Year: 2004 Vol. 70 Ed. 6 - (21º)
Relato de Caso
Pages: 833 to 836
Trichilemmal carcinoma: A case study
Author(s): Marcos Antônio Nemetz , Regina Maria da Cunha , Priscilla Reeck2, Waldir Carreirão Neto2, Maria Teresa S. Moreira , Marina S. Coelho
Keywords: Key words: trichilemmal carcinoma.
Abstract:
Summary
Trichilemmal carcinoma is a malignant lesion of low degree, not so frequent, that originates from a hair follicle cell, being necessary a special diagnosis in relation to others skin carcinomas. The aim of this issue is to relate a case of trichilemmal carcinoma dealt in the sickroom of Otorrinolaringologia and Head and Neck Surgery from "Universidade Regional de Blumenau" in a male 86-year-patient, that had a lesion in a left supra-clavicle region with a year of evolution and progressive growth, measuring 75x45 mm, vegetate, hardened, reddish, with a central ulceration, blood secretion and local pain. The tumor was removed surgically with free limits. Due to the type of lesion generally nor develops metastases, neither has local recidivation, it was decided for not realizing concomitant therapy only periodical inquiring of the lesion.
![]()
Introduction
Trichilemmal carcinoma is an unusual malignant lesion, which, due to its rare incidence of recurrences or metastases, is considered a low malignancy carcinoma.
It originates from a hair follicle cell and differential diagnosis includes other skin carcinomas.
The present study reports a case of trichilemmal carcinoma found in an 86-year-old woman, in which we present the disease's features.
Literature Review and Differential Diagnosis
Trichilemmal (TLC) is a term formerly introduced by Headington in 1976, although it had not been adopted by pathologists1 for many years. Currently, the publication of different studies has greatly contributed to distinguish TLC from other groups of follicular tumors.
Trichilemmal carcinoma is a rare tumor that shows predilection for sun-exposed skin. It generally affects subjects aged 40 - 90 years old. The favorite occurrence sites are face, scalp, neck and back of hands2.
Van Vlotem et al. found a greater number of carcinomas in patients submitted to irradiation for benign diseases of the head and neck. According to the author, this lesion has long latency period and its prevalence is straightly related to a certain irradiation dosage to which the patients were submitted3.
Clinically, lesions usually appear as ulcerated or scabbed papules, lumps or plaques. Other features include a reddish - "color of flesh" - spot measuring around 0.5-2cm in its greater diameter2. It is usually a solitary lesion - multiple types are seldom reported3. Diagnosis may be determined by simple histology and/or immunohistochemistry of the lesion.
Histologically, the lesion is mainly an intraepithelial tumor or is most commonly associated with an invasive component, which may involve the epidermis up to the subcutaneous fat. In general, this lesion appears in continuity with the epidermis and/or follicular epithelium. In larger lesions, bleeding and/or necrosis are reported.
Immunohistochemistry reveals negative results for CEA and EMA, although there are reports of late positive cases2.
Differential diagnosis should be done with squamous cell carcinomas, basal cell carcinomas, keratoacanthomas, and malignant nodular melanomas. However, those are papule-nodular lesions that usually extend to the reticular dermis and develop local recurrences and metastases. Conversely, trichilemmal carcinoma is a slow growing lesion and hardly reappears after its excision or develops metastases in other sites1.
Case Study
C.K., 86 years old, female, widow, born in Rio do Sul (SC), coming from Blumenau, former-rural worker.
The patient arrived at the ambulatory of Universidade Regional de Blumenau presenting reddish and slightly painful skin lesion on the left supraclavicular region. Additionally, the lesion showed features of progressive growth, hardened vegetative friable mass, with intermittent local pain and one-year evolution.
For the last 10 years, the patient removed a basal cell carcinoma on the right side of the face and squamous cell carcinomas found on the right pre-auricular region, back of nose and left clavicle. The latter received postsurgical irradiation.
The patient was apparently in good health and did not refer history of systemic pathology.
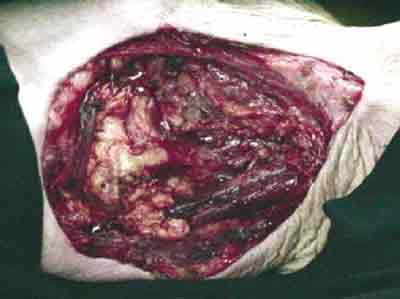
The examination revealed a hardened, reddish, vegetative, ulcerated and painful lesion on the left supraclavicular region, measuring 75x45mm, with bloody secretion and adherence to deep layers. Pre-scalenic muscles were also involved, although not leading to motor deficit (Photos 1-2).
Surgical treatment was established, during which a nodular infiltrating and ulcerated tumor of the neck skin was found. The left clavicular fossa was involved and blocked by neoplasia. The clavicular periosteum and scalenic muscles (Photo 3) were removed, and primary reconstruction with myocutaneous flap rotation of the pediculated greater pectoralis muscle in the inner mammary artery was performed.
The patient responded well to treatment and was discharged from hospital on the 5th postoperative day.
