Year: 2004 Vol. 70 Ed. 5 - (18º)
Relato de Caso
Pages: 695 to 700
TEMPORAL BONE FIBROUS DYSPLASIA - REPORT OF TWO CASES
Author(s):
Roberto Claudio B. Oliveira1,
Lidio Granato2,
Gustavo Polacow Korn2,
Manoel de Almeida Marcon3,
Adicelia Pacheco Cunha3
Keywords: fibrous dysplasia, temporal bone, mastoidectomy.
Abstract:
Fibrous dysplasia of the temporal bone (FDTB) is a disorder which etiology is still controversial. Its main clinical feature is a progressive narrowing of the external auditory canal following by conductive hearing loss. Temporal or retroauricular enlargement, ear discharge, otalgia, and sensorineural hearing loss are additional findings. Women and Caucasians are more affected. The prominent finding is a homogeneous radiodense "grounded glass" like image shell surrounded by dense cortical tissue. However, other radiological patterns of this disease may be displayed. Microscopically, a trabecular of bone in "Chinese letter" configuration is found. The two cases of FDTB herein reported are particularly special for a far beyond temporal commitment reaching the zygomatic area in the first case and sphenoid and pterygoid bones in the second one. This infrequent clinical feature with unusual radiological findings made these two cases worth-reported.
![]()
INTRODUCTION
Fibrous dysplasia is a bone disorder of unknown origin in which normal bone is replaced by fibrotic and trabecular disorganized bone tissue. It was first described by McCune and Bruch in 1937. The disease was classified into three variants: monostotic form, polyostotic and Albright syndrome. The disease occasionally affects the temporal bone, with unilateral predominance associated with conductive hearing loss secondary to external auditory canal compression 1.
As to gender, the proportion of patients with temporal fibrous dysplasia is predominant in men (2:1). The main racial group affected is Caucasians, with 80% predominance 2. Typical radiological exam demonstrates characteristic aspect of homogenous ground-glass appearance, involved in a shell of dense cortical tissue.1
The most common manifestation is conductive hearing loss. Other symptoms include temporal and retroauricular bulging, otorrhea, otalgia, pulsatile tinnitus and sensorineural hearing loss.
We will describe two cases of fibrous dysplasia, whose main characteristic was involvement beyond temporal bone affection.
CASE REPORT
Case 1.
C.P.S., 26 years of age, female housewife, born and living in Sao Luiz do Maranhão.
The patient had complaint of right ear mass for 6 months associated with fetid otorrhea and progressive hearing loss on the right for approximately 3 years. In the past year, she had noticed asymmetric growth of the face, larger on the right. As personal history, she was submitted to tympanoplasty six years before on the left ear.
General physical examination did not evidence affections and the ENT exam showed left ear with affections. Facial asymmetry, owing to bulging of retroauricular and zygomatic regions, of hardened consistency without phlogistic signals on the right side. The otoscopy on the right side showed polypoid lesion, bleeding upon touch in the external auditory canal, purulent secretion around the lesion preventing visualization of tympanic membrane. Audiometry showed bilateral conductive hearing loss, mild on the left and moderate/severe on the right, with 96% speech discrimination on both sides.
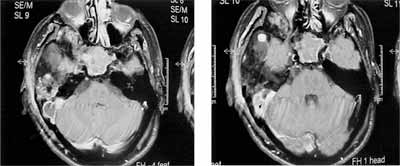
We ordered computed tomography (CT scan) of temporal bones. The findings included: evidence of diffuse increase throughout the right temporal bone, expansive, of heterogeneous density, similar to ground-glass; absence of ossicle chain and reduction of middle ear volume; presence of soft tissue material occupying the external auditory canal, as demonstrated in Figures 1 and 2.
Figures 1 and 2. Diffuse increase of temporal bone, with heterogeneous density, similar to ground glass.
We decided for conduction of radical mastoidectomy with wide meatoplasty. We removed external auditory canal polyp and observed material of whitish aspect, with desquamation up to inside the middle ear, similar to a cholesteatoma. The mastoid was filled with fibrous-bone tissue similar to spongy bone, occupying also the aditus and antrum; tympanic cavity of reduced volume; absence of incus and malleus, and remains of stapes.
The clinical pathology result demonstrated temporal bone fibrous dysplasia on the right.
Case 2.
U.C.A., 36 years old, male business person, born and living in Santa Cruz, SP.
