Year: 2002 Vol. 68 Ed. 2 - (7º)
Artigo Original
Pages: 196 to 201
Eagle Syndrome: surgical treatment evaluation
Author(s):
Romualdo Suzano Louzeiro Tiago 1,
Marcílio Ferreira Marques Filho 2,
Clícia Adriana Santos Maia 3,
Osvaldo Fonseca Souza Santos 4
Keywords: Eagle's syndrome, ligament stylohyoid, ossification
Abstract:
Introduction: The styloid apophysis is an osseous outgrowth originating in the tympanum portion of the temporal bone. Its growth, or the ossification of the stylohyoid ligament, may cause a series of symptoms, such as dysphagia, odynophagia, facial pain, otalgia, cephalea, tinnitus and trismus. This set of symptoms associated to the presence of an elongated styloid aphophysis is known as the Eagle syndrome. Aim: To report on a group of four patients with Eagle syndrome, as well as to discuss the clinical presentation and the most suitable treatment of this disease. Study design: Clinical retrospective. Material and Method: A retrospective clinical study of four patients who were submitted to surgery at the HSPE-FMO (State Public Servants Hospital) of São Paulo, and at the HSPM (Municipal Public Servants Hospital) of the city of São Paulo, in the period from June, 1998, to June, 2001. The surgical treatment was the therapeutic option selected, with the removal of the elongated styloid aphophyses. The clinical evolution was assessed during the postoperative period. Results: Of the four patients, three were females and one a male, ages ranging from 38 to 68 years, with an average age of 57.25 years. The elongated styloid aphophyses were found and operated in both sides in 50% of the cases. Full remission of the symptoms occurred in three of the patients, and a partial improvement was observed in the other patient. Conclusion: This disease should be considered when the patient presents symptoms, such as dysphagia, odynophagia, facial pain, otalgia, cephalea, tinnitus and trismus. Surgical treatment is the best form of conducting such cases with patients presenting elongated styloid aphophysis and symptoms compatible with the Eagle syndrome, with the external approach being the one that offers greater safety and allows for a more complete resection.
![]()
INTRODUCTION
Styloid apophysis is a bone projection that originates from the tympanic portion of the temporal bone. The increase in styloid apophysis or ossification of stylohyoid ligament may trigger a number of symptoms such as dysphagia, odynophagia, facial pain, otalgia, headache, tinnitus and trismus. The syndrome was initially described in 1937 by W. W. Eagle, who observed associated cervical-pharyngeal symptomatology to the presence of elongated styloid apophysis (Eagle, 1937; Eagle, 1948)1,2. In the literature, we observed that there are two different types of Eagle's syndrome: classical Eagle's syndrome and carotid artery-styloid apophysis syndrome (Eagle, 1948)2.
Elongation of styloid apophysis may happen by a process of ossification of the stylohyoid ligament, which forms the stylohyoid ligament complex, or by growth of the apophysis as a result of some factor that triggers osteogenesis, such as for example, trauma (Balbuena et al, 1997)3.
The diagnosis should be considered in patients who present symptoms compatible with Eagle's syndrome, after the exclusion of other etiologies that originate similar manifestations. Digital palpation of tonsil site increases the pain reported by patients and confirms the diagnosis. Radiological assessment provides more objective parameters and allows measurement of styloid apophysis size.
In the present study, we present a group of four patients with elongated styloid apophysis whose symptoms were compatible to Eagle's syndrome, in order to discuss clinical presentation and the most appropriate treatment of the disease.
case report
Case 1
SSS, 38 year-old female patient, with complaint of acute cervical pain for approximately 6 years on the upper jugular-carotid region, associated to sensation of foreign body in the oropharynx, intense odynophagia, perioral pain, dysphagia and bilateral otalgia, worse on the right side. The patient did not report history of cervical trauma or tonsillectomy. At the onset of symptoms, she was diagnosed with temporomandibular dysfunction but there was no improvement after clinical treatment. In the initial examination, we did not perform palpation of tonsillar site.
