Year: 2004 Vol. 70 Ed. 5 - (11º)
Artigo Original
Pages: 651 to 657
Anatomical relationship between the optic nerve and the sphenoid sinus: a computed tomography study.
Author(s):
Paulo Cesar J. Dias1,
Pedro Luiz M. Albernaz2,
Hélio K. Yamashida3
Keywords: optic nerve, sphenoidal sinus, computed tomography.
Abstract:
Introduction: The sphenoid sinus, out of the facial sinuses, is certainly the most neglected as far as diagnosis is concerned. The surgical approach requires a detailed anatomical knowledge, considering the serious complications resulting from injuries of vital structures adjacent to this region. The objective of our research is to evaluate the anatomic relationship of the optic nerve with the sphenoid sinus making use of the computed tomography. Material and Method: The authors present a retrospective analysis of 203 computed tomographies of facial sinus belonging to individuals of both sexes aged 14 and over. The examinations were evaluated observing the course of the optic nerve, obtained through the degree of its projection on the wall of the sphenoid sinus. The method used was the modified classification of Delano, evaluating the absence of bone reduction (dehiscence) of the optic nerve in the sphenoid sinus. We analysed the degree of pneumatization of the sphenoid sinus, using Hammer´s classification adapted by Guerrero, apart from the pneumatization of the anterior clinoidal process and pterigoid and the presence of the Onodi cell. Results: Most of the patients (78.96%) presented their optic nerve with a Type 1 course. Type 2 was observed in 16.83% of the patients, Type 3 in 3.47% and Type 4 in 0.74%. The presence of dehiscence of the optic nerve in the wall of the sphenoid sinus was evidenced in 21.29% of the cases. Related to pneumatization, we noticed that the pre-selar type was observed in 6.44%, the post-selar type appeared in 39.11%, the selar type appeared in 54.45%, and the apneumatized type was not observed in any of the cases. The pneumatization of the anterior clinoidal process was verified in 10.64% of the cases, while the pterigoid process was apparent in 21.29% of the cases. The Onodi cell (sphenoetmoidal) was found in 7.92% of the cases. Conclusion: The presence of dehiscence of the optic nerve is related with the degree of pneumatization of the anterior clinoid and the pterigoid processes, the presence of the Onodi cell (sphenoetmoidal) and Course Types 2, 3 and 4 considered the relationship between the optic nerve and the sphenoid sinus.
![]()
INTRODUCTION
Endoscopic surgery of facial sinuses has become a successful technique included in programs for training of otorhinolaryngologists1. Complications occur in 2.8% to 29% of the cases, according to different authors2. Among such complications, those affecting the optic nerve, causing ophthalmoplegia and blindness3, are the most important ones. These occurrences have encouraged studies of the optic channel, particularly, its anatomical relationship with the sphenoid and ethmoid sinuses. The great anatomical variability of the sphenoid and ethmoid sinuses is well documented4 6. Information available in the literature shows that certain areas are considered of high risk for injuries, such as the papyraceous lamina; ethmoidal floor, close to the anterior and posterior ethmoidal arteries; cribriform plate; the area between the posterior ethmoid and the sphenoid sinuses; and the postero-lateral wall of the sphenoid sinus5. In order to reduce the risks of complications, the anatomical knowledge of these areas is of utmost importance. Training in cadavers, along with increasing practical experience, will render safe surgical procedure1. Careful examination of such structures may be accomplished through preoperative computed tomography (CT). The purpose of this study is to evaluate the anatomical relationship between the optic nerve and the sphenoid sinus through CT scans and to determine the frequency of anatomical variations that could predispose patients to optic nerve injuries.
