with similar gender distribution and a mean age of 38.3 years. Fifty three cases (98.1%) affected the mandible. Forty nine cases (90.8%) were classified as solid ameloblastomas, 3 (5.6%) as desmoplastic ameloblastomas, and 2 (3.7%) as hybrid lesions. The most frequent histological patterns in solid ameloblastomas were follicular (77.6%), acanthomatous (69.4%), and plexiform (65.3%). Focal areas of desmoplastic ameloblastomas were identified in 11 solid ameloblastomas (22.4%). Conclusion: Despite its characterization as a distinct variant, our results revealed that focal areas of desmoplastic ameloblastomas can be observed with some frequency in conventional ameloblastomas.
![]()
INTRODUCTION
Ameloblastoma is a benign epithelial odontogenic tumor, locally invasive and of slow growth1. Numerous histological patterns can be seen in these lesions, such as: follicular, plexiform, acanthomatous, desmoplastic, basal cells and granular2. Up to 1992, the World Health Organization (OMS) recognized the existence of 3 distinctive clinicopathologic variants of ameloblastoma, called conventional solid ameloblastoma, unicystic ameloblastoma and peripheral ameloblastoma3.
Case reports and retrospective studies4-8 carried out after the WHO's 1992 classification3 reported important clinical and image differences between ameloblastomas comprised exclusively of the desmoplastic pattern and solid lesions made by the remaining histological patterns. Thus, in their most recent classification of odontogenic tumors, published in 2005, the WHO excluded the desmoplastic pattern from the histological spectrum of solid ameloblastomas and placed it as a distinctive variant called desmoplastic ameloblastoma9.
According to the WHO9, ameloblastomas which have both solid and desmoplastic areas are called hybrid lesions. It is suggested that the hybrid lesions represent a coalition of tumors10,11. Notwithstanding, Melrose12 states that the word "hybrid" does not have a clearly defined purpose and, if considered literally, can overestimate the meaning of seeing areas of desmoplastic ameloblastoma in combination with islets of solid ameloblastoma.
Having the recent classification of odontogenic tumors from the WHO9, the present study aims at doing a retrospective analysis of the clinical and histopathological findings from a number of solid ameloblastomas filed in the Laboratory of Oral Pathology of the Department of Dentistry of the Federal University of Rio Grande do Norte (UFRN).
MATERIALS AND METHODS
We carried out a retrospective study in a series of cases of solid ameloblastomas using clinical charts and histology slides found in the files of the Laboratory of Oral Pathology of the Department of Dentistry of the UFRN. This study was approved by the Ethics in Research Committee of the UFRN (Document # 171/2008).
We used 54 cases of solid ameloblastomas. The criteria established in order to include the cases in the sample were the presence of a recorded chart, with the gender of the patient and anatomical location of the lesions, as well as the existence of enough biological material in the paraffin blocks in order to prepare the histology slides. Any case which did not match the criteria previously established was taken off the study.
For the clinical study, we collected data regarding the patients' gender and age, as well as anatomical location, symptoms and time of lesion development.
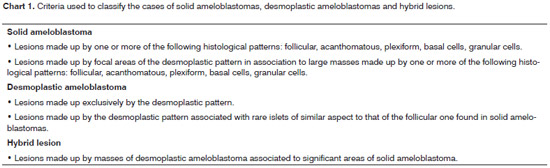
For the morphological study we used 5mm thick slides cut from the paraffin material, dyed by the hematoxylin- eosin technique. The specimens were analyzed under light microscopy (Olympus X31 microscope), identifying the histological patterns present and the predominant histological pattern in the lesions. Later on, having as reference the study led by Waldron and El-Mofty13 and the classification of odontogenic tumors by the WHO9, The cases were classified into desmoplastic solid ameloblastomas or hybrid lesions. The criteria used to classify the cases are presented on Chart 1.
The data obtained was plotted on electronic spreadsheets using Microsoft Excel (Microsoft Corporation), and later on exported to the Statistical Package for Social Sciences (SPSS 13.0), from which we obtained the mean values, absolute and percentage frequencies through descriptive statistics techniques. In order to analyze the differences between solid ameloblastomas, desmoplastic ameloblastomas and hybrid lesions in relation to gender, anatomical location, region and symptoms, we used the Chi-Squared test, considering p<0.05 as significant value.