As a result of progression of symptoms, we investigated gastroesophageal reflux disease and excluded the diagnostic hypothesis. Since the patient persisted with symptoms, she was reevaluated in the service and upon palpation of the tonsillar site we observed hardened, sharp and bilateral projection that increased pain upon palpation. On the neck examination, we palpated a nodular sharp lesion on the upper jugular-carotid region at the level of the mandible angle. We ordered computed tomography scan (CT scan) of skull base and neck with three-dimensional reconstruction, and it revealed symmetrical and prominent styloid apophyses of about 4cm each (Figure 1). The other bone structures were within the normal range. A mandible panoramic x-ray showed elongated styloid apophysis and calcification of stylohyoid ligament (Figure 2).
The patient was submitted to surgical upper cervicotomy of 4cm long and 3cm from the mandible angle. We identified sternocleidomastoid muscle, posterior portion of digastric muscle, internal and external carotid arteries, styloid process and stylohyoid, styloglossus and stylopharyngeal muscles. Next, we performed subperiosteal detachment and removed 3cm fragments of the styloid apophysis on both sides.
After three months of postoperative follow-up, the patient reported complete remission of symptoms.
Case 2
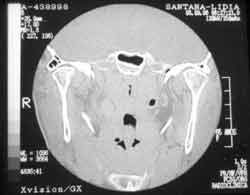
LPS, 65 year-old female patient, assessed by the Service of Neurosurgery, HSPE - FMO, with complaint of pain on the right hemiface, she took carbamazepine and it did not improve her clinical picture. After 4 years from the first assessment, the patient felt severe pain on the right lateral border and base of the tongue. We performed nervous block of glossopharyngeal nerve on the right with 4ml of lidocaine at 2%, intraorally, with complete remission of pain. After the therapeutic trial, Eagle's syndrome was diagnosed and the patient was referred to the Sector of Head and Neck Surgery at HSPE-FMO, where she reported cervical pain on the upper jugular-carotid region for 7 years, radiated to the right lateral border of the tongue and occipital region. She also reported pain on the same region on the other side, but less marked. She did not report history of cervical trauma or tonsillectomy. In the physical examination, the palpation of tonsillar site revealed hardened, sharp, bilateral projection, followed by increased pain upon palpation. The neck examination revealed nodular and sharp lesion on the upper jugular-carotid region at the level of the mandible angle, larger on the right side. We ordered skull base and head CT scan and observed symmetrical and prominent styloid apophyses (Figure 3), reaching the level of C3, at the level of lateral pharyngeal space (tonsils). Anterior-posterior cranial x-ray confirmed the increase in styloid apophysis and calcification of stylohyoid ligament, especially on the right side (Figure 4).
The patient was submitted to surgical treatment - upper cervicotomy, and we removed fragments of about 3.5cm from the styloid apophyses on both sides.
After 8 months of postoperative follow-up, the patient reported partial remission of symptoms, still presenting mild cervical pain on the right side.
Case 3
CCN, 58-year-old female patient, had complaint of upper cervical pain for approximately 1 year, radiated to the left ear and associated to foreign body sensation in the pharynx and mild dysphagia. The patient did not report history of cervical trauma or tonsillectomy. Upon physical examination, we observed thickness of the anterior pillar of the left side tonsil and upon palpation of the tonsil site we detected hardened and sharp projection. Mastoid and cranial x-rays were ordered and they showed longer styloid apophysis on the left, which was possibly widened in the proximal segment compared to the contralateral styloid apophysis (Figure 5).
The patient was submitted to surgical treatment with upper cervicotomy and a fragment of approximately 4cm was removed from the styloid apophysis on the left side.
Five months after the surgery, the patient reported complete remission of symptoms.
Case 4
AL, 68-year-old male patient, reported sensation of foreign body on the base of the tongue for approximately 6 years, associated to high cervical pain on the left, radiated to the left ear. The patient did not refer history of cervical trauma or tonsillectomy. Upon the physical examination, we palpated, on the left tonsillar site, a hardened and sharp projection. We ordered cervical planigraphy that revealed long styloid apophysis on the left side.