MATERIAL AND METHOD
A retrospective study of 202 computed tomography of facial sinuses from individuals of both genders, aged 14 and over, was conducted at the Imaging Department of Federal University of Sao Paulo (UNIFESP), from March 1998 to January 1999. Only normal scans and those showing sinus disease were evaluated. Postoperative scans of patients who underwent surgeries in the paranasal sinus and base of the skull or who had tumor lesions affecting these areas were not included. The CT scans were performed with devices Siemens DR and Shimatsu SCT-4500 T. The studied images included the coronal plane, perpendicular to the hard palate; the patients were placed in dorsal position, with head hyperextension (appropriate head support was used for this position), and the sections were 4.0/4.0 mm in width/ increment. Images scanned in axial plane were parallel to the hard palate; the patients were placed in dorsal position, with normal cervical position (with appropriate head support), and the sections were 4.0/4.0 mm in width/ increment. The images were scanned with 120/125 KV and 224/225 mAs. Tomographic windows used were 1500-2000 / 270-300 for bones and 320-350/ 35-40 (width/ level) for soft tissues.
Analysis of the optic nerve path
Scans of the optic nerve path were examined through its level of projection in the lateral sphenoid wall. The method used was Delano's Modified Classification into four types of optic nerve paths:
- type 1 - nerve path is close to the sphenoid sinus, without projecting into its wall (Figure 1).
- type 2 - nerve path is close to the sphenoid wall, projecting into its wall (Figure 2).
- type 3 - nerve path is close to the sphenoid wall, with visible projection, more than 50% of the optic nerve diameter is in the sphenoid sinus (Figure 3).
- type 4 - nerve path passes through the sphenoid sinus (total inclusion - Figure 4).
We also evaluated bone dehiscence, characterized by absence of bone reduction between the optic nerve and contents of the sphenoid sinus.
When we evaluated the type of pneumatization of the sphenoid sinus, we considered the level of pneumatization and sella turcica exposure. We used Hammer's7 classification adjusted by Guerrero8; however, we did not include the semi-sellar type. We considered sagittal plane sections of skull and we drew two imaginary lines, perpendicular to the sphenoidal plane: Line A, anterior to the sella turcica at the level of the sellar tuberculum, and Line B, at the posterior clinoid process (Figure 5). This evaluation was performed considering axial and coronal sections of a skull tomogram.
- nonpneumatized, sinus agenesis.
- conchal, small sinus, with slight pneumatization and without association with sella turcica.
- pre-sellar, pneumatization does not surpass, posteriorly, the vertical plane of the sellar tuberculum, i.e., it is tangent to Line A.
- sellar, pneumatization of the sphenoid sinus reaches the vertical plane of the posterior clinoid process, i.e., it is tangent to Line B. It is related to the anterior wall and floor of sella turcica.
- post-sellar, pneumatization of the sphenoid sinus surpasses Line B, perpendicular to the posterior clinoid process, it surpasses the sellar dorsum and may reach the occipital basilar process.
Evaluating the pneumatization of the pterygoideus (Figure 6) and anterior clinoid processes, we considered the air present in these structures.
In order to identify Onodi cells (Figure 8), we used the definition established at the International Conference for Sinus Disease. In this Conference, the anatomical terminology of paranasal sinuses was established according to Stammberger9, who defined the Onodi cells as "posterior ethmoidal cell located laterally or superiorly to the sphenoid sinus and closely associated with the optic nerve".
RESULTS
Four hundred and four optic nerves were evaluated in 202 patients. Chart I shows that the most frequently observed relationship was type 1, in 78.72% of the cases, where the optic nerve is close to the sphenoid sinus without projection into its wall. Type 2, with projection into the sinus wall, was noted in 16.83% of the cases; type 3, in which the optic nerve channel shows visible projection and more than 50% of the optic nerve diameter is in the sphenoid sinus, was found in 3.47% of the cases. In 0.74% of the cases, the nerve is included in the sphenoid sinus, the relationship between the path of the optic nerve channel and the sphenoid sinus is type 4. Chart II shows the distribution of dehiscence in the path of the optic nerve channel, noted in 21.29% of the cases. The main findings regarding the type of sphenoid sinus are depicted in Chart III, where we note a higher concentration of the sellar type in 54.45% of the cases. The post-sellar type occurred in 39.11% of the cases and pre-sellar in 6.44% of the cases. In Chart IV, we note pneumatization of the anterior clinoid process in 10.64% of the cases. The pneumatization of the pterygoideus process (Chart V) occurred in 21.29% of the cases. Chart VI depicts the distribution of Onodi cell, noted in 7.92% of the cases.
