Year: 2004 Vol. 70 Ed. 5 - (14º)
Artigo de Revisão
Pages: 671 to 677
AIRWAY COMPLICATIONS ASSOCIATED WITH ENDOTRACHEAL INTUBATION
Author(s):
Regina H. G. Martins1
Norimar H. Dias2,
José R. C. Braz3,
Emanuel C. Castilho4
Keywords: intubation, airway, complications, morbidity.
Abstract:
We reviewed the main airway complications associated with endotracheal intubation, presented some results of our researches and alert health professionals for the high incidence of airway injuries. The knowledge of the physiopathology of these injuries will help to proper prophylactic and practice conducts to prevent the airway complications associated with endotracheal intubation.
![]()
INTRODUCTION
Endotracheal intubation allows healthcare professionals to provide either short or a long time ventilation support for patients under anesthetics or under mechanical ventilation. The presence of oral or nasotracheal tubes in direct contact with the airway structures may cause lesions in the mucosa, especially in traumatic intubation or in prolonged use of large diameter tubes and also due to high pressure in tube cuffs. One can also note damage to air conditioning in the nasal fossa, as it is not in contact with the inhaled air - due to the presence of the tube - it can not perform the important role as filter, moisturizer and heater of inhaled gases.
In the last decades, attempts to reduce morbidity associated with intubation became evident with the development of new types of cuffs for tracheal tubes (which also became longer and with better compliance), with the availability of new tube prototypes and with heated moisturizers coupled to the mechanic ventilation. Likewise, guidelines to residents, physicians and nurses regarding the necessary care while introducing the tracheal tube have been emphasized as well as information about the proper diameter to be used and the proper techniques for suctioning pulmonary excretions.
Based on the knowledge developed on airway complications and the pathophysiology of the mucosa injuries associated with endotracheal intubation, simple and practical prophylactic actions should be taken during the care provided to patients undergoing intubation or tracheotomy to assure reduction in airway morbidity rates.
REVIEW OF LITERATURE
From the 1960's on, several publications have focused on the different mucosa injuries in the upper airway tract due to endotracheal intubation - either because they were difficult intubations, traumatic intubations, and long duration intubations or because of the compression of the mucosa caused by the tube cuff1-4. For pedagogical purposes, the different injuries shall be divided into three categories: lesions happening during the introduction of the intubation tube; secondary lesions caused by the contact of the tube or its cuff with the airway structures, and, injuries caused by poor conditioning of the inhaled air.
Injuries during the introduction of the intubation tube
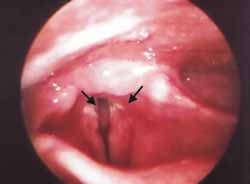
When the tube is being orally introduced, during the attempts to expose the glottis with the laryngoscope, we read about lacerations occurring in the lips, gingival region, uvula, palate, tonsils, pharynx, epiglottis, vocal folds, esophagus and trachea and, also, about hematomas and avulsion in the vocal folds, dislocation and luxation in the arytenoid cartilages 5. These acute injuries happen, usually, when inexperienced personnel perform the task, and, in emergency situations that require a fast approach to the airways (Figure 1).
Depending on its extension, the lacerations in the oral mucosa and the pharynx may lead to severe dysphagia. Lesions in the cartilage structures, such as the epiglottis, the arytenoids and the cricoids may develop into perichondritis and fever, otalgia, dysphagia and even lack of mobility of glottic structures as a result of cricoarytenoid joint chondritis 6.
Perforations in the esophagus may cause mediastinitis and abscess7. Lacerations in the tracheal mucosa occur mainly in the membranous portion and may cause pneumomediastinum 8. Teeth fractures and avulsions, particularly in the upper incisors may also occur due to traumatic bearing of the laryngoscope blade during the attempts to expose the glottis, especially in larynges that have too anterior neck position.
In nasotracheal intubations, there is the possibility of occurring lacerations in the nasal vestibular mucosa, in the turbinates and rhinopharynx causing epistaxis that may occasionally be quite severe. There are also published reports describing ischemic lesions in the skin and in the nasal vestibular cartilage due to improper fixation of the tube 5.