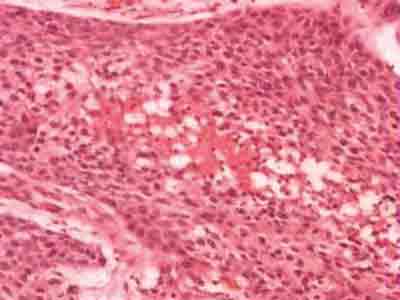
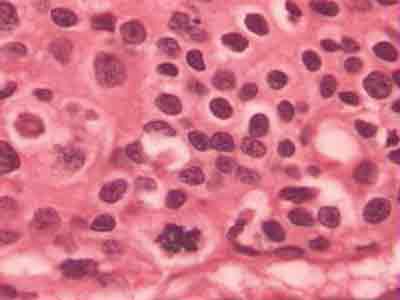
The clinical pathology revealed that macroscopically the specimen consisted of skin segment and subcutaneous tissue measuring 105x70x60mm. A 75x45mm elevated lesion formed by a pale, granular and friable tissue was observed on the epidermis surface. It showed deep infiltration and hypodermis involvement. Microscopically, the histological sections revealed an infiltrating and ulcerated epithelial neoplasia, constituted by cystic configuration and multiple layers of epithelial cells with enlarged hyperchromatic nucleus, presenting moderate pleomorphism and broad eosinophilic cytoplasm. Extensive necrotic fields and numerous mitotic figures were present. Deep infiltration of the skeletal muscular tissue was observed. Surgical margins were free of disease. Diagnosis: Trichilemmal carcinoma (Photos 5, 6 and 7).
Discussion
Trichilemmal carcinoma, also known as trichilemmal pillar tumor, is a rare condition. It shows predilection for females over 40 years of age4. The usual sites include scalp, neck and face, which are sun-exposed areas.
Clinically the tumor may appear as a pale tan or reddish papule, ulcerated or exophytic plaque or nodule, presenting keratosis or scabs3.
In general, it arises as a solitary lesion, measuring 3 cm in its greater diameter1. It is frequently found within less than a year of evolution, presenting fast growth3.
The trichilemmal carcinoma is the malignant form of the trichilemmoma. Although this issue is still under investigation, high-dosage irradiation therapy on previous lesions, as well as repetitive X-rays for diagnostic purposes, have been related to this type of carcinoma3. Moreover, there are reports of development of this lesion from a burn scar5 or in regions frequently exposed to sun6.
Histologically, TLC consists of cells that proliferate to the central lobular region from the pilosebaceous follicle composed by mitotic-potential malignant cells, although of low aggressive nature. Some of these tumors show pagetoid spread, others show infiltration into the deep dermis (intra-epithelial invasion). Lymphocystic and plasmatic cells are usually observed.
Even though its histological structure suggests a certain malignancy grade, trichilemmal carcinoma has an indolent clinical course. Cases with recurrence or metastasis have been seldom reported in the literature7-9.
Trichilemmal carcinomas must be distinguished from other malignant skin lesions so that the best treatment options can be adopted according to the lesion.
Surgery is the treatment of choice for trichilemmal carcinomas with comprehensive excision and periodical follow-up. Adjuvant therapy is not necessary.
Closing Remarks
Trichilemmal carcinoma is a rare skin neoplasia. In a 40-year-old female patient presenting a lesion in a sun-exposed area, characterized by vegetative mass simulating malignancy, this diagnosis should be considered. This is a slow-growing neoplasia, with low mitotic rate, rare occurrence of local relapses or metastases, and whose treatment is mainly surgical.
References
1. Barnhill RL et al. Textbook of Dermatology. United States of America. Mc Graw-Hill Company, Inc.; 1998. p.613-4.
2. Mckee P et al. Pathology of the Skin. 2ª ed. Barcelona, Spain: Mosby-Wolf; 1996. 15.21-15.22.
3. Chan KO et al. Multiple tumor presentation of trichilemmal carcinoma. Br J Plast Surg 1999; 52(8): 665-7.
4. Maciel RARS et al. Tumor pilar triquilemal: estudo crítico de um caso peculiar e revisäo de literatura. An brasdermatol 1985; 60(2):81-6.
5. Ko T et al. Trichilemmal carcinoma developing in a burn scar: a report of two cases. J Dermatol 1996; 23(7): 463-8.
6. Dekio S, Funaki M, Jidoi J, Mihara M. Trichilemmal carcinoma on the thigh: report of a case. J Dermatol 1994; 21(7): 494-6.
7. Reis JP et al. Trichilemmal carcinoma: a review of 8 cases. J Cutan Pathol 1993; 20: 44-9.
8. Boscaino A et al. Trichilemmal carcinoma: a study of seven cases. J Cutan Pathol 1992; 19: 94-9.
9. Swanson PE et al. Trichilemmal carcinoma: clinicopathologic study of 10 cases. J Cutan Pathol 1992; 19: 100-9.
Photo 1. Photo of the lesion. Ectoscopy: lesion located on the left supra-clavicular region, vegetative, ulcerative and with reddish color.
Photo 2. Photo of the lesion before the surgical procedure. Excision margins were limited by methylene blue.
Photo 3. Photo after the excision of the lesion.
Photo 4. Photo after primary reconstruction with flap rotation.
Photo 5. Micropathography - HE 40x - Skin with preserved epidermis, we can see infiltrative epithelial neoplasm in the dermis - trichilemmal carcinoma.
Photo 6. Micropathography - HE 40x - Neoplasm forming solid elongated blocks growing towards dermis, with central necrosis - trichilemmal carcinoma.
Photo 7. Micropathography - HE 40x - Blocks of neoplastic cells with moderate nuclear atypia, keratinized cytoplasm. Observe mitosis figure at 6 o'clock. - trichilemmal carcinoma.