DISCUSSION
When we compared data concerning the level of projection of the optic nerve in the wall with those reported in the literature, we noted that Delano10 examined 150 CT scans, in axial and coronal sections, from patients over 13 years old and found type 1 in 76%; type 2 in 15%; type 3 in 6% and type 4 in 3% of the cases. We noted that our results concerning types 1 and 2 were similar. However, our study did not show the same results for types 3 and 4. The reason for such discrepancy is that we used a different definition for type 3, in which the nerves had a relevant projection (more than 50% of its diameter was inside the sphenoid sinus), and type 4, the optic nerve passes through the sphenoid sinus (it is included in the sphenoid sinus). In the terminology adopted by Delano10 the limits between types 3 and 4 are not clear. Data related to optic nerve dehiscence in the sphenoid wall ranges from 2% to 12%11,13 in studies conducted in skulls of dead bodies. This study, in which we used CT scans, registered 21.29% of optic nerve dehiscence. We noted that the percentage of dehiscence was highly variable in the literature. We also observed that the incidence of dehiscence was much higher in evaluations performed by CT scans. This variation may be due to CT inability to detect bone widths of less than 0.5mm14. Some authors11,13-16 reported in some cases, that the bone dividing the sphenoid sinus and the optic nerve is less than 0.5mm in width. Delano et al.10 found type 1 dehiscence in the optic nerve path in 7% of the cases; type 2 in 82%; and types 3 and 4 in 100% and 11.11% of the cases, respectively. When we evaluated the level of pneumatization of the sphenoid sinus, according to optic nerve projection and dehiscence, we noted that the increase in pneumatization was associated with higher level of projection and dehiscence of the optic nerve in the sphenoid wall. Some authors7,13,17,18 noted that the extensive pneumatization of the sphenoid sinus increases exposure and vulnerability of the optic nerve. The conchal sphenoid sinus was not seen in our study. According to the literature 6,7,19,20, this type is found in 3% to 25% of the cases. However, the authors did not mention the age of affected patients. Because this type of pneumatization is transitory during sinus development, they probably included in their study children of an age group in which the conchal type was more frequent. In the distribution for type of sphenoid sinus, the pre-sellar type occurred in 6.44% of the cases. The incidence for this type ranges from 11% to 29.2%6,7,14,19,20. These studies were conducted in cadavers, among which they included children and teenagers, what may explain the increased frequency of the pre-sellar type. To confirm our hypothesis, Guerrero8 reported pre-sellar type in 5% of the cases evaluated by MRI in adults. In our study, the sellar type occurred in 54.45% of the cases. Comparing this result with those reported in the literature7,11,17,21 , ranging from 76% to 86.67%, we noted that in our study, the incidence of sellar type was reduced. The authors classified the types of sphenoid sinus into conchal, pre-sellar and sellar, where pneumatization extended to the sphenoid body and, posteriorly, the clivus; therefore, the post-sellar type was included in this classification, resulting in higher occurrence of sellar type. Guerrero8 found 41.67% incidence of sellar type, whereas the incidence in our study was higher (54.45%). This may be explained by the inclusion of the semi-sellar type in the author's classification, reducing the incidence of sellar type. The post-sellar type was noted in 39.11% of the cases in our study. Lang20 found it in 47.6% of the cases, Navarro17 described pneumatization of the sphenoid sinus expanding to the occipital in 40% of the cases. Guerrero8 found the post-sellar type in 54% of the cases. As we can note, such discrepancies in the literature may be due to the material and method used for evaluation and the type of classification adopted. We used the classification in three types of sphenoid sinus because the definition through CT is simple. Pneumatization of the anterior clinoid process occurred in 10.64% of the cases, whereas literature shows an incidence ranging from 4% to 21%2,14,22 Delano et al.10 found pneumatization of the anterior clinoid