The patient had had diagnosis of fibrous dysplasia on the right for 10 years followed periodically by clinical examination and CT scan, progressing with significant hearing loss on the right and intermittent otorrhea. Fifteen days before he had presented fever, severe right ear pain, otorrhea and bulging of retroauricular and temporal regions with hyperemia and pain upon palpation.
The general physical examination was uneventful and ENT examination showed stenosis of external auditory canal on the right, with small amount of yellowish secretion, and it was not possible to visualize the tympanic membrane. We confirmed the presence of hyperemia and retroauricular edema on the right and homolateral temporal region with a small drainage orifice on the external third of auditory canal. As to tuning fork test (512Hz), left air conduction values were better than on the right, Rinne was positive on the left and negative on the right, Weber lateralized to the right. Assessment of cranial nerves and neurological examination did not evidence significant deficits. Audiometry showed mixed hearing loss on the right, as shown by Figure 3.
Figure 3. Audiometry showing mixed hearing loss on the right.
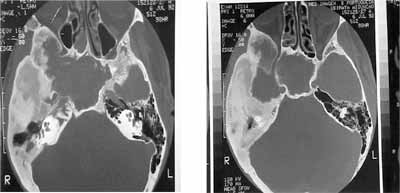
We ordered magnetic resonance imaging (MRI). The findings included: significant bone thickness comprising the temporal bone (squamous portion and petrous part) and homolateral pterygoid, which presented predominance of hyposignal in sequences T1 and T2; we observed material with hypersignal in T2, occupying sphenoid sinus and mastoid on the right, with loss of habitual trabecular bone, and peripheral enhancement after injection of paramagnetic contrast. We could see bulging of sphenoid sinus wall, increase of soft parts of right peri-auricular region with impairment of subcutaneous fat, as demonstrated by Figures 4 and 5.
Figures 4 and 5. T1 spin after contrast and T1 with suppression of fat. We can notice increase in soft parts with impregnation of anomalous contrast and enhanced area.
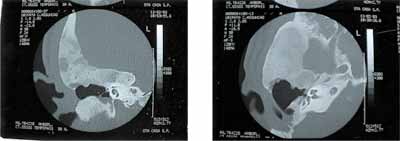
We also conducted temporal bone CT scan. We could notice thickness that impaired the petrous pyramid on the right, with area of sclerosis with unpolished glass aspect, characteristic of fibrous dysplasia. We observed material with soft part attenuation in the tympanic membrane, and we did not visualize the ossicle chain (suggesting the presence of cholesteatoma). Presence of stenosis of external auditory canal. We did not observe fistula pathway (Figures 6 and 7).
Figures 6 and 7. Areas similar to unpolished glass, associated with external auditory canal stenosis and probably, cholesteatoma.
We decided for the conduction of radical mastoidectomy with wide meatoplasty. In the external auditory canal, we noticed presence of polyp in its external third, with fistula on the superior-external region with purulent secretion drainage. The remaining of the external canal had stenosis caused by bone growth. In the mastoid opening, we observed friable subcutaneous tissue with granulation, presence of fistula in the posterior mastoid wall visualizing large cavity with tissue similar to cholesteatoma. Mastoid antrum was reduced because of the dysplastic process filled with bone tissue, hindering the access to middle ear, which presented only malleus with erosion, incus was absent and there were remains of stapes. We removed bone tissue similar to spongy bone with exposure of temporomandibular joint for cleaning purposes and removal of cholesteatoma. Exposure of posterior-inferior meninges; facial nerve was apparently intact. The clinical pathology analysis revealed presence of dysplastic bone and cholesteatoma.
The patient came back after one year and the postoperative follow-up showed radical cavity with good aspect and totally epithelialized. In the inferior portion that corresponded to the region of hypotympanum there was soft part tissue recovered with skin.
Figures 8 and 9. One-year postoperative follow-up showing good aspect of wide radical cavity, surrounded by dysplastic bone.
DISCUSSION
Von Recklinghausen in 1891 was the first one to describe the characteristic bone lesions which are today named fibrous dysplasia, but only in 1937 McCune and Bruch 3 described this distinct clinical entity from other bone formation anomalies. The term "fibrous dysplasia" was introduced by Lichtenstein 4 in 1938, and it was classified into three subgroups. The monostotic form with involvement of one single bone (70%), the polyostotic form, with involvement of many bones (30%), and McCune-Albright syndrome with bone impairment associated with skin and mucosa damage and endocrinopathies. In all clinical forms, bone lesions lead to trabecular and cortical bone defects that may range from some centimeters to massive lesions that distort the contour of the affected bone 5.
