Year: 2005 Vol. 71 Ed. 2 - (19º)
Relato de Caso
Pages: 237 to 240
Nasal paraganglioma: a case report
Author(s): Mauren P. Rocha1, Andréa M. Campagnolo1, Vanessa S. Macedo1, Fabiana B. Scarton2, Henrique P. Rocha3, Gabriel Kuhl4
Keywords: nasal paraganglioma, nasal cavity, nasal tumour.
Abstract:
Paragangliomas arise from paraganglionic tissue of the autonomic nervous system. Paragangliomas of the head and neck region are rare. The most common sites of origin of this neoplasm in the head and neck region are the carotid body, the jugular bulb and the vagal body. Paragangliomas of the nose and paranasal sinuses are very uncommon. The authors referred about one case of nasal paraganglioma in a 45-year-old male patient, who was submitted to surgical excision, and discuss the clinical findings, diagnostic criteria, treatment, prognosis and literature review. The importance of reporting this case refers to the rarity of paragangliomas located in the nasal cavity and paranasal sinuses.
![]()
Introduction
Paragangliomas are neoplasias arising from paraganglionic tissue of the autonomic nervous system. Paraganglions are of neuroectodermal origin and present two types of cells: Type I, which contain catecholamine granules; Type II, which are supportive cells similar to Schwann cells surrounding type I cells1.
Paraganglions are broadly distributed in the human body, found in the lungs, heart, mediastinum, gastrointestinal tract, retroperitoneal region and bladder. In the head and neck, they were found in trachea, tongue, larynx, hypophysis, pineal gland and orbit. Despite these findings, the most prevalent sites of paragangliomas are the carotid body, jugular body, along glossopharyngeal nerve and its tympanic branch, and the vagus nerve, especially next to nodal ganglion 2.
This study reports a case of nasal paraganglioma in a 45-year-old male patient due to the rare aspect of such clinical condition at this specific site.
Literature Review
Head and neck paragangliomas are very rare, with an incidence of 0.0012%3. In general, they are symptomatic tumors, which may be clinically taken for other benign or malignant lesions3. Paragangliomas are not uncommonly diagnosed as glomic tumors, as they both present intense vascularization4, regardless of being immune and histologically distinct. Types most frequently found are the carotid (carotid body), jugular (jugular bulb) and vagal (vagal nerve)5.
The site of origin of nasal paragangliomas remains unknown. Many authors suggest the existence of paraganglionic tissue in the pterygopalatine fossa, based on paraganglions' close relationship with arteries and cranial nerves. However, among the cases previously reported in literature, the majority was found in the regions of ethmoidal middle concha or ethmoidal sinus1.
Case Report
J.C., a 45-year-old Caucasian man searched for medical care complaining of nasal obstruction for one year. He also referred chronic nasal secretion with periods of purulent rhinorrhea. No bleeding, pain or facial edema was reported.
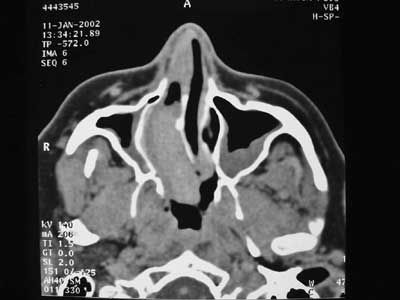
At otolaryngological examination, previous rhinoscopy showed a polyploid mass in the right nasal fossa. Fibroscopy revealed a lesion in the right nasal fossa obstructing the ipsilateral choanal portion. Computed tomography scan (CT) presented a lesion with dense soft tissues in the right nasal cavity (Figure 1). Incisional biopsy was performed under local anesthesia revealing a nasal paraganglioma. After previous embolization of the maxillary artery by arteriography (Figure 2), the patient was submitted to surgery with transoperative freezing process, on January 16th 2002, when total excision of lesion was carried out. Both the clinical pathology and final examinations confirmed the presence of a nasal paraganglioma. No immediate or late postoperative complications were observed. After 5 months of surgery, the patient was asymptomatic and attending outpatient follow-up. So far, he has not showed evidences of relapses.
Discussion
Paragangliomas of the nose and of paranasal sinuses are very infrequent. According to a study comprising 73 cases of head and neck paragangliomas, only 3 were of nasal and paranasal types2. An updated literature review demonstrated only 22 cases of paragangliomas on that anatomical site1.
Nasal paraganglioma is a slow-growing neoplasia, with a time interval between symptoms' onset and diagnosis of 2 or more years5. There is a well-defined and natural tendency towards multicentricity. Many synchronic tumors are incidentally revealed during arteriography. Usually, incidence of bilaterality and multicentricity of these tumors are of 3%, going up to 26% among patients with positive family history, which corroborates family predisposition6.
Clinical expression is recurrent episodes of mild to profuse epistaxis, rhinorrhea, nasal obstruction and facial edema, which may be followed by blurred vision3,5. In general, this neoplasia presents with a polyploid mass fixed to the lateral wall of the nasal fossa or on the upper region of the rhinopharyngeal roof3. In some cases, the paranglioma extends to the paranasal sinuses, with erosion of bone walls5.