RESULTS
The analysis of the clinical data revealed a similar involvement between the genders, with 27 cases (50.0%) diagnosed in men and 27 (50.0%) in women. The age of the patients varied between 12 and 92 years, with a mean value upon diagnosis of 38.3 years. Men and women revealed mean ages of 38.2 and 38.4 years, respectively. As far as anatomical location is concerned, we noticed a predilection for the mandible (98.1%). Most of the cases were asymptomatic (82.1%) and were located in the posterior portion of the gnathic bones (66.7%). Time of evolution varied between 1 month and 33 years, with a mean value of 34.9 months. The diameter of the lesions varied between 0.7 cm and 15.0cm, with a mean value of 4.2cm.
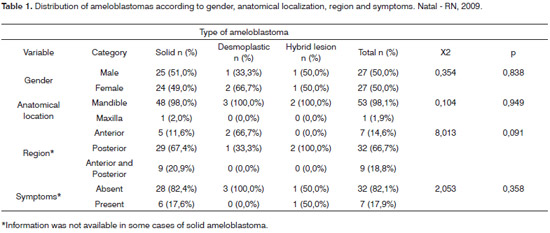
After histopathological evaluation, 49 cases (90.8%) were classified as solid ameloblastomas, 3 (5.6%) as desmoplastic ameloblastomas and 2 (3.7%) as hybrid lesions. The clinical data related to gender, anatomical location, region and symptoms concerning each type of ameloblastoma are presented on Table 1. We did not notice statistically significant differences between solid ameloblastomas, desmoplastic ameloblastomas and hybrid lesions as far as gender is concerned (p=0.838), anatomical location (p=0.949), region (p=0.091) and symptoms (p=0.358).
Solid ameloblastomas affected patients with ages between 12 and 92 years (mean of 37.7 years). Desmoplastic ameloblastomas and hybrid lesions were respectively diagnosed in patients with ages between 20 and 51 years (mean of 34.3 years) and 44 and 71 years (mean of 57.5 years). In relation to size, solid ameloblastomas had diameters between 0.7 cm and 15.0cm (mean of 4.3cm), while desmoplastic ameloblastomas have a diameter between 3.0cm and 4.0cm (mean of 3.5cm). Information regarding size was available in only one case (50.0%) of hybrid lesion, which showed a diameter of 5.0cm. The time of evolution for solid lesions varied between 1 month and 33 years (mean of 36.9 months). Desmoplastic ameloblastomas and hybrid lesions showed, respectively, evolution times between 12 and 24 months (mean of 18 months) and 18 and 24 months (mean of 21 months).
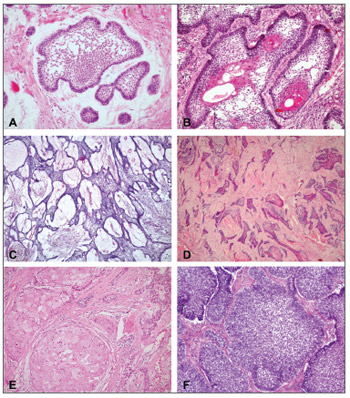
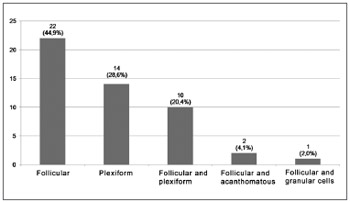
The follicular (77.6%) (Fig. 1A), acanthomatous (69.4%) (Fig. 1B) and plexiform (65.3%) (Fig. 1C) histologic patterns were the most frequent among the solid ameloblastomas. Notwithstanding, focal areas of desmoplastic ameloblastomas were identified in 11 solid lesions (22.4%) (Fig. 1D). And finally, granular cells and basal cells patterns were the least common in solid ameloblastomas, being identified in 12.2% (Fig. 1E) and 8.2% of the cases (Fig. 1F), respectively. The analysis of the predominant histological pattern in solid ameloblastomas revealed the follicular as the most frequent (44.9%), followed by the plexiform (28.6%) and the follicular/plexiform association (20.4%). The distribution of the cases of solid ameloblastoma in relation to the predominant histologic pattern is presented on Fig. 2.
Figure 1. Microphotography of histological patterns. (A) Follicular pattern (H/E-200x); (B) Acanthomatous pattern (H/E-200x); (C) Plexiform pattern (H/E-100x); (D) Desmoplastic pattern (H/E-100x); (E) Granular cells pattern (H/E-200x); (F) Basal cells pattern (H/E-200x).
Figure 2. Frequency of the predominant histological pattern in solid ameloblastomas.
Among the hybrid lesions, the ratio of the solid ameloblastoma areas and that of desmoplastic ameloblastomas was similar (50.0%/50.0%). An assessment of solid ameloblastoma areas in the three hybrid lesions revealed only the histological patterns (100.0% of the cases), plexiform (100.0% of the cases) and acanthomatous (50.0% of the cases). Desmoplastic ameloblastomas had rare islets with a follicular pattern similar to those from solid lesions which were made almost exclusively of this histological pattern.