process in 4% of the cases evaluated through CT scans. Dessi23 evaluated 150 CT scans and noted that the projection of the optic nerve into the sphenoid sinus was generally associated with pneumatization of the anterior clinoid process; however, the frequency of such anatomical variation was not described. The results of our study show an association between optic nerve dehiscence and pneumatization of the anterior clinoid process in 81.39% of the cases. Delano10 reported it in 77% of the cases, similar to the findings in our study. The frequency of pneumatization of the pterygoideus occurred in 21.29% of the cases, unilaterally in 5.94% and bilaterally in 15.34% of the cases, ranging from 15% to 43.6%1,12,14,22. Guerrero8, evaluating 300 MRI scans, found pneumatization of the pterygoideus process in 26.67% of the cases, unilateral in 11.00% and bilateral in 15.67% of the cases. As we can note, this aspect is controversial in the literature, even when the same methods are used. Many authors mentioned that pneumatization of the anterior clinoid and pterygoideus processes are anatomical changes predisposing to optic nerve injury12,14,18,22-24. As for distribution of Onodi cell, we noticed that it occurred in 7.92% of the cases. The description of the close morphological relationship between the posterior ethmoid sinus and the optic nerve was reported by Onodi27. Subsequently, other authors4,15,17,25 reported the vulnerability of the optic nerve in the posterior ethmoid and sphenoid sinuses. Incidence of Onodi cells ranges from 7% to 42%1,14,20,25,26. Some authors14,26 evaluated the head of cadavers using dissection through endoscope, and noted enlargement of structures and better visualization of anatomical details that could be missed by CT scans. This may explain the higher incidence of Onodi cell noted by such authors. On the other hand, our study shows results similar to those reported by Weinberger1 and Driben26 , when using CT scans. Driben26, in turn, questions CT reliability to detect Onodi cell. This limitation could occur when small segments of optic nerve were not detected in thicker sections26. We noted that in the literature, these discrepancies occur mainly due to differences in the concept of Onodi cell adopted by each author, the possible reason for the differences in results.
CONCLUSIONS
The sellar type sphenoid sinus was the most common one, and type 1 was the most common relationship between the optic nerve and the sphenoid sinus. Optic nerve dehiscence is associated with pneumatization of the anterior clinoid and pterygoideus processes and with types 2, 3 and 4 of the relationship between the optic nerve path and the sphenoid sinus. Onodi cell is associated with a higher incidence of optic channel dehiscence.
REFERENCES
1. Weinberger DG, Anand VK, Rawi A, Cheng HJ. Surgical anatomy and variations of the Onodi cell. Am J Rhinology 1996; 10:365-70.
2. Freedman HM, Kern EB. Complications of endoscopic intranasal ethmoidectomy: A review of 1000 consecutive operations. Laryngoscope 1987; 89:421-34.
3. Plate S, Asboe S. Blindness as a complication of rhinosurgery. J Laryngol 1981; 95: 317-22.
4. Hudgins PA. Complications of endoscopic sinus surgery the role of radiologist in prevention. Radiologic Clin North Am 1993; 31: 21-32.
5. Onish T, Tachibana T, Kaneko Y, Esaki S. High risk areas in endoscopic sinus surgery and prevention of complications. Laryngoscope 103:181-5.
6. Ouaknine GE, Hardy J. Microsurgical anatomy of the pituitary gland and the sellar region 2. The bony structures. Am Surg 1987; 53:291-7.
7. Hammer G, Radberg C. The sphenoidal sinus - An anatomical and oentgenoligic study with reference to transsphenoid hypophysectomy. Acta Radiol 1961; 56:401-22.
8. Guerrero AL. Pneumatização do seio esfenoidal de adultos e sua relação com o trajeto da artéria carótida interna - avaliação pela ressonância magnética. São Paulo, 1999. (Tese Doutorado - Escola Paulista de Medicina).
9. Stammberger HR, Kennedy DW. Paranasal sinuses: Anatomic terminology and nomenclature. In: International Conference on sinus disease: terminology staging therapy. Kennedy DW. Ann Otol Rhinol Laryngol Suppl 1995; 104: 7-31.
10. Delano MC, Fun FY, Zinreich J. Relationship of the optic nerve to the posterior paranasal sinuses: A CT anatomic study. AJNR Am J Neuroradiology 1996; 17(4): 669-75.