Secondary injuries caused by the contact of the tube or its cuff with the airway structures
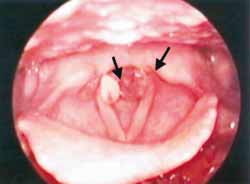
Clinical trials have displayed several types of larynx and tracheal mucosa lesions after varied periods of intubation. Duration of intubation is one of the main reasons for aggravating the injuries9,10. As the glottis has a "V" configuration, the main lesions occur in the posterior portion of the larynx, at the level of the vocal apparatus where the tube is in close contact with the mucosa. Endoscope examinations performed soon after extubation allow the identification of superficial ulcerations in this site that usually has fast tissue healing (Figure 2). However, some patients develop granulomas - usually bilateral and pediculated - in the inner face of both vocal apophasis. These granulomas lead to persistent dysphonia and not always have spontaneous regression: sometimes they require surgical removal (Figure 3)11.
The continuous and traumatic contact of the tube in the posterior glottis area may cause ulceration in that site involving the interarytenoid mucosa epithelium, scar with cicatricial fibrosis and fixation of the arytenoid cartilage in the midline, simulating bilateral palsy of the vocal folds. In these cases, direct laryngoscopy and electromyography of the vocal muscle are necessary to clarify the diagnosis6.
Inappropriate intubation tube diameter and difficulty in keeping the intubated patient immobile are factors that predispose to the development of airway lesions. Constant flexion, extension and lateral neck movements made by an agitated patient cause friction of the tube and the cuff against the respiratory tract. In a patient who is not sedated, there are also reflex movements of swallowing and adduction of the vocal folds on the tracheal tube. Thus, the longer the tube remains, the higher the risks for the occurrence of lesions.
Ulcerate injuries involving the glottic region may happen during self-extubation made by the patient when the cuff is inflated.
The tracheal mucosa, in contact with the tube cuff, is particularly vulnerable to ischemic lesions. The older tube cuffs bear low air volume, high pressure and are not compliant. They were gradually replaced by more compliant and more extensive tubes. As they are longer, they distribute the pressure in a more extensive area, therefore, decreasing the possibility of injuring the tracheal mucosa.
Several authors have studied the mucous membrane injuries related to high pressure of endotracheal tube cuffs. Nordin (1977)1 carried out a thorough trial on intubated rats by varying the cuff pressure from 20 to 100mmHg. He noticed that, when the pressure was higher than the capillary perfusion (25 mmHg), an ischemic process would occur in the mucosa and this ischemia was proportionally as strong as the increase in pressure. The author observed extensive erosion in the respiratory epithelium when pressures above 100 mmHg were used and erosion expanded to the intercartilaginous areas. These areas would also become grounds for bacteria colonies and chondritis.
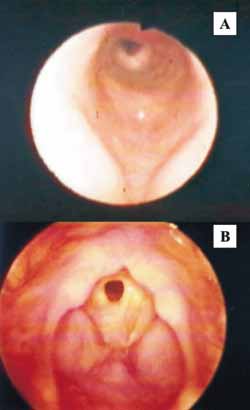
In patients who need long periods of endotracheal intubation, such as in cases of chronic respiratory failure and in neurological patients, the lack of control in the interior pressure of the cuff may cause a permanent mucosa ischemia, tracheal dilation and healing with stenosis. (Figures 4a and 4b)12. The development of these lesions is directly related to the duration of intubation. According to Whited (1979)13, the risks of stenosis are minimum in less than six-day intubations (< 2% of the cases) and become more meaningful after more than ten-day intubations (12% to 15% of the cases).
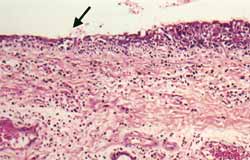
In an experimental study with anaesthetized dogs undergoing endotracheal intubation for only four hours, we were able to show - by means of a histological analysis of the tracheal epithelium in the area in contact with the intubation tube - early lesions in the tracheal mucosa, such as superficial erosions and infiltrate of neutrophil polymorphonuclear cells (Figure 5)14. Similar findings had been documented by Alvarez and Aragón (1981)15 while analyzing trachea fragments of patients submitted to tracheotomy and who had been kept intubated for at least 48 hours. In the mucosa erosion site, the authors have identified fibrin deposits and the beginning of a recovery process.