DISCUSSION
Because of clinical and image differences between ameloblastomas made up exclusively of the desmoplasticpattern and solid lesions made up of the other histological patterns4-8, in the most recent classification of odontogenic tumors from the WHO9, the desmoplastic pattern was taken off the histological spectrum of solid ameloblastomas and fit within a distinct variant, called desmoplastic ameloblastoma.
Solid ameloblastomas affect the mandible prefferably1,2,14,15, especially the posterior region1,15, with a proportion between the gnathic bones of 1:5.416. Our results corroborate the fact that these lesions have a predilection for the posterior mandible. Desmoplastic ameloblastomas affect predominantly the anterior maxillary bones5,8,13,17-19 and reveal a ratio varying between 1:0.6 and 1:16,9,18. The findings of the present study agree with the preferential involvement of the anterior maxillary bones by desmoplastic lesions. Moreover, the reduced number of desmoplastic ameloblastomas seen in the present study corroborates the reports on the low frequency of this variant, encompassing between 0.5% and 13.0% of all ameloblastomas1,2,4,5,13,15,18,19.
Despite the aforementioned differences, solid and desmoplastic ameloblastomas share clinical traits. Both of them present asymptomatic and slow growth masses1,9,18,19 and, in general, are diagnosed in individuals between 30 and 60 years1,4,9,11. Moreover, solid and desmoplastic ameloblastomas have a relatively similar distribution between the genders6,9,11,16. The results from the present investigation are in agreement with these statements.
In sync with the similarities aforementioned, Keszler et al.20 carried out a comparative study with solid and desmoplastic ameloblastomas and did not report relevant differences between the genders, age or recurrence after treatment. For these authors, the desmoplastic ameloblastomas should not be considered a distinct clinicopathologic variant.
The size reported for the desmoplastic ameloblastomas varied between 1.0cm and 8.5cm5,6,11,18,19, usually with a diameter larger than 3.0cm4-6,17,21. The average diameter for solid ameloblastomas varies between 4.3cm16 and 6.2cm1. Some cases may be very large, with diameters exceeding 15.0 cm22. In the present investigation, solid and desmoplastic lesions had a mean diameter of 4.3cm and 3.5cm, respectively. Such findings match the literature data and stress the absence of significant differences between these variants as to the size of the lesions.
Duration time of the solid ameloblastomas can extend from 1 to 40 years1,16, with mean times between 27 months16 and 42.9 months15. Duration of the desmoplastic lesions can extend from 1 month all the way to 20 years18,19, with a mean time of 23 months18. In the present investigation, solid and desmoplastic lesions had a mean development time of 36.9 months and 18 months, respectively. These results match literature reports and there may be a relatively longer duration for desmoplastic ameloblastomas.
In the present study, the analysis of the predominant histological pattern in the solid lesions revealed the follicular (44.9%), the plexiform (28.6%) and the follicular/ plexiform association (20.4%) as the most frequent ones. Similarly, Waldron and El-Mofty13 identified as predominantly common patterns in solid ameloblastomas the follicular (64.9%), the plexiform (16.9%) and the follicular/plexiform association (12.9%). Adebiyi et al.2 reported that most of the solid lesions belonged to the follicular type (70.4%), plexiform (14.1%) and acanthomatous (4.2%). Reichart et al.16 also reported the following solid lesions as being themost common patterns found: follicular (35.4%), plexiform (31.5%) and acanthomatous (11.8%). Our findings are in agreement with a greater frequency of follicular and plexiform patterns found in ameloblastomas.
In the present sample, most of the solid lesions (75.5%) were made up by more than one histological pattern. Similarly, in the study carried out by Adeline et al.15, 68.6% of the solid ameloblastomas revealed more than one histological pattern. Nonetheless, only 16.1% and 19.7% of the solid lesions evaluated by Reichart et al.16 and Kim and Jang14, respectively, showed more than one histological type. According to Adebiyi et al.2 and Waldron and El-Mofty13, ameloblastomas, especially the large ones, are made up of numerous histological patterns. For these authors, the quantity of tissue available for analysis has a relevant impact on the predominant histological type of ameloblastomas. Thus, it is possible that the differences seen between the present study and those by Reichart et al.16 and Kim and Jang14 are, in part, associated to the quantity of material available for microscopic evaluation.