The patient was submitted to surgical treatment with upper cervicotomy and a fragment of approximately 3cm was removed from the styloid apophysis on the left side.
After 13 months of postoperative follow-up, the patient reported complete remission of symptoms.
RESULTS
We performed a retrospective clinical study of four patients operated on at Hospital do Servidor Público Estadual, - FMO and Hospital do Servidor Público Municipal, São Paulo, between June 1998 and June 2001. Out of the 4 patients, three were females and one was male, ages ranging from 38 to 68 years, mean age of 57.25 years. Elongated styloid apophysis was found and operated bilaterally in 50% of the cases. The chosen access route was external, and we observed complete remission of symptoms in three patients and partial improvement in the other patient.
Table 1.
Figure 1. Skull base computed tomography (CT scan) scan with three-dimensional reconstruction, showing elongation of styloid apophysis and ossification of stylohyoid ligament, more on the right, approaching the hyoid bone.
Figure 2. Mandible panoramic x-ray. The arrows indicate the elongated styloid apophyses,
Figure 3. Skull base CT scan showing elongated styloid apophyses that reached the pharyngeal lateral space.
Figure 4. Cranial anterior-posterior simple x-ray - Arrows indicate the elongated styloid apophyses, more on the right.
Figure 5. Cranial profile simple x-ray - Arrows indicate the elongated styloid apophyses.
DISCUSSION
Styloid apophysis is an elongated cylindrical and sharp bone projection that originates anterior-medially from the mastoid process. The length varies from 2 to 3cm, serving as an attachment point for the stylohyoid, styloglossus and stylopharyngeal muscles. The facial nerve emerges posteriorly as from the stylomastoid foramen, and crosses laterally through the parotid gland. Medially to the styloid apophysis, we find the internal jugular vein, glossopharyngeus, vagus and accessory cranial nerves, and internal carotid artery. Medially to the tip of the apophysis there is the superior pharyngeal constrictor muscle and pharyngeal-basilar fascia, adjacent to the tonsillar fossa. Laterally, there is the external carotid artery. The stylohyoid ligament extends from the styloid apophysis to the smaller horn of the hyoid bone. These structures are derived from the mesenchyma of the second branchial arch or Reichert cartilage (Balbuena et al, 1997)3.
The ossification of stylohyoid ligament or growth of styloid apophysis of the temporal bone is not rare and it may affect nearly 4% of the general population (Gossman et al, 1977)4; some authors believe that the incidence may be as high as 28% (Gorlin et al, 1990)5. Approximately 50% of the cases present a tendency of having it on both sides and the presence of symptoms is associated to proximity of styloid apophysis with the internal and external carotid artery, trigeminal nerve, facial nerve, glossopharyngeus nerve, vagus nerve, pharyngeal muscles and pharyngeal mucosa (Balbuena et al, 1997; Guo et al, 1997)3,6.
Eagle's syndrome was described in 1937 and it is clinically divided into two categories: Classical Eagle's syndrome and carotid artery-styloid apophysis syndrome. The classical Eagle's syndrome was described as the presence of continuous pharyngeal pain, worsened during swallowing and associated with ipsilateral reflex otalgia, increase of salivation and sensation of pharyngeal foreign body. The pain was attributed to the healing process present after tonsillectomy or a cervical trauma and it may affect all age ranges (Eagle, 1937)1.
The carotid artery-styloid apophysis syndrome is not associated to tonsillectomy and it is probably the result of internal and external carotid artery compression caused by stimulation of the sympathetic chain present on the walls of these vessels. The resulting symptom is carotodynia, that is, pain on the distribution regions of the carotid arteries: temporal or frontal headache, otalgia, dizziness, tinnitus (Eagle, 1937; Eagle, 1948; Balbuena et al, 1997)1,2,3. The most common symptoms in the carotid artery-styloid apophysis syndrome are dysphagia (80%), sensation of pharyngeal foreign body (50%), otalgia (45%), pain on the carotid artery distribution regions (20%), pain on the temporomandibular joint (10%), glossopharyngeus neuralgia (10%), and facial pain (10%) (Guo et al, 1997)6. The carotid artery-styloid apophysis syndrome occurs in middle aged patients because of the abnormal ossification process of stylohyoid ligament (Chouvel et al, 1996)7. Definite diagnosis is made by palpation of stylohyoid apophysis on the tonsillar site (Eagle, 1948; Gossman et al, 1977)2,4.