Etiology of fibrous dysplasia (FD) is controversial. It is believed that there may be abnormal enzymatic activity in the formation of mesenchymal bone 6, abnormal calcium and phosphorous mechanisms 7, and osteoblastic hyperplasia 8. Schlumberger suggested that the monostotic form of the disorder may not be related to both Albright syndrome and polyostotic form, but it is rather caused by an abnormal process of healing right after a lesion.9
Radiological studies of such lesions normally demonstrate homogenous radiodensity involving any combination of temporal bone and petrous, tympanic, mastoid or squamous portion. Three radiographic patterns of skull and facial bone fibrous dysplasia were described by Fries: Pagetoid (56%), affecting radiodense and transparent areas; sclerotic (23%), homogeneously dense, and cystic pattern (21%), with radiolucid spherical or ovoid areas surrounded by dense limits10.
Monostotic fibrous dysplasia represents 7% of all bone tumors and it is the most frequent benign lesion to affect the brain. It is normally detected in the first 2 decades of life, even though it involves only 10% of craniofacial structures; it is the most prevalent fibrous dysplasia of the head and neck 2. Maxilla and mandible are the most frequently affected bones in the cranio-maxillo-facial area. Temporal bone is affected in only 18% of the FD cases, and it is frequently associated with monostotic forms rather than polyostotic ones 11.
As to pathophysiology, whereas most authors think that monostotic fibrous dysplasia represents a congenital anomaly of mesenchymatous bone formation, transmission mode (autosomal dominant or recessive) is still an open topic 6. Other theories of MFD are less important. Schlumberger described FD as a disorder of healing process 12. Other authors suggested that MFD was secondary to a stop in bone maturation.
Macroscopic examination of FD reveals expansion of trabecular bone inside a thin cortical layer, medullar and trabecular region form an area that becomes soften, either white or red, depending on vascularization of the lesion 6. However, since there is no definite capsule, there is abrupt transition to healthy bone. Bone sutures are respected so that FD does not extend to articulated surfaces of neighboring bones. There is no periostactic invasion 6, 12.
Microscopic assessment shows stroma of collagen matrix with fibroblasts in an entangled pattern with trabecular bone, similar to Chinese letters. FD shows bone pattern that is entangled rather than lamellar, which allows differentiation from ossifying fibroma 9, 13.
MFD is a benign process of slow growth, which becomes silent at puberty. The most common otological symptom of temporal bone FD is conductive hearing loss secondary to occlusion of Eustachian tube, external auditory canal obstruction or fixation of ossicle chain 14. Exuberant growth of fibrous dysplasia in the region of the external acoustic canal leads to progressive stenosis, resulting in sequestration of keratin fragments 15. Complete erosion of ossicles may be seen secondary to cholesteatoma 16. Since the petrous apex is occupied by the cholesteatoma there may be erosion of temporal bone at any of the four directions: superiorly to the middle cranial fossa, posteriorly to the posterior cranial fossa, inferiorly to the neck, and inferior-medially to the parapharyngeal space. As the disease aggressively progresses in the temporal bone, there may also be involvement of cranial nerves or central nervous system 13. Facial nerve may be involved in 10% of the cases 1.
Differential diagnosis of FD includes malignant and benign lesions. Benign lesions are: solitary unilocular cyst, non-ossifying fibroma, eosinophylic granuloma, cholesteatoma, meningioma, Paget disease, osteochondroma, ossifying fibroma, repairing granuloma of giant cells, exostosis, aneurysmatic bone cyst, cystic fibrous osteitis, ameloblastoma, and plasma cell myeloma. Malignant lesions include sarcoma and metastatic osteoblastic lesions.
Treatment of temporal bone fibrous dysplasia has been traditionally conservative and directed to preventing stenosis of external auditory canal. The course of fibrous dysplasia is unpredictable. Some lesions remain stable for many years, whereas others can quickly progress. Despite that, fibrous dysplasia normally presents slow, progressive and chronic growth. Spontaneous neoplastic transformation in sarcoma has been described in 0.04% of the cases 17. Radiotherapy is contraindicated in the control of fibrous dysplasia because it can increase the incidence of malignant degeneration 15, 18. Out of sarcomas, osteosarcoma is the most frequently found variety, followed by chondrosarcoma 17,19.