It is known that some patients develop tracheal stenosis even if intubated for short periods. Thus, one must recognize that other factors play a role in the development of tracheal stenosis, such as respiratory tract infections, use of systemic corticoids, hemodynamic instability, hypoproteinemia, hypoxemia, anemia and the immotile cilia syndromes. 16.
Measuring cuff pressure is not a routine in the operating room or in the ICU (intensive care unit). Estimating cuff pressure by palpating the trial cuff does not detect high pressures. The importance of monitoring the pressure occurring inside the cuff is highlighted by some authors because it is a very simple and low cost procedure that may be done with a portable digital manometer. 4,17,18.
There is no consensus yet on the maximum pressure in the tracheal tube cuff to avoid lesions. The critical values for cuff pressure have been considered between 25 to 30 cmH2O, very close to the capillary perfusion pressure 3,4.
In our series, Castilho et al. (2003)4, in a recent experimental study with dogs, analyzed the histology of the tracheal mucosa from the site in contact with the cuff, using in one of the groups cuff pressure of 25 cmH2O, and, in another group, sealing pressure of 13 cmH2O (the minimum pressure that enabled artificial ventilation). The authors observed that, in both groups, there were important epithelium lesions when compared to the normal respiratory epithelium: there were areas with superficial erosion and cilia loss (Figures 6a and 6b). The study confirmed the importance of maintaining cuff pressure below the capillary perfusion pressure since the authors detected some lesions, although superficial, in the respiratory epithelium even with very low levels of pressure inside the cuff.
The pressure inside the tube cuff may increase during anesthesia, because of diffusion of anesthetic gases occurring inside it, as it happens with nitrous oxide soon after the beginning of the use of anesthetics. In order to avoid cuff expansion, an intubation tube with an attached air escape valve (Lanz valve) has been designed (Figure 7). In this type of probe, the tracheal tube has a re-diffusion valve that allows for the interior pressure in the cuff not to exceed 25 to 30 cmH2O. Aiming at studying the efficacy of this new tube cuff prototype, Navarro et al. (2001)18 measured intubation tube cuff pressures in 40 patients receiving anesthetics with nitrous oxide - 20 of them submitted to intubation under conventional tube with low pressure cuffs and 20 of them intubated with tubes with Lanz valve. Although there is evidence of the efficacy of the tubes with Lanz valve, the cost of this tube is still too high, reason why its routine use in hospitals is unfeasible.
One other attempt to avoid the diffusion of nitrous oxide into the cuff is the introduction of lidocaine solution or sterile saline in its interior. Clinical trials have shown the efficacy of this method, which also reduces the occurrence of odynophagia and dysphagia symptoms postoperatively, causing milder reaction to the tracheal tube when lidocaine is used19. The main inconvenience in this method is the risk of accidental rupture of the tube cuff leading to aspiration of large amount of liquid into the airways. Another attempt to minimize the morbidity rate associated with endotracheal intubation is the use of laryngeal mask (Figure 8), which started to be used, initially, in salvage situations as it is very easy to use even by inexperienced personnel. As the years went by, the advantages proved to be better than expected and these masks started to be used as routine in hospitals. Its main advantage is that, after it is inserted, it fits in the hypopharynx and does not get in contact with the glottis; therefore, it reduces postoperative hoarseness and dysphagia 20. This is the reason why voice professionals started to use the laryngeal mask as their first choice procedure in anaesthesia21.
Moreover, note that the hypopharynx region - where the cuff remains inflated after its insertion - is quite extensible and well adapted to the swallowing functions, receiving different volume of food bolus. Thus, as the pressure inside the cuff is not totally transmitted to the mucosa, the incidence of mucosa ischemia and stenosis is much lower.22.
