Year: 2003 Vol. 69 Ed. 3 - (7º)
Artigo Original
Pages: 333 to 336
Acoustic rhinometry evaluation of nasal cavity and nasopharynx before and after adenoidectomy
Author(s):
Carlos E. N. Nigro[1],
Elder Goto[1],
Josiane F. A. Nigro[1],
Joao F. M. Junior[2],
Olavo Mion[2],
Richard L. Voegels[3]
Keywords: adenoidectomy, acoustic rhinometry.
Abstract:
Introduction: The authors evaluate the minimum cross-sectional area (MCA) and nasal volume (NV) of the nasal cavity and nasopharynx before and after adenoidectomy. Study Design: Clinical prospective.
Aim: Evaluate changes of nasal cavity and nasopharynx before and after adenoidectomy using objective technique for assessment the nasal patency, acoustic rhinometry. Material and Method: Twenty-three children (52 nasal cavities) with surgical indication for adenoidectomy were evaluated with acoustic rhinometry before and 15 days after surgery. Results: The MCA of nasal cavity changed, before decongestion, from 0,73 cm2 preoperatively into 0,79 cm2 postoperatively and after decongestion, from 0,87 cm2 preoperatively into 0,93 cm2 postoperatively. The volume of nasal cavity changed, before decongestion, from 6,18 cm3 preoperatively into 6,47 cm3 postoperatively and after decongestion, from 8,31 cm3 preoperatively into 8,65 cm3 postoperatively. The MCA of nasopharynx changed, before decongestion, from 2,43 cm2 preoperatively into 2,69 cm2 postoperatively and after decongestion, from 2,76 cm2 preoperatively into 3,79 cm2 postoperatively. The volume of nasopharynx changed, before decongestion, from 5,57 cm3 preoperatively into 6,14 cm3 postoperatively and after decongestion, from 6,51 cm3 preoperatively into 8,78 cm3 postoperatively. Conclusion: The increase of MCA and volume of the nasopharynx agree with the improvement of the symptoms that patients or parents reported after adenoidectomy.
![]()
INTRODUCTION
"Adenoid vegetation" was first described by Meyer in 1870 in his study in which he described digital palpation method as a major diagnostic tool and also described the limitations of posterior rhinoscopy 1. Recent studies evidenced the efficacy of nasofibroscopy in adenoid hypertrophy detection, however, it is an invasive method but it offers many advantages against simple X ray in profile 2. Symptoms mentioned by parents were a key source of information for the definition of adenoidectomy 3.
Some assertions have been made regarding acoustic rhinometry (AR) potential for the detection and outcome of patients with adenoid hypertrophy, although many studies have evidenced low accuracy of AR in reflecting actual anatomic status of nasopharynx due to technical limitations of the technique itself. 5,6.
The occurrence of occlusion of upper airways in patients with pharyngeal tonsil hypertrophy followed or not by palatine tonsil hypertrophy is commonly seen in ENT clinical practice sometimes associated with hypertrophy of inferior conchae.
The objective of this study was to analyze changes in geometry of nasal and nasopharynx cavities that occurred in children that have undergone adenoidectomy associated or not with palatine tonsillectomy. Acoustic rhinometry was conducted pre and postoperatively to check changes in volume and minimal cross-sectional area (MCA) of nasal fossae and to find out what occurs with volume and minimal cross-sectional area of nasopharynx where the pharyngeal tonsil is located.
CASE STUDY AND METHOD
This study was approved by the Ethics Committee of Clinical Hospital of the Medical School of the University of Sao Paulo and those responsible for the pediatric patients signed an informed consent term authorizing the performance of Acoustic Rhinometry Examination.
Thirty-three pediatric patients (66 nasal cavities), 16 boys and 17 girls, with surgical indication for adenoidectomy with or without palatine tonsillectomy, underwent Acoustic Rhinometry before surgery and 15 days after surgery to assess changes in geometry of nasal and nasopharynx cavities.
All patients had symptoms of upper airway obstruction: mouth breathers most of the day (96%), daily snoring (69%), apnea events (15%), recurrent media otitis (11%) and adenoid hypertrophy confirmed by nasofibroscopy or radiological exam.
This study excluded patients that had undergone previous nasal or pharyngeal surgery; with symptoms and/or signs of allergic rhinitis or sinus disease at the moment of Acoustic Rhinometry exam; the same applied to severe septum deviation in former rhinoscopy and choanal atresia.
Twenty-three patients returned 2 weeks postoperatively for the performance of a new Acoustic Rhinometry - 9 boys and 14 girls aged 3 to 10 years old, mean age of 6.1 years. Acoustic Rhinometry was performed 3 times in each nostril before and 15' after the application of 3 sprays of Oximethalozin Chloridrate (Vasoconstrictor) applied topically on the nose and performed according to the standard advocated by Hilberg et al. 7; tracing that showed obvious artifact were discarded. Acoustic rhinometer used was the Eccovision Acoustic Rhinometry (Laboratório Hood).
Minimal Cross-sectional Area (MCA) and nasal volume were measured in the first 5 cm from the nostril since this region provides increased reliability for the exam 8, additionally, we measured nasopharynx MCA and volume represented in the nasal rhinogram as the X axis from 6.5 to 8.5 cm from the nostril9.
MCA and volume of both nasal fossae were added up to mitigate measurement failures due to structural alterations or nasal cycle.
Every patient had his or her nasal cavity and nasopharynx MCA and volume checked before preoperative and postoperative application of Vasoconstrictor. For purposes of comparison of such values the Student's t test was used for paired samples.
RESULTS
All patients or their tutors mentioned subjective improvement of obstruction symptoms of upper airways such as mouth breathing, snoring and/or apnea.
In nasal fossae MCA, before application of VC, ranged from 0.73 ± 0.17 cm2 (0.46 - 1.18) preoperatively to 0.79 ± 0.20 cm2 (0.47 - 1.22) postoperatively; p < 0.01. After the application of VC it ranged from 0.87 ± 0.24 cm2 (0.49 - 1.41) preoperatively to 0.93 ± 0.24 cm2 (0.60 - 1.47) postoperatively; p < 0.01. The volume of nasal fossae before application of VC ranged from 6.18 ± 1.42 cm3 (3.84 - 9.35) preoperatively to 6.47 ± 1.60 cm3 (4.12 - 10.10) postoperatively; p < 0.05. After application of VC it ranged from 8.31 ± 2.10 cm3 (4.23 - 12.70) preoperatively to 8.65 ± 2.08 cm3 (4.42 - 12.02) postoperatively; p < 0.05.
In the nasopharynx the MCA before application of VC ranged from 2.43 ± 1.06 cm2 (1.10 - 4.81) preoperatively to 2.69 ± 1.19 cm2 (1.09 - 5.35) postoperatively; p < 0.05. After application of VC it ranged from 2.76 ± 1.15 cm2 (1.08 - 4.88) preoperatively to 3.79 ± 1.69 cm2 (1.55 - 7.12) postoperatively; p < 0.001. Nasopharynx volume before application of VC ranged from 5.57 ± 2.33 cm3 (2.45 - 10.99) preoperatively to 6.14 ± 2.48 cm3 (2.43 - 11.62) postoperatively; p < 0.01. After application of VC it ranged from 6.51 ± 2.61 cm3 (2.70 - 11.48) preoperatively to 8.78 ± 3.40 cm3 (3.61 - 14.48) postoperatively; p < 0.001.
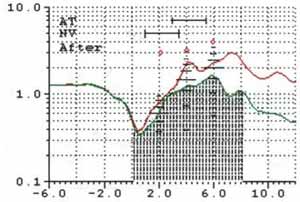
Figure 1 exemplifies the changes in area and volume of nasal fossae and nasopharynx after application of nasal VC.Figure 1. Nasal rhinogram before vasoconstriction (inferior) and after it (superior) after adenoidectomy.
DISCUSSION
The objective of this study was to investigate changes in geometry of nasal fossae and nasopharynx through Acoustic Rhinometry before and after adenoidectomy. In nasopharynx the increase of MCA and volume was highly significant after application of vasoconstrictor.
Kim et al.10, to determine the adenoidectomy effect in the geometry of nasal cavity and nasopharynx, performed Acoustic Rhinometry preoperatively and 15 days after surgery, before and after topical application of vasoconstrictor. The rhinogram before the application of vasoconstrictor pre and postoperatively showed an increase in MCA region of the apex of the inferior concha and in nasal fossae volume; after decongestion of mucosa there was an increase of MCA only in the nasopharynx, similarly to the results found in our study.
Cho et al.4 concluded after evaluating nasopharynx through Acoustic Rhinometry pre and postoperatively and comparing with findings in other control group that MCA and nasopharynx volume are significantly lower in groups of patients with hypertrophy adenoid with significant increase of nasopharynx MCA and volume after surgery.
Mostafa11 found significant increase in nasopharynx MCA and volume after adenoidectomy and concluded that Acoustic Rhinometry could be used as screening method and if there is high suspicion of adenoid hypertrophy, endoscopy could be planned.
Riechelmann et al.9 compared nasopharynx of children with preoperative adenoid hypertrophy and after adenoidectomy surgery against a control group of children without adenoid hypertrophy and found that pre and postoperatively nasopharynx MCA differences were not statistically significant even if compared with the MCA of the control group.
Fisher et al.12 stated that Acoustic Rhinometry does not have accuracy to evidence small alterations in nasopharynx volume and concluded that Acoustic Rhinometry has little predictive value if used alone to evaluate the presence of hypertrophy adenoid; it will have higher predictive potential if used jointly with clinical picture of the patient.
In the nasopharynx, we found an increase of MCA and nasal volume after removing adenoid tissue. Such increase was higher if we compare these measures after using a topical nasal decongestant, probably due to easy propagation of sound waves reflected by reduction of sound volume in erectile tissues of nasal fossae.
Exams performed preoperatively could undersize nasal geometry due to the likelihood of secretion stasis in nasal fossae of mouth breathing children even after we requested them to clean up their noses.
Although Acoustic Rhinometry had decreased level of precision for measuring nasopharynx size due to the presence of severe obstruction in the past causing underestimation of posterior region, the voluntary and involuntary movements of soft palate, sound leakage to the opposite nasal fossae and the physical limitations of the technique itself 5, 12, 14, 15, it was able to evidence the MCA gain and pervious volume in the postoperative nasopharynx.
CONCLUSIONS
The increase of nasopharynx MCA and volume indicating improvement of nasal permeability matched the improvement of obstructive symptoms mentioned by patients and family members after adenoidectomy.
REFERENCES
1. Meyer, W. On adenoid vegetations in the naso-pharyngeal cavity: their pathology, diagnosis and treatment. Med Chir Trans 1870; 53: 191 - 215 apud FISHER, E. W. et al. Acoustic Rhinometry in the Pre-operative Assessment of Adenoidectomy Candidates. Acta Otolaryngol (Stockh) 1995; 115: 815 - 822.
2. Monteiro E. C. M., Pilon R.R., . Dall, Oglio G. P. Estudo da hipertrofia adenoideana: endoscopia x radiografia de nasofaringe. Rev. Bras. Otorrinolaringologia 2000; 66 (1): 9-12.
3. Hibbert, J.; Tweedie, M. C. K. The value of signs and symptoms in the diagnosis of enlarged adenoids. Clin Otolaryngol 1977; 2: 297 - 304 apud FISHER, E. W. et al Acoustic Rhinometry in the Pre-operative Assessment of Adenoidectomy Candidates Acta Otolaryngol (Stockh) 1995; 115: 815 - 822.
4. Cho, J.; Lee, D.; Lee, N.; Won, Y.; Ion, H., Suh, B. Size assessment of adenoid and nasopharyngeal airway by acoustic rhinometry in children. J. Laryngol. Otol. 1999; 113: 899 - 905.
5. Tomkinson, A.; Phil, M.; Eccles, R. The identification of the potential limitation of acoustic rhinometry using computer-generated, three-dimensional reconstructions of simple models. Am. J. Rhinol. 1996; 10: 77 - 82.
6. Buenting, J.E.; Dalston, R.M.; Smith, T.L.; Drake, A.F. Artifacts associated with acoustic rhinometric assessment of infants and young children: a model study. J. Appl. Physiol. 1994; 77 (6): 2558 - 2563.
7. Hilberg, O.; Pedersen, O.F. Acoustic rhinometry: recommendations for technical specifications and standard operating procedures. Rhinol. Supp. 2000; 16: 03 -17.
8. Hilberg, O.; Pedersen, O.F. Acoustic rhinometry: influence of paranasal sinuses. J. Appl. Physiol. 1996; 80: 1589 - 1594.
9. Riechelmann, H.; Connel, J.M.; Rheinheimer, M.C.; Wolfensberger, M.; Mann, W.J. The role of acoustic rhinometry in the diagnosis of adenoidal hypertrophy in pre-school children. Eur. J. Pediatr. 1999; 158: 38 - 41.
10. Kim, Y.; Kang, J.; Yoon, K. Acoustic rhinometric evaluation of nasal cavity and nasopharynx after adenoidectomy and tonsillectomy. Int. J. Pediatr. Otorhinolaryngol. 1998; 44: 215 - 220.
11. Mostafa, B. E. Detection of adenoidal hypertrophy using acoustic rhinomanometry. Eur Arch Otorhinolaryngol 1997; 254 (suppl. 1): S27 - S29.
12. Fisher, E.W.; Palmer, C.R.; Daly, N.J.; Lund, V.J. Acoustic rhinometry in the pre-operative assessment of adenoidectomy candidates. Acta Otolaryngol. (Stockh.) 1995; 115: 815 - 822.
13. Silkoff, P. E. et al. Reproducibility of Acoustic Rhinometry and Rhinomanometry in Normal Subjects. Am. J. Rhinol. 1999; 13: 131 - 135.
14. Hilberg, O.; Jackson, A. C.; Swift, D. L.; Pedersen, O. F. Acoustic rhinometry: evaluation of nasal cavity geometry by acoustic reflection. J.Appl. Physiol. 1989; 66: 295 - 303.
15. Lenders, H.; Pirsig, W. Diagnostic value of acoustic rhinometry: patients with allergic and vasomotor rhinitis compared with normal controls. Rhinology. 1990 28 (1): 5 - 16.
1 Ph.D. studies under course, Discipline of Otorhinolaryngology, HCFMUSP.
2 Ph.D., Assistant Professor, Discipline of Otorhinolaryngology, HCFMUSP.
3 Ph.D., Associate Professor, Discipline of Otorhinolaryngology, HCFMUSP.
Study conducted at the Division of Clinical Otorhinolaryngology, Hospital das Clínicas, FMUSP.
Address correspondence to: Dr. Carlos Eduardo N. Nigro - Rua Prof. Luiz Augusto da Silva, 67, centro, CEP: 12020-360, Taubaté , SP, Brazil - E-mail: otorrinoclinica@uol.com.br