In the present study, focal areas of desmoplastic ameloblastoma were seen in 11 (22.4%) solid lesions. Although the recent classification from the WHO9 describes the cases of solid and desmoplastic ameloblastomas as hybrid lesions, the rate of desmoplastic areas in these 11 solid lesions was not significant to classify them as hybrid. According to Waldron and El-Mofty13, the hybrid ameloblastoma lesions reveal typical areas of desmoplastic ameloblastomas in association with significant areas of solid ameloblastoma. Similarly, in the present study, the hybrid lesions revealed a similar ratio (50.0%/50.0%) among areas of solid and desmoplastic ameloblastomas. Thus, our studies reveal that focal areas of desmoplastic ameloblastomas can be identified with relative frequency in solid lesions.
Waldron and El-Mofty13 were the first to characterize the ameloblastoma hybrid lesion. Similarly to desmoplastic ameloblastomas, the hybrid lesions are rare, making up between 1.1%10 and 4.5% of all the ameloblastomas13. Cases have been seen in men and women between 25 and 82 years10,13,17,23,24. Most of the hybrid lesions affect the mandible10,13,17,23,24, and they can be restricted to the posterior region13 or simultaneously affect the anterior and posterior regions10,17,24. The results from the present investigation are in agreement with reports found in the literature.
In the hybrid lesions, the solid ameloblastoma areas are usually made up of the plexiform13 and follicular10,23 histological patterns. In the latter, sites of squamous metaplasia10,23 and keratinization10 have also been described. Our findings are in agreement with these observations. Rarely, the solid areas of hybrid lesions show basal cells patterns25 or those of granular cells10.
Numerous aspects associated with ameloblastoma hybrid lesions are yet to be unveiled. We still do not know whether areas of desmoplastic ameloblastomas transform into solid ameloblastoma or desmoplastic alterations happen afterwards in the stroma of a solid ameloblastoma11. For Waldron and El-Mofty13, the absence of desmoplastic alterations seen in most of the solid lesions seen in their study would back up the first hypothesis.
According with Takata et al.10 and Philipsen et al.11, hybrid lesions could represent a coalition of tumors. Notwithstanding, Melrose12 states that the term "hybrid" does not have a clearly defined purpose and, if considered literally, can overestimate the meaning of seeing areas of desmoplastic ameloblastomas in combination with islets of solid ameloblastoma. The identification of focal areas of desmoplastic ameloblastoma in 22.4% of the solid lesions evaluated in this study suggest that it is not very likely that we would have a coalition of tumors and corroborate the statement from Melrose12.
We must stress that the low frequency of desmoplastic ameloblastomas and hybrid lesions makes it difficult to identify possible clinical differences between these lesions, as well as between them and solid ameloblastomas. In sync with this statement, the percentage differences between solid and desmoplastic ameloblastomas, seen in some clinical findings reported in the present study, did not have statistical significance. Thus, we stress the importance of carrying out multicentric studies which could assess a larger number of cases of desmoplastic ameloblastomas and hybrid lesions.
CONCLUSION
The recent classification of odontogenic tumors of the WHO describes the desmoplastic ameloblastoma as a distinct variant and assigns the cases of coexistence between solid and desmoplastic ameloblastomas as hybrid lesions. Nonetheless, the results from this study reveal that focal areas of desmoplastic ameloblastomas can be identified with a relative frequency in solid ameloblastomas.
REFERENCES
1. Ledesma-Montes C, Mosqueda-Taylor A, Carlos-Bregni R, León ER, Palma-Guzmán JM, Paéz-Valencia C et al. Ameloblastomas: a regional Latin-America multicentric study. Oral Dis. 2007;13(3):303-7.
2. Adebiyi KE, Ugboko VI, Omoniyi-Esan GO, Ndukwe KC, Oginni FO. Clinicopathological analysis of histological variants of ameloblastoma in a suburban Nigerian population. Head Face Med. 2006;2:42.
3. Kramer IRH, Pindborg JJ, Shear M. WHO histological typing of odontogenic tumours. 2nd ed. Berlin: Springer-Verlag; 1992. p.124.
4. Kaffe I, Buchner A, Taicher S. Radiologic features of desmoplastic variant of ameloblastoma. Oral Surg Oral Med Oral Pathol. 1993;76(4):525-9.
5. Kishino M, Murakami S, Fukuda Y, Ishida T. Pathology of the desmoplasic ameloblastoma. J Oral Pathol Med. 2001;30(1):35-40.
6. Beckley ML, Farhood V, Helfend LK, Alijanian A. Desmoplastic ameloblastoma of the mandible: a case report and review of the literature. J Oral Maxillofac Surg. 2002;60(2):194-8.
