Year: 2004 Vol. 70 Ed. 6 - (26º)
Relato de Caso
Pages: 855 to 857
Chronic myeloid leukemia in association with squamous cell carcinoma of tonsillar region submitted to postsurgical irradiation
Author(s): Sergio Altino Franzi , Ali Amar1, Milena Mendes Incerti , Abrão Rapoport1, José Pedro Zampieri Filho , Andréia Gomes Monteiro
Keywords: Key words: squamous cell carcinoma, leukemia, tonsillar region.
Abstract:
Summary
Surgery and postoperative radiotherapy are the standard treatment of advanced squamous cell carcinoma of the tonsillar region and they are based in the specimen findings such margins, vascular embolization, perineural infiltration or metastatic lymph nodes. Apparently, the radiotherapy has the potential to bring malignant neoplasm, however this fact though is uncommon. We described a case of a 54-year-old Caucasian male with squamous cell carcinoma of tonsillar region treated by surgery and radiotherapy eleven years ago. After three years of follow-up he presented all of a sudden swoon and weakness. The laboratorial exam showed higher rate of leucocytes. The result of the myelogram showed as diagnostic a chronic myeloid leukemia. The patient received Hydroxyurea and soon after Interferon. After eight years of follow-up he had no evidence of disease.
![]()
Introduction
The treatment of choice for advanced squamous cell carcinoma of the tonsil consists of surgery and postsurgical radiotherapy. Indication of postsurgical radiotherapy is based on examination of the surgical specimen, taking into account the surgical margins, presence of neoplastic embolization, perineural infiltration or metastatic cervical lymph nodes, particularly if capsular rupture is identified.
Nicu1, Miller2 and Ilbery and Rickinson3 have related the carcinogenic effects to ionizing irradiation in human beings. Caquet4 conducted a study in which the effects of ionizing radiation as potential agent in the development of head and neck neoplasias were described. The study was based on a patient with laryngeal squamous cell carcinoma who was submitted to ionizing irradiation and developed a clinical case of chronic myeloid leukemia.
The anatomical sites which most frequently develop a second tumor within an estimated period of 10 years when exposed to ionizing radiation are: mouth, oropharynx, larynx and thyroid (Wang5, Jackson6).
Cases of squamous cell carcinoma of the tonsil that develop a second primary tumor in the form of chronic myeloid leukemia after being submitted to postsurgical radiotherapy are rare. A case of a clinical stage IVB squamous cell carcinoma of the right palatine tonsil submitted to postsurgical radiotherapy is presented below.
Case Study
A 54-year-old Caucasian male worker (contact with iron and aluminum as a boiler operator) was admitted to the Department of Head and Neck Surgery and Otorhinolaryngology of Hospital Heliópolis in November 1992 with complaint of slow-growth (5 months) lump on the neck and sore throat. The patient stated that there were no dysphasia, hoarseness, dyspnea, otalgia, personal or family history of cancer. Oroscopy revealed ulcerative-vegetative lesion with infiltration to the right tonsil, measuring 3 X 3 cm, limited to the anterior right pillar; then, the posterior pillar was also affected, involving the upper region of the soft palate as an erythroplastic lesion, 1cm distally from the uvula and preserving the lingual-tonsillar sulcus. A hard-consistency lymph node block in the neck - measuring 8.5 X 6.5 cm - involved the upper and the right middle jugular-carotid chains, presenting mobility at the deepest layers, though not affecting the skin. Moreover, the lesion was painless and with bosselated surface.
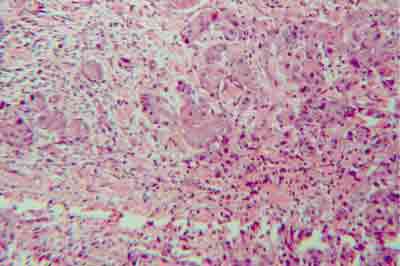
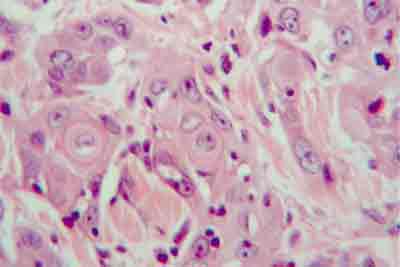
A biopsy of the primary site was performed, revealing clinical stage T2 N3 M0 well- differentiated squamous cell carcinoma (Figures 1-2). Furthermore, right-retromolar- type surgery was carried out. Due to posterior exiguous margin, the patient received a 5000-cGy postsurgical radiotherapy dosage on the cervical-facial fields, as well as on the supraclavicular fossa, in the period between October and November 1992.
