Year: 2004 Vol. 70 Ed. 5 - (6º)
Artigo Original
Pages: 612 to 621
Endoscopy of the internal auditory canal through retrolabyrinthine approach
Author(s):
Rafael B. Cahali1,
Michel B. Cahali2,
Rubens V. B. Neto2,
Ricardo F. Bento3,
Guilherme C. Ribas4
Keywords: internal auditory canal, retrolabyrinthine approach, endoscopy.
Abstract:
Introduction: The retrolabyrinthine approach is a safe route to the cerebellopontine angle, which allows preservation of hearing and facial nerve function. However, it doesn't allow a straight view of the whole internal auditory canal (IAC) with the operating microscope. The endoscopes may be used to assess the IAC during retrolabyrinthine approaches. The objective of this study is to evaluate the capabilities of different angled endoscopes in assessing the IAC. Methods: We performed the retrolabyrinthine approach in 40 temporal bones and then we measured the hidden distance in every quadrant as seen with the microscope and the 0°, 30° and 70° endoscope. Results: We observed that the hidden distances decreased, statistically, according to the optic used, in the following sequence: microscope, 0°, 30° and 70° endoscope. Only the 70° endoscope allowed a full view of the fundus of the IAC, which occurred in 27.5% of the cases. Partial view of the fundus of the IAC was possible in 67.5% of the bones with the 70° endoscope and in 12.5% with the 30° endoscope, whereas neither the 0° endoscope nor the microscope allowed any view of the fundus. The mean hidden distances at the superior-anterior quadrant measured with the microscope and the 0°, 30° and 70° endoscopes were, respectively: 10.4mm, 7.3mm, 4.3mm and 1.1mm. The 70° endoscope was significantly better than the others in the evaluation of the IAC and it should be considered the optic of choice in the assessment of the IAC during retrolabyrinthine approaches.
![]()
INTRODUCTION
The internal auditory canal (IAC) and the cerebellopontine angle (CPA) are the most difficult approaches to temporal bone. The evolution of science made it possible to diagnose small tumor lesions of CPA or those confined in the IAC in patients with few symptoms. Among all different CPA approaches the pre-sigmoid retrolabyrinthine approach presents itself as a craniotomy which is very close to this region, with the advantage of requiring minimal brain tissue retraction and preserving the capsule; however, it provides inadequate operative field for the assessment of IAC and is not indicated for total removal of tumors within that section1. PROTT 2 described the use of rigid endoscopes introduced through retrolabyrinthine approach to overcome this disadvantage of otomicroscopy and to assess the IAC through the internal acoustic pore. Some authors have been using this approach since then to remove tumors of this section by introducing endoscopes in the operative field to improve the IAC view.3,4,5.
DARROUZET et al.5 described the extended retrolabyrinthine approach with comprehensive drilling of the retro-sigmoid cortical bone and sectioning the endolymphatic duct, allowing increased retraction of the sigmoid sinus and the dura from the posterior fossa, extending the exposure of the CPA section. Nevertheless, the lateral third of the IAC still remained hidden to otomicroscopy in this approach.
The endoscope angulations used in retrolabyrinthine approaches varied in scientific studies, and some investigators used optic devices ranging from 0o 6, 30o 7 and 70o 8 degree angle. According to our knowledge, there are no studies assessing the IAC field of visualization obtained with different optic angulations. The objective of this study was to compare the ability of surgical microscope and 0o, 30o and 70o angled rigid endoscopes in assessing IAC during pre-sigmoid retrolabyrinthine craniotomy in order to quantify the hidden portion of IAC in each quadrant and the likelihood of viewing the IAC fundus.
MATERIAL AND METHOD
MATERIAL
The study was performed in 40 human temporal bones collected from necropsies conducted in the Death