7. Iida S, Kogo M, Kishino M, Matsuya T. Desmoplastic ameloblastoma with large cystic change in the maxillary sinus: report of a case. J Oral Maxillofac Surg. 2002;60(10):1195-8.
8. Mintz S, Velez I. Desmoplastic variant of ameloblastoma: report of two cases and review of the literature. J Am Dent Assoc. 2002;133(8):1072- 5.
9. Gardner DG, Heikinheimo K, Shear M, Philipsen HP, Coleman H. Ameloblastomas. In: Barnes L, Eveson JW, Reichart P, Sidransky D. World Health Organization Classification of Tumors. Pathology & Genetics of Head and Neck Tumours. Lyon: IARC Press; 2005. p.296-300.
10. Takata T, Miyauchi M, Ogawa I, Zhao M, Kudo Y, Sato S et al. So-called 'hybrid' lesion of desmoplastic and conventional ameloblastoma: report of a case and a review of the literature. Pathol Int.1999;49(11):1014-8.
11. Philipsen HP, Reichart PA, Takata T. Desmoplasic ameloblastoma (including "hybrid" lesion of ameloblastoma). Biological profile based on 100 cases from the literature and own files. Oral Oncol. 2001;37(5):455-60.
12. Melrose RJ. Desmoplastic ameloblastoma. Pathol Rev. 1999;4:21-7.
13. Waldron CA, El-Mofty SK. A histophatologic study of 116 ameloblastomas with special reference to the desmoplastic variant. Oral Surg Oral Med Oral Pathol. 1987;63(4): 441-51.
14. Kim SG, Jang HS. Ameloblastoma: a clinical, radiographic, and histopathologic study of 71 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91(6):649-53.
15. Adeline VL, Dimba EA, Wakoli KA, Njiru AK, Awange DO, Onyango JF, et al. Clinicopathologic features of ameloblastomas in Kenya: a 10-year audit. J Craniofac Surg. 2008;19(6):1589-93.
16. Reichart PA, Philipsen HP, Sonner S. Ameloblastoma: biological profile of 3677 cases. Oral Oncol. 1995;31B(2):86-99.
17. Higuchi Y, Nakamura N, Ohishi M, Tashiro H. Unusual ameloblastoma with extensive stromal desmoplasia. J Craniomaxillofac Surg. 1991;19(7):323-7.
18. Ng KH, Siar CH. Desmoplastic variant of ameloblastoma in Malaysians. Br J Oral Maxillofac Surg. 1993;31(5):299-303.
19. Lam KY, Chan ACL, Wu PC, Chau KY, Tideman H, Wei W. Desmoplastic variant of ameloblastoma in Chinese patients. Br J Oral Maxillofac Surg. 1998;36(2):129-34.
20. Keszler A, Paparella ML, Dominguez FV. Desmoplastic and nondesmoplastic ameloblastoma: a comparative clinicopathological analysis. Oral Dis. 1996;2(3):228-31.
21. Eversole LR, Leider AS, Hansen LS. Ameloblastoma with pronounced desmoplasia. J Oral Maxillofac Surg. 1984;42(11):735-40.
22. Kalavrezos N, Baldwin DJ, Walker DM. Giant neglected ameloblastoma: single stage treatment and clinicopathologic review. Br J Oral Maxillofac Surg. 2008;46(7):591-3.
23. Santos JN, Souza VR, Azevędo RA, Sarmento VA, Souza LB. "Hybrid" lesion of desmoplastic and conventional ameloblastoma: immunohistochemical aspects. Braz J Otorhinolaryngol. 2006;72(5):709-13.
24. Philipsen HP, Ormiston IW, Reichart PA. The desmo- and osteoplastic ameloblastomas. Histologic variant or clinicopathologic entity? Int J Oral Maxillofac Surg. 1992;21(6):352-7.
25. Hirota M, Aoki S, Kawabe R, Fujita K. Desmoplastic ameloblastoma featuring basal cell ameloblastoma: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99(2):160-4.
1. Dentistry student, scientific initiation scholarship holder - Federal University of Rio Grande do Norte.
2. MSc in Oral Pathology, PhD student in oral pathology - Federal University of Rio Grande do Norte.
3. PhD in Oral Pathology - Professor of the Graduate Program in Oral Pathology - Federal University of Rio Grande do Norte.
4. PhD in Oral Pathology, Professor of the Graduate Program in Oral Pathology of the Federal University of Rio Grande do Norte.
5. PhD in Oral Pathology, Professor of the Graduate Program in Oral Pathology - Federal University of Rio Grande do Norte.
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on June 30, 2009;
and accepted on August 13, 2009. cod.6484