In a trial with dogs undergoing anesthesia, we have used the laryngeal mask with different pressures in the cuff interior (group I 119 mmHg + 4; group II - 234 mmHg + 13) and analyzed the histology and scan electronic microscopy of the hypopharynx region in contact with the tube cuff. We noticed, in both groups, mild congestion of the cover epithelium, acute inflammatory process and small areas of mucosa superficial ulceration, even in the group submitted to high pressure in the cuff (Figures 9a and 9b)23. Although we have not observed significant changes in laryngopharynx mucosa in contact with the laryngeal mask, several authors report complications with the use of this mask such as edema; cyanosis and tongue paralysis24 ; vocal fold paralysis25; and uvula and palate lacerations26.
Lesions caused by poor conditioning of inhaled air
Most of the conditioning of inhaled air occurs in the nasal fossa and in the rhinopharynx. That is where the air is heated and humidified and where a large amount of particles and microorganisms of the environment are filtered and adhere to the mucus layer covering all the respiratory epithelium. Thanks to the mucociliary activity, these particles are propelled towards the digestive tract to be swallowed and eliminated. In an intubated or tracheomitized patient, the inhaled air goes straight to the trachea without any previous conditioning. Among the main consequences for inhaling dry and cold air are the damages caused to the epithelium such as edema in the airway mucosa, cilia dyskinesia and secretion stasis27.
Marfatia et al. (1975)28 analyzed the respiratory epithelium of rats exposed to mechanical ventilation with dry and cold air and observed the destruction of the hair cells, areas of disorganized respiratory epithelium and mucus thickening. They have also underlined the increase in airway resistance, decrease in pulmonary compliance, changes in pulmonary inflammatory interstitial surfactant and infiltrate composition. Having as a goal the analysis of the effects of temperature and humidity of the inhaled air in the respiratory epithelium, we have carried out trials in dogs submitted to mechanical ventilation and air inhalation at different temperatures (27 to 36o C) and different absolute humidity grades (17 to 36 mgH2OL-1) during a four-hour period29. In the histological analysis of tracheobronchial tree mucosa biopsies, we observed infiltrate of polymorphonuclear cells on the epithelial surface and in the corium in the group of animals ventilated with cold and low humidity gases, and, also, congestion and hemorrhage. The respiratory epithelium was normal in the group that received ventilation with gases heated at temperatures between 32 and 36o C and humidity ranging from 30 to 36 mgH2OL-1.
Even after several publications have proven that poor conditioning of inhaled air into the respiratory tract is a factor of morbidity, it is still not a routine in operating rooms, even during long surgeries, to have heated humidifiers attached to the ventilation systems. In most of our services, these devices are only available in the intensive care units.
Heat and humidity switchers, called "artificial nostrils", are small devices coupled to the ventilation systems. They are filters that are able to retain heat and humidity, which are eliminated during exhaling and re-used in inhaling. In trials with dogs, Bisinotto et al. (1999)30, by means of histological studies and by scan electronic microscopy of tracheobronchial tree spears, have shown the capacity of these switchers in conditioning the inhaling air and their ability to help to preserve the integrity of the respiratory epithelium. In the group of animals where the devices were not used the authors reported low heat and humidity values in the inhaling branch of the ventilation system and histological lesions in the respiratory epithelium, such as cilia loss and cilia agglomeration in addition to dryness and rupture of mucus droplets.
DISCUSSION
Secondary airway complications associated with endotracheal intubation are quite frequent and many of them have mild symptoms that do not last long. Nevertheless, in many cases these lesions may be severe and affect permanently larynx and trachea structures and they require surgical repair, such as with glottic and tracheal stenosis.
Breathing through a tracheal tube is not a physiological act but, in some cases, it becomes necessary. Knowing the airway morbidity associated with intubation and understanding lesion pathophysiology and the predisposing factors for these injuries enable us to adopt prophylactic procedures that surely will help us to reduce these complications.
Clinical research studies and trials mentioned in this article enabled the adoption of guidelines for intubated patients such as: carefulness and dexterity in placing the tube; ideal diameter choice; option for new tube prototypes with more compliant and more flexible cuffs; proper immobilization of the patients; careful tracheal suctioning; permanent monitoring of the pressure inside the cuff, and use of heated humidifiers or heat and humidity switchers.