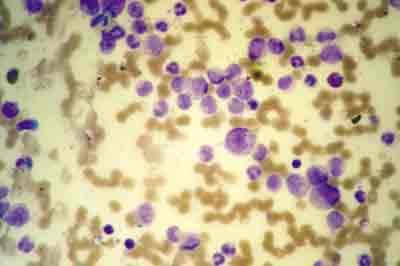
Three years later (1995), the patient presented hypothyroidism and was prescribed with Levothyroxine. Chronic myeloid leukemia was also diagnosed (Figures 3 and 4), which was treated with Hydroxyurea (20-30 mg/kg/day). The disease was controlled and the patient started taking Interferon - 6 million units/5x/week. In September 2003, the patient was well, with no symptoms nor evidence of disease (Figure 3).
Discussion
The knowledge that head and neck neoplasias submitted to ionizing irradiation may develop a lymphoreticular neoplasia is attributed to Hazen (1966) 7. This concept was reinforced by a study published by Nicu1, in which he reported the carcinogenic effects of irradiation in humans. Mays8 suggested that the onset of a second primary tumor could be related to "internal" radioactivity in the human economy.
In the mentioned case, the development of leukocytosis (around 78,000) after the third year of combined treatment led to the diagnosis of chronic myeloid leukemia, which was confirmed by a myelogram (Figures 3 and 4). Moreover, hypothyroidism was detected - a not-so-uncommon sequel when the thyroid is included in the irradiation field - and, as it presents only a few symptoms, it is usually diagnosed later.
Considering that squamous cell carcinoma of aerodigestive tract upper airways developing a second lymphoreticular primary tumor when submitted to postsurgical irradiation is a rare occurrence, a causal association is not considered. Although the causes are still under investigation, the risk of cancer induction by radiation has been corroborated by several epidemiological studies, in which translocations and loss of genetic material8 are the main cytogenetic changes described. Follow up of patients treated with radiotherapy should always take into consideration the potential rise of a second primary tumor as a result of the therapeutic modality employed.
References
1. Nicu MD. [Carcinogenic effect of radiations in humans]. Stud Cercet Endocrinol 1970; 21:19-29.
2. Miller RW. Radiation-induced cancer. J Natl Cancer Inst 1972; 49:1221-6.
3. Ilbery PL, Rickinson AB. Radiation carcinogenesis. Australas Radiol 1973; 17:66-77.
4. Caquet R, Festal G, Laroche C, LeCharpentier M, Bernadou A. [Letter: Cancer of the larynx. Radiotherapy-chronic myeloid leukemia].Nouv Presse Med 1975; 17: 20:1510.
5. Wang MB, Kuber N, Kerner MM, Lee SP, Juilliard GF, Abemayor E. Tonsillar carcinoma: analysis of treatment results. J Otolaryngol 1998; 27: 1221-7.
6. Jackson SM, Hay JH, Flores AD, Weir L, Wong LW, Schwindt C, Baerg B. Cancer of tonsil: the results of ipsilateral radiation treatment. Radiother Oncol 1999; 51:123-8.
7. Hazen RW, Pifer JW, Toyooka ET, Livingood J, Hempelmann LH. Neoplasms following irradiation of the head. Cancer Res 1966; 26: 305-11.
8. Mays CW. Cancer induction in man from internal radioactivity. Health Phys 1973; 25: 585-92.
Figure 1. Moderately differentiated squamous cell carcinoma (HE, 100X).
Figure 2. Moderately differentiated squamous cell carcinoma (HE, 400X) with evidence of keratin cells.
Figure 3. Peripheral blood smear, Leishmann stained (100X) presenting leukocytosis, neutrophilia with variable dysplasia and cells of different maturation grades.
Figure 4. Peripheral blood smear, Leishmann stained (400x) presenting high number of blasts. Neutrophils and monocytes of different maturation grades.