11. Fujii K, Chambers SM, Rhoton AL. Neurovascular relationships of the sphenoid sinus. A microsurgical study. J Neurosurg 1979; 50: 31-9.
12. Scuderi AJ, Harnsberger HR, Boyer RS. Pneumatization of the paranasal sinuses: normal features of importance to the accurate interpretation of CT scans in MRI images. AJR Am J Roentgenol 1993; 160: 1101-4.
13. Wigand EM. Endoscopic Surgery of the Paranasal Sinuses and anterior Skull Base. New York: 1990. p. 53-62.
14. Kainz J, Stammberger H. Danger areas of the posterior rhinobasis. An endoscopic and anatomical-surgical study. Acta Otolaryngol 1992 (Stockh) 112: 852- 61.
15. Bansberg SF, Harnes SG, Forbes S. Relationship of the optic nerve to the paranasal sinuses as shown by CT. Otolaryngol Head Neck Surg 1987; 96: 331-5.
16. Habal MB, Maniscalco JE, Rhoton AL. Microsurgical anatomy of the optic canal: correlates to optic nerve exposure. J Surg Res 1977; 22: 547-33.
17. Navarro J. Cavidade do nariz e seios paranasais. Anatomia Cirúrgica 1. Bauru All Dent; 1997. p. 109-16.
18. Terrier G. Rhinosinusal Endoscopy. Diagnosis and Surgery. Milano: Zambon Group 1991. P235-243.
19. Congdon ED. The distribution a mode of origin of septum in walls of the sphenoid sinus. Anat Rec 1920; 18 (2): 97-116.
20. Lang J. Clinical Anatomy of the Nose Nasal Cavity and Paranasal Sinuses. New York: Thieme; 1989. p. 70-98.
21. Vidic B. The postnatal development of the sphenoidal sinus and its spread into the dorsum sellae and posterior clinoid processes. Am J Roentgenol 1968; 104 177-83.
22. Bolger WE, Cliffort AB, Parsons DS. Paranasal sinus bony anatomic variations and mucosal abnormalities: CT analysis for endoscopic sinus surgery. Laryngoscope 1991; 101: 56-64.
23. Dessi P, Moulin G, Castro F, Chagnaud C. Protrusion of the optic nerve into to the ethmoid and sphenoid sinus: prospective study of 150 CT studies. Neuroradiology 1994; 36:515-6.
24. Mafee MF. Preoperative imaging anatomy of nasal ethmoid complex for functional endoscopic sinus surgery. Radiology Clin. North Am 1993; 31(1): 1-19.
25. Van Alyea OE. Sphenoid sinus. Anatomic study with consideration of the clinical significance of structural characteristics of the sphenoid sinus. Arch Otolaryngol 1941; 34: 225-53.
26. Driben JS, Bolger WE, Robles HH, Cable B. The reliability computerized tomographic detection of the Onodi (sphenoethemoid) cell. Am J Rhinology 1998; 12(2): 105-11.
27. Onodi A. The optic nerve and the accessory cavities of the nose. Ann Otol Rhinol Laryngol 1908; 17: 1-61.
Figure 1. Coronal section showing optic nerve with type 1 path.
Figure 2. Coronal section showing optic nerve with type 2 path.
Figure 3. Coronal section showing optic nerve with type 3 path.
Figure 4. Coronal section with optic nerve type 4 path.
Figure 5. Saggital section at the sphenoid level.
Figure 6. Coronal section showing pneumatization of anterior clinoid process.
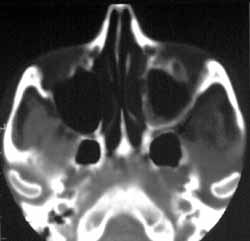
Figure 7. Axial section showing pneumatization of pterygoideus process.
Figure 8. Axial section showing presence of Odoni cells.
Chart 1. Distribution of types of optic nerve paths.
Chart 2. Distribution of optic nerve dehiscence.
Chart 3. Distribution of sphenoid sinus type.
Chart 4. Distribution of pneumatization of anterior clinoid process.
Chart 5. Distribution of pneumatization of pterygoideus process.
Chart 6. Distribution of presence of Odoni cells.