CLOSING REMARKS
Airway complications associated with endotracheal intubation are frequent and, many times, quite severe. The incidence of these lesions can be minimized when we understand its pathophysiology, which allows us to adopt prophylactic procedures that should be taught and spread among all healthcare professionals who care for intubated patients.
REFERENCES
Nordin U. The trachea and cuff-induced tracheal injury. Acta Otolaryngol 1977; 345(suppl):1-71.
Stauffer J, Olsen D, Petty HT. Complications and consequences of endotracheal intubation and tracheostomy. Am J Med 1981; 70:65-76.
Guyton DC, Barlow MR, Besselievre TR. Influence of airway pressure on minimum occlusive endotracheal tube cuff pressure. Crit Care Med 1997; 25:91-4.
Castilho EC, Braz JRC, Martins RHG, Gregório E. Efeito da pressão limite de 25 mmH2O e mínima de selo do balonete de tubos traqueais sobre a mucosa traqueal do cão. Rev Bras Anestesiologia 2003; 53:743-55.
Lacau Saint Guily J, Boisson-Bertrand D, Monnier P. Lésions liées à l'intubation oro- et nasotrachéale et aux techniques alternatives: lèvres, cavités buccale et nasales, pharynx, larynx, trachée, oesophage. Annales Françaises d'Anesthésie et de Réanimation 2003; 22:81-96.
Gacek RR, Gacek MR, Montgomery WW. Evidence for laryngeal paralysis in cricoarytenoid joint arthritis. Laryngoscope 1999; 109:279-83.
Ku PKM, Tong MCF, Ho KM, Kwan A, Van Hasselt CA. Traumatic esophageal perforation resulting from endotracheal intubation. Anesth Analg 1998; 87:730-1.
Molins L, Buitrago LJ, Vidal G. Tracheal lacerations after intubation. Chest 1998; 114:1793-4.
John SJ, Matsura H, Kotani Y, et al.. Change in tracheal blood flow during endotracheal intubation. Acta Anaesthesiol Scand 1987; 31:300-4.
Brichet A, Ramon P, Marquette CH. Sténoses et complications trachéales postintubation. Réanimation 2002; 11:1-10.
Pontes PAL, De Biase NG, Gadelha MEC. Clinical evolution of laryngeal granulomas: treatment and prognosis. Laryngoscope 1999; 109:289-94.
Luna CM, Legarreta G, Esteva H, Laffaire E, Jolly EC. Effect of tracheal dilatation and rupture on mechanical ventilation using a low-pressure cuff tube. Chest 1993; 104:639-40.
Whited RE. Laryngeal dysfunction following prolonged intubation. Ann Otol Rhinol Laryngol 1979; 88:474-8.
Martins RHG, Braz JRC, Bretan O, Defaveri J. Lesões precoces da intubação endotraqueal. Rev Bras Otorrinolaringologia 1995; 44:181-85.
Alvarez AC, Aragón JA. Alteraciones precoces de la mucosa traqueal, producidas por la intubación observadas mediante el microscopio electrónico de barrido (M.E.B.). An. Otorrinolaringol Ibero-Am 1981; 5:369-80.
Yang KL. Tracheal stenosis after a brief intubation. Anesth Analg 1995; 80:625-7.
Braz JRC, Navarro LHC, Takata IH, Nascimento P. Endotraqueal tube cuff pressure need for precise measurement. Med J 1999; 117:243-47.
Navarro LHC, Braz JRC, Pletsh AK, Amorim RB, Módolo NSP. Estudos comparativos das pressões de balonetes de tubos traqueais, contendo ou não válvula geradora de pressão de Lanz. Rev Bras Anestesiologia 2001; 51:17-27.
Estebe J-P, Dollo G, Corre PL, et al. Alkalinization of intracuff lidocaine improves endotracheal tube-induced emergence phenomena. Anesth Analg 2002; 94:227-30.
Brimacombe J, Berry A. The laryngeal mask airway - the first ten years. Anaesth Intensive Care 1993; 21:225-6.