In both cases described here, there was formation of polyp and stenosis of external auditory canal. In our study, the second case had involvement not only of the temporal bone but also of sphenoid and pterygoid region on the right, in addition to velamentum of sphenoid sinus, compatible with mucocele, representing much more significant involvement than in the first case. In addition, owing to the obstruction, there was secondary infection with drainage deficiency, leading to formation of abscess and fistula.
In the first case, infectious process that started after bone expansion led to keratin sequestration, progressing to cholesteatoma, destruction of ossicle chain with functional disorder and formation of large polyp obstructing the external auditory canal. The CT aspect suggested FD, but in other areas there was higher density and the clinical pathology suggested osteoma. In a literature report, Kessler et al, 1990, described a case of temporal bone dysplasia that was initially diagnosed as osteoma20.
CLOSING REMARKS
Temporal bone fibrous dysplasia may have different presentations and the disease may be limited to the temporal bone or affect other neighboring regions. Diagnosis is not always easy; in many cases it may be mistaken by other entities, such as osteoma. Thus, for correct diagnosis, it is necessary to rely on clinical history, complete ENT examination, imaging studies and clinical pathology analyses.
REFERENCES
1. Morrissey, D.A., Talbot J. M., Scheuning I.I. A J Fibrous dysplasia of the temporal bone: reversal of sensorial hearing loss after the decompression of the internal auditory canal. Laryngoscope, 1997; 107: 1336- 1340.
2. Nager, G.T., Kennedy, D.W., Kopstein, E. Fibrous dysplasia: a review of the disease and its manifestation in the temporal bone. Ann Otol Rhinol Laryngol, 1982; 91(supple 92):1-52.
3. McCune, D. J., Bruch, H. Osteodystrophia fibrosa: Report of a case in which condition was combined with precocious puberty, pathologic pigmentation of skin and hyperthyroidism with review of literature. Am J Dis Child 1937; 54:806-848
4. Lichtenstein, L. Polyostotic fibrous dysplasia. Arch Sur 1938; 36: 874-898.
5. Reitzik M, Lownie JF: Familial polyostotic fibrous dysplasia. J Oral Surg 1975; 40: 769-774
6. Lichtenstein L, Jaffe HL: Fibrous dysplasia of bone. Arch Pathol 1942; 33: 777-816
7. Murray RC, Kirkpatrick HJR, Forrai E: Case of Albright`s syndrome (osteitis fibrosa disseminata ) . Br J Surg 1946; 34: 48-57.
8. Changus GW: Osteoblastic hyperplasia of bone . A histochemical appraisal of fibrous dysplasia of bone. Cancer 1957; 10: 1157-1161 .
9. Schlumberger HG: fibrous dysplasia of single bones (monostotic fibrous dysplasia ) . Milit Surgeon 1947; 99:504-527 .
10. Fries JW: The roengten features of fibrous dysplasia of the skull and facial bones: a critical analysis of thirty-nine pathologically proven cases. Am J Roentgenol 1957; 77:71-88 .
11. Younis, M., Haleem, A. Monostotic fibrous dysplasia of the temporal bone. J Laryngol Otol , 1987; 101, 1070-1074.
12. Batsakis, J. Tumours of the head and neck. 2nd edition. Willian and Wilkins, Baltmore, 1979; 410-413.
13. Zappia, J. LaRouere, M., Telian, S. Massive ossifying fibroma of the temporal bone. Otolaryngol Head Neck Surg , 1990; 103(3):480-483.
14. Lambert, P.,Brackman, D. Fibrous dysplasia of the temporal bone: the use of computerized tomography. Otolaryngol head neck surg 1984;92(4): 461-462.
15. Smoutha, E., Edelstein, D., Parisier, S. Fibrous dysplasia involving the temporal bone: report of three new cases. Am J Otol 1987; 8(2): 103-107 .
16. Basek, M. Fibrous dysplasia of the middle ear. Arch Otolaryngol 1967; 86: 528-534.
17. Schwartz DT , Alpert M: The malignant transformation of fibrous dysplasia. Am J Med Sci 1964; 247:35-54.
18. Gross CW, Montgomery WW: Fibrous dysplasia and malignant degeneration. Arch Otolaryngol 1967; 85:653-657
19. Huvos, A., Higinbothan, H., Miller, T. Bone sarcomas arising in fibrous dysplasia. J Bone Joint Surg 1972; 54A: 1047-1056.
20. Kessler A., Wolf M., Ben-Shoshan J. Fibrous dysplasia of the temporal bone presenting as an osteoma of the external auditory canal. Ear Nose Throat J, 1990;69:197-199.