Clinical diagnosis is based on history of cervical-pharyngeal pain, associated to palpation of the styloid process through the tonsillar site or high cervical region. Styloid apophysis in normal people is not palpable. A firm and sharp resistance in the tonsillar site suggests elongation of the styloid apophysis and this movement normally triggers severe pain, similar to the pain reported by the patients. The diagnosis may be confirmed with infiltration of lidocaine in the tonsillar site, which is followed by complete remission of pain (Bafaqeeh, 2000)8.
The diagnostic suspicion of elongated styloid apophysis in a symptomatic patient may be confirmed with radiological study, including cervical planigraphy, head x-ray (lateral and anterior-posterior incidence) and mandible panoramic x-ray, plus head and neck CT scan. CT with three-dimensional reconstruction allows measurement of the styloid apophysis and assessment of ossification of the stylohyoid ligament (Bafaqeeh, 2000)8.
The literature is controversial in terms of the real existence of this syndrome, since there are many patients who have elongated styloid apophysis and do not manifest clinical symptomatology, questioning the cause-effect relation of the radiological finding. Keur et al (1986)9 observed that 33% of the women and 29% of the men have radiological abnormalities compatible with elongation of stylohyoid complex. Out of the total, only 31% present pain on the cervical region and 16% present facial pain, being the most frequent symptom in women. However, in such study, the authors did not report the result of clinical or surgical treatment.
There are some mechanisms that may explain the cause of pain in Eagle's syndrome, and the main ones are:
· secondary to mechanical irritation of pharyngeal mucosa;
· stretching of nervous endings of cranial nerves 5th, 7th, 9th and 10th, producing post-tonsillectomy fibrosis;
· fracture of the ossified stylohyoid ligament, caused by cervical trauma or sudden neck movement, with consequent proliferation of granulation tissue that may generate pressure on the structures of the stylohyoid complex;
· pressure on the carotid artery with stimulation of the sympathetic chain that involves the carotid sheath;
· degenerative abnormalities on the attachment tendon of stylohyoid muscle or attachment tendinitis.
Differential diagnosis of Eagle's syndrome should include all possible causes of pain in the region of the head and neck, especially trigeminal and glossopharyngeal neuralgia. Other causes include: temporomandibular joint dysfunction, tongue base and hypopharynx tumor, degenerative disorders of the cervical spine, chronic tonsillitis, chronic pharyngitis and chronic submandibulitis (Chouvel et al, 1996)7. Glossopharyngeal neuralgia is generally manifested as sharp recurrent pain of short duration normally triggered by hot and cold stimuli and sometimes by movements of the tongue base (Bafaqeeh, 2000)8. The main cause of glossopharyngeal secondary neuralgia is Eagle's syndrome, and resection of stylohyoid apophysis is the main treatment approach (Soh, 1999)10.
In the literature, we could observe two different ways of treating Eagle's syndrome when symptoms are disabling. Some authors advocated the clinical treatment with infiltration of corticoids or anesthetics (Kunachak, 1995)11. However, the most effective and satisfactory treatment is surgical resection of the styloid apophysis, either by external or intraoral approach (Bafaqeeh, 2000)8.
Despite the fact that intraoral access is faster and leaves no visible external scars (Soh, 1999; Bafaqeeh, 2000)8,10, it does not provide appropriate visualization of styloid apophysis adjacent structures and there is a higher risk of cervical space contamination. Moreover, it prevents wider resection of the styloid apophysis (Chouvel et al, 1996)7.
The advantages of the external access are better exposure and preservation of vascular and nervous structures and wide resection of styloid apophysis (Chouvel et al, 1996)7. The resulting scar of this surgical approach is high and cervical, leading to small and esthetically acceptable mark.
CONCLUSION
The disease may be considered when the patient presents symptoms such as dysphagia, odynophagia, facial pain, headache, tinnitus and trismus. Patients that present pain in the cervical-pharyngeal region should be submitted to clinical assessment, including palpation of the tonsillar site and radiological study to investigate abnormal ossification of osteo-ligament stylohyoid complex.
Surgical treatment to patients that present elongated stylohyoid apophysis with symptoms compatible with Eagle's syndrome is the best way to conduct these cases, and external approach is the one that provides more safety and enables complete resection.
REFERENCES
1. Eagle WW. Elongated styloid process. Report of two cases. Arch Otolaryngol 1937;25:584-7.
2. Eagle WW. Elongated styloid process Further observations and a new syndrome. Arch Otolaryngol 1948;47:630-40.
3. Balbuena L, Hayes D, Ramirez SG, Johnson R. Eagle's Syndrome: elongated styloid process. South Med J 1997;91:331-4.
4. Gossmann JR, Fla H, Tarsitano JJ. The styloid-stylohyoid syndrome. J Oral Surg 1977;35:555-60.
5. Gorlin RJ, Cohen MM, Levin LS. Syndromes affecting the central nervous system. In Gorlin RJ et al Syndromes of Head and Neck. 3rd edition. New York: Oxford University Press; 1990. p. 608-10.
6. Guo B, Jaovisidha S, Sartoris DJ, Ryu KN, Berthiaume MJ, Clopton P, Brossman J, Resnick D. Correlation between ossification of the stylohyoid ligament and osteophytes of the cervical spine. J Rheumatol 1997;24:1575-81.
7. Chouvel P, Rombaux P, Philips, Hamoir M. Stylohyoid chain ossification: choice of the surgical approach. Acta Otolaryngol. Belg 1996;50:5761.
8. Bafaqeeh SA. Eagle's syndrome: classic and carotid types. J Otolaryngol 2000;29:88-94.
9. Keur JJ, Campbell JPS, Mccarthy JF. The clinical significance of the elongated styloid process. Oral Surg. Oral Med Oral Pathol 1986;61:399-404.
10. Soh KB. The glossopharyngeal nerve glossopharyngeal neuralgia and the Eagle's syndrome: current concepts and management. Singapore Med. J 1999;40:659-65.
11. Kunachak S. Anterior cervical pain syndromes: hyoid thyroid and cricoid cartilages syndromes and their treatment with triamcinolone acetonide. The J Otol Laryngol 1995;109:49-52.
1 Master in Otorhinolaryngology and Head and Neck Surgery, UNIFESP-EPM. Assistant Physician, Sector of Head and Neck Surgery, Service of Otorhinolaryngology, HSPE-FMO-São Paulo/SP. Assistant Physician, Service of Otorhinolaryngology, HSPM São Paulo/SP.
2 Doctorate studies under course, Post-Graduate Course on Otorhinolaryngology and Head and Neck Surgery, UNIFESP-EPM.
3 Master studies under course, Post-Graduate Course on Otorhinolaryngology, Medical School of Santa Casa de São Paulo.
4 Resident Physician, Service of Otorhinolaryngology, HSPM São Paulo/SP.
Affiliation: Sector of Head and Neck Surgery, Service of Otorhinolaryngology, Hospital do Servidor Público Estadual - Francisco Morato de Oliveira
São Paulo/SP. Service of Otorhinolaryngology, Hospital do Servidor Público Municipal, São Paulo/SP.
Address correspondence to: Romualdo S. L. Tiago - Rua Estado de Israel 493, ap 51 - Vila Clementino - São Paulo CEP 04022-001 - Tel. (55 11) 5084.7725 - E-mail: romualdotiago@uol.com.br
Article submitted on November 26, 2001. Article accepted on January 17, 2002.