Zimmert M, Zwirner P, Kruse E, Braun U. Effects on vocal function and incidence of laryngeal disorders when using a laryngeal mask airway in comparison with an endotracheal tube. Eur J Anaesthesiol 1999; 16:511-5.
Marjot R. Pressure exerted by the laryngeal mask airway cuff upon the pharyngeal mucosa. Br J Anaesth 1993; 70:25-9.
Martins RHG, Braz JRC, Abud TMV. Effect of high laryngeal mask airway intracuff pressure on the laryngopharyngeal mucosa. Laryngoscope 2000; 110:645-50.
Laxton CH. Lingual nerve paralysis following the use of the laryngeal mask airway. Anaesthesia 1996; 51:869-70.
Fawcett WJ, Daya H, Weir N. Recurrent laryngeal nerve palsy and the laryngeal mask airway (letter). Anaesthesia 1996; 51:708.
Lee JJ. Laryngeal mask and trauma to uvula. Anaesthesia 1989; 44:1014-5.
Chalon J, Loew DAY, Malebranche J. Effects of dry anesthetic gases on tracheobronchial ciliated epithelium. Anesthesiology 1972; 37:338-43.
Marfatia S, Donahoe PK, Hendren WH. Effect of dry and humidified gases on the respiratory epithelium in rabbits. J Pediatr Surg 1975; 10:560-83.
Martins RHG, Braz JRC, Defaveri J. Estudo da umidificação e do aquecimento dos gases inspirados durante ventilação mecânica no cão. Rev Bras Otorrinolaringologia 1996; 62:206-18.
Bisinotto FMB, Braz JRC, Martins RHG, Gregório EA, Abud TMV. Tracheobronchial consequences of the use of heat and moisture exchanges in dogs. Can J Anesth 1999; 46:897-903.
Figure 1. Laceration and hematoma in the left vocal fold during direct laryngoscopy. Exam performed with rigid telescope.
Figure 2. Ulcerated lesion in the posterior glottic commissure soon after extubation. Exam performed with rigid telescope.
Figure 3. Bilateral intubation granulomas inserted in the vocal apophasis. Exam performed with rigid telescope.
Figure 4. a - Tracheal stenosis (exam performed with flexible nasofibroscope); b - glottic stenosis (exam performed with rigid telescope).
Figure 5. Histological section of dog's tracheal epithelium showing the superficial ulceration in the endotracheal tube cuff site. (20X, hematoxylin-eosine-HE).
Figure 6. a - Normal tracheal epithelial surface in a dog. Note the homogeneous distribution of the cilia tapetum (Electronic Scan Microscopy, 750X); b - Areas of the tracheal epithelium with cilia loss. The remaining cilia are disorderly grouped (Electronic Scan Microscopy, 1500X).
Figure 7. Tracheal tube attached to Lanz valve (arrow).
Figure 8. Laryngeal Mask.
Figure 9. Scan electron microscopy of stratified paved epithelium in the hypopharynx region in contact with the laryngeal mask cuff. Note the areas of superficial epithelial desquamation.
In a, 1260 X; in b, 1570 X.
1. Ph.D., Assistant Professor, Discipline Otorhinolaryngology, Medical School, Botucatu (UNESP).
2. Former resident, Discipline og Otorhinolaryngology, Master in Surgery, School of Medicine, Botucatu (UNESP).
3. Faculty Professor, Department of Anesthesiology, Medical School, Botucatu (UNESP).
4. Ph.D. in Surgery, Physician, Discipline of Otorhinolaryngology, Medical School, Botucatu (UNESP).
This study was carried out by the Discipline of Otorhinolaryngology and the Department of Anesthesiology, School of Medicine, Botucatu (UNESP).
Address correspondence to: Regina Helena Garcia Martins, Disciplina de Otorrinolaringologia, Departamento de Oftalmologia, Otorrinolaringologia e Cirurgia de Cabeça e Pescoço da Faculdade de Medicina de Botucatu, Distrito de Rubião Junior.
18618-970 Botucatu, SP, Brazil
Tel/Fax: (55 14) 38116256 - Email: rmartins@fmb.unesp.br.