Year: 2003 Vol. 69 Ed. 2 - (21º)
Relato de Caso
Pages: 279 to 282
Nasolabial bilateral cyst: two case report and a review of the literature
Author(s):
José A. de P. Felix[1],
Paulo J. F. Ferreira[2],
Rodrigo Correa[3],
Rodrigo Cantini[4],
Rosalvo M. Neto[5],
Felippe Felix[6]
Keywords: nonodontogenic cyst, nasolabial cyst
Abstract:
The nasolabial cyst is an uncommon midfacial lesion. Its bilateral occurrence is extremely rare. Few cases ara described in the literature. This clinical manifestation represents the most important criterion for diagnosis. Therapy consists of surgical removal using an intraoral approach. The authors present two cases of bilateral nasolabial cysts, both in middle aged females, and a review of the literature is included.
![]()
Introduction
Nasolabial cysts were originally described by Zuckerkandl in 1882. It is a rare embryonic cyst, non-odontogenic, originated from the upper lip region right below the nasal ala. It is named nasoalveolar cyst, nasal vestibule cysts and nasal mucoid cysts, but the main denomination is nasolabial cyst, created by Rao in 1955, and currently considered the most appropriate one1.
The occurrence of this type of lesion is uncommon and bilateral presentation is extremely rare2. Few bilateral cases have been documented in the literature. Most of the time they are unilateral, but in 10% of the cases the presentation is bilateral3. The first authors to report cases of bilateral nasolabial cysts were Kofler in 1916 and Terracol in 19364.
The purpose of the present study was to report two cases of bilateral nasolabial cysts, one diagnosed concomitantly and the other diagnosed at different times, in addition to reviewing the literature on the topic.
CASE REPORT 1
Female 43-year-old patient, from Ceara state, presented complaint of size and pain close to the right nasal fossa followed by nasal obstruction, in July 1998. She reported that swelling had been in place for 1 year and progressively increased.
Upon conducting the physical ENT examination, we detected a painful increase of hard consistency, fluctuating with normal color, measuring approximately 2.5cm followed by right nasal ala elevation and effacement of the corresponding nasolabial groove (Figure 1). We ordered simple paranasal sinuses x-ray and it was not possible to identify the lesion. We conducted clinical topographic diagnosis of nasolabial cyst and indicated surgical procedure. It is important to point out that the left side had no impairment.
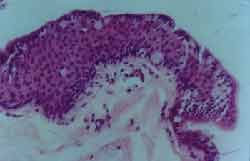
The patient underwent surgical resection under general anesthesia in September 1998 via intraoral access. A gingivolabial incision was made, between the central incisor and the first right upper molar, removing the lesion by open resection. The cyst had approximately 2.5cm with yellowish secretion inside it. Histology showed cystic fibrosis wall with lumen lined with cylindrical pseudo-stratified epithelium involving muco-secretory goblet cells; in two areas the metaplastic squamous epithelium forced the cylindrical epithelium, leading to atrophy (Figure 2). Five-month postoperative follow-up was asymptomatic.
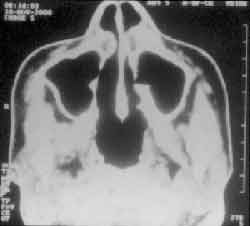
In March 2000, she came back and reported that as of December 1999, she detected a similar growth on the left side. In the ENT examination, we found a cystic tumor of approximately 2cm on the left nasolabial groove (Figure 3). We ordered paranasal sinuses CT scan that showed rounded tumor in the left nasal vestibule restricted to the soft parts of the pre-maxillary region (Figure 4).
The patient was submitted to surgical exeresis of the new cysts in September 2000. The clinical pathology showed similar aspects to the previous one. There was good progression in the 6-month postoperative follow-up.
CASE REPORT 2
Female 31-year-old patient, born and living in Guapimirim (RJ), whose main complaint was a "lump in the nose". She reported onset of the tumor on the left nasal fossa floor 2 years before with progressive increase in size, starting to bulge the right nasal fossa floor (Figure 5). She did not report pain, epistaxis, rhinorrhea or nasal obstruction. Upon physical ENT examination she presented bulging of both nasal fossae, larger on the left, with not phlogistic signs, occupying approximately 30% of the left nasal fossa and 20% of the right nasal fossa; in addition, there was effacement of the bilateral nasolabial groove.
We ordered paranasal sinuses CT scan that showed material with soft part density occupying the floor of both nasal fossae, organized in rounded shape (Figure 6). Nasal endoscopy confirmed bulging on the floor with diagnosis of bilateral nasolabial cysts.
She was submitted in April 2001 to surgical removal of the nasal cysts (Figure 7). The clinical pathology showed that both cystic formations were similar among each other and those in Case 1. The 5-month postoperative follow-up was uneventful.
Figure 1. Tumor on the right nasal ala region.
Figure 2. Squamous epithelium metaplasia area lining he cyst lumen, with identification of some goblet cells (H. E. 200x).
Figure 3. Tumor on the left nasal ala.
Figure 4. Paranasal sinuses computed tomography showing rounded tumor mass on the left nasal vestibule restricted to soft parts of the pre-maxilla regions.
Figure 5. Tumor on the right and left nasal ala regions.
Figure 6. Paranasal sinuses computed tomography scan showing material with soft tissue density occupying the floor of both nasal fossae.
Figure 7. Surgical exposure of both nasolabial cysts.
Discussion
Maxillary cysts are divided into inflammatory and embryonic and the latter ones are odontogenic or non-odontogenic.
In the literature, there is much discussion on the origin of cysts. In 1913, Klestadt suggested that such cysts were derived from ectodermic debris (embryonic facial groove epithelium) in the fusion line between medial and lateral nasal processes with the maxillary process; for this reason, they are called fissures 3, 5, 6. The other theory to explain the genesis of such cysts was developed by Bruggemann (1920) saying that it would be derived from the nasolachrymal duct epithelium (anterior-inferior) during the embryonic development 5-7. The epithelium that recovers the duct is pseudo-stratified columnar, similar to what is frequently observed in the nasolabial cyst wall4-6. In the present study, all lesions presented this epithelial lining. Both theories are anatomically valid4.
The female: male ratio for bilateral cysts is 5.5:1 and for unilateral, 3.5:18. The lesion is more frequent in Black people3, 9, 10 and frequently they are in the 4th and 5th decades of life7, 9, 11. They are normally unilateral (90%) and bilateral in only 10% of the cases3, 9.
Clinically, they are characterized by the presence of tumefaction of slow growth on the inferior ventral portion of the pyriform region, anterior to the maxillary bone and bulging of the nasolabial groove, as well as nasal obstruction, and dentition remains unaffected6. It occasionally causes pain in the presence of infection (50% of the cases), being that in such situations it can drain both in the nasolabial groove and in the oral cavity6, 11.
The diagnosis of nasolabial cysts is essentially clinical. Exploration by two-digit palpation shows a fluctuating tumefaction between the nasal vestibule floor and the gingivolabial groove and it helps confirm the diagnosis6. Since it is a soft tissue lesion, it is not detected by simple x-ray, except if it causes significant bone erosion of the maxillary bone. Computed tomography can show the cystic nature of the lesion and its relation with nasal ala and maxillary bone as the most common bone affection. Normally, the patient seeks for medical treatment after detecting facial deformity. In some cases, the diagnosis can be unexpectedly made in a routine ENT examination.
The lesion has slow growth and variable dimensions (2-3cm)3, however, there has been a report of a giant cyst from which they drained 250ml9.
Differential diagnosis has to be made with other cysts of the maxillary region and other nasal masses10. Infected nasolabial cysts can be mistaken for furunculum of the nasal vestibule floor. But except for this entity, the characteristics of the lesion are very different from others and there are no questions concerning the correct diagnosis.
Histopathology analysis of the lesion was described for the first time by Brown-Kelly in 189812. The cysts consist of respiratory epithelium (cylindrical ciliated pseudo-stratified or stratified with goblet cells), but there may be squamous metaplasia or infected cysts6. The fluid contained in the cysts is produced by the goblet cells.
Owing to the progressive facial deformity, the risk of infections and sequelae and pain manifestations in the region, the patient should be informed about the need for surgical removal. The procedure is simple enucleation through intraoral access, with gingivolabial groove incision (Denker) and open dissection of the lesion. The walls are closely related with the mucosa of the nasal vestibule floor and in most situations, it causes its laceration. We should conduct sutures with absorbable threads to prevent the development of oronasal fistula. The recurrence is rare and prognosis is excellent5, 7. It is a benign pathology and there is only one report by Arnold (1929) of carcinomatous degeneration of a nasolabial cyst 8,13.
CLOSING REMARKS
Nasolabial cysts are many times underdiagnosed in the initial steps. The physical and topographic examination is the preferred method for the diagnosis, followed by imaging exams with computed tomography. The best treatment approach is total exeresis of the lesion using sublabial intraoral incision at the incisor fossa level, which provides wide exposure and complete removal.
References
1. Fanibunda KB. Bilateral nasolabial cysts: a case report. Dent Pract 1970;20: 249-250.
2. Brandão GS, Ebling H, Souza IF. Bilateral nasolabial cyst. Oral Surg 1974;37:480-484.
3. Barzilai M. Bilateral nasoalveolar cysts: case report. Clin Radiol 1994;49(2): 140-141.
4. Waldrep AC, Capodanno JÁ. Bilateral nasolabial cysts: report of case. J Oral Surg 1966;24:347- 350.
5. Graamans K. Nasolabial cysts: diagnosis mainly based on topography?. Rhinology 1983;21: 239-249.
6. Kuriloff DB. The nasolabial cyst-nasal hamartoma. Otolaryngol Head Neck Surg 1987;96:268-272.
7. David VC, O´Connell JE. Nasolabial cyst. Clin Otolaryngol 1986;11:5-8.
8. Roed-Peterson B. Nasolabial cysts: a presentation of five patients with a review of literature. Br J Oral Surg 1969;7:84- 95.
9. Cohen MA, Hertzanu Y. Huge growth potential of the nasolabial cyst. Oral Surg 1985;59:441-5.
10. Karmody CS, Gallagher JC. Nasoalveolar cysts. Ann Otol 1972;81:278-283.
11. Allard RHB. Nasolabial cysts: review of the literature and report of seven cases. Int J Oral Surg 1982;11:351-359.
12. Burtschi TA, Stout RA. Bilateral nasoalveolar cysts. Oral Surg 1963;16: 271-275.
13. Egervary G, Csiba A. Bilateral nasolabial cyst. Dental Digest 1969;75:504-7.
14. Walsh-Warine GP. Nasoalveolar cysts: aetiology, presentation and treatment. J laryngol Otol 1967;81:263-273.
15. Rao RV. Nasolabial cyst. J Laryngol Otol 1955;69:352-4.
1 Joint Professor, Discipline of Otorhinolaryngology, Medical School, Universidade Federal Fluminense.
2 Assistant Professor, Discipline of Otorhinolaryngology, Medical School, Universidade Federal Fluminense.
3 Graduate studies in course, Discipline of Otorhinolaryngology, Medical School, Universidade Federal Fluminense.
4 Graduate studies in course, Discipline of Otorhinolaryngology, Medical School Universidade Federal Fluminense.
5 Graduate studies in course, Discipline of Otorhinolaryngology, Medical School Universidade Federal Fluminense
6 Undergraduate, Medical School, Universidade Federal Fluminense.
Address correspondence to: José Antonio de Paula Felix - Rua Cel. Moreira César 229, sala 1815 24230-053 Icaraí, Niterói RJ
Tel/fax: (55 21) 2710-6220 - E-mail: felfelix@cruiser.com.br
Study presented at 2º Congresso de Otorrinolaringologia, Universidade de São Paulo.
Article submitted on May 24, 2002. Article accepted on June 10, 2002.