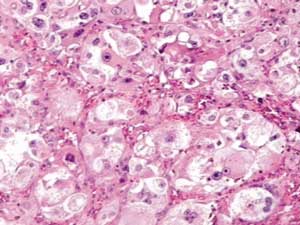
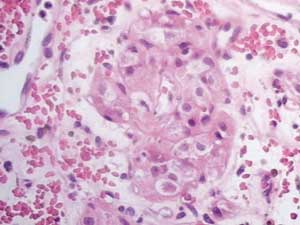
Macroscopically, paragangliomas are hard lesions of grayish or rosy color and with encapsulated aspect3. Histologically, these neoplasias are peculiarly formed by epithelioid cells with round nuclei and eosinophilic cytoplasm, forming nests called zellballen which are separated by a rich capillary net of reticulin (Figure 3)1,5,7. Electronic microscopy revealed the presence of cytoplasmatic neurosecreting granules in these cells of the cytoplasm 1. Some benign neoplasias present cell pleomorphism and nuclear hyperchromic aspect, including mitotic figures, which leads many authors to assume the presence of bone invasion or distant metastases in the establishment of malignancy diagnosis 1.
Assessment and diagnosis of nasal paragangliomas must include computed tomography, nuclear magnetic resonance and arteriography with investigation of the venous phase. Arteriography also allows evaluation of collateral circulation. Tumor extension and its relation with vascular structures of the neck and skull base should be established6.
Use of special histological staining is important to demonstrate neurosecreting cytoplasmatic granules 3. Histological analysis samples may be successfully obtained by means of incision biopsy of lesion, as demonstrated by Lack et al3. In this research study, incision biopsy provided a diagnosis of all cases of nasal (3), carotid (3), jugular (7) and orbital (1) paragangliomas, to which this technique was applied3.
Considering that paragangliomas present tendency towards progressive invasion of vital structures - leading to morbidity -, and also count on improved surgical techniques available, surgical excision with disease-free borders remains the treatment of choice for these neoplasias3. However, paragangliomas tend to locally relapse due to its nature and localization1. Radiotherapy for the treatment of paragangliomas is reported in the literature, but with variable results. Many authors reported an appropriate disease control with radiotherapy, although not reaching the cure. Thus, this therapeutic approach is reserved for patients without surgical indication or those with inadequate tumor excision. Chemotherapy was clearly ineffective in the treatment of paragangliomas. Embolization has been primarily used to restrict blood volume during surgery1,8.
Paragangliomas may occur as the syndrome of multiple endocrine neoplasia (MEN) combined with medullar carcinoma of thyroid gland and, optionally, as pleochromocytoma. In such cases, endocrine evaluation and magnetic nuclear resonance of the adrenal, thoracic and neck regions are necessary for an appropriate therapeutic strategy9.
Malignant head and neck paragangliomas show an incidence of 4 to 19%1. Metastases are rare and are found in 9% of the cases4. Literature reports show that metastases tend to involve lymph nodes, lungs and bones2. It is widely accepted that malignancy potential of paragangliomas cannot be estimated by lesions' histological aspect only2. Not only histological findings suggestive of potential malignant behavior - such as mitotic figures, nest necrosis and vascular invasion - should be considered, but also an accurate assessment of paragangliomas presenting uncommon infiltrating growth or recurrences4,10 should be performed. Such neoplasias should be submitted to aggressive surgical resections, once they are strongly characteristic of malignant behavior1. However, an aggressive intervention on these specific cases may not always lead to good results, as prognosis of patients with malignant paragangliomas are normally reserved, regardless of the lesion's site1.
Closing Remarks
The rare occurrence of paragangliomas of the nasal fossa has motivated our study. Once diagnosed, they should be treated surgically, considering its morbidity due to tendency towards progressive invasion of vital structures. However, even with adequate surgical approach, paragangliomas tend to present local relapse due to its nature and localization.
References
1. Nguyen Q, Gibbs P, Rice D. Malignant nasal paraganglioma: a case report and review of the literature. Otolaryngology - Head and Neck Surgery 1995; 113(1): 157-61.
2. Talbot A. Paraganglioma of the maxillary sinus. J Laryngol Otol 1990; 104: 248-51.
3. Lack E, Cubilla A, Woodruff J, Farr H. Paragangliomas of the head and neck region: a clinical study of 69 patients. Cancer 1977; 39: 397-409.
4. Battiata B, Vander W, Adair C, Mair E. Quiz case. Archives of Otolaryngology - Head and Neck Surgery 2001; 127(3): 329-30.
5. Himelfarb M, Ostrzega N, Samuel J, Shanon E. Paraganglioma of the nasal cavity. Laryngoscope 1983; 93: 350-2.
6. Mavez M, Carl Rusty. In: Bailey B, Healy G, Johnson J. Head & Neck Surgery- Otolaryngology, 3rd Edition. Philadelphia: Lippincott-Williams & Wilkins, 2001; p. 1562-73.
7. Kuhn J, Aronoff B. Nasal and nasopharyngeal paraganglioma. J Surg Oncol 1989; 40: 38-45.
8. Watson DJ. Nasal paraganglioma. J Laryngol Otol 1988; 102: 526-9.
9. Maier W, Marangos N, Laszig R. J. Laryngol Otol 1999; 113(11): 978-82.
10. Branham G, Gnepp D, O'Menomey S, Friedman W. Malignant paraganglioma - a case report and literature review. Otolaryngol Head Neck Surg 1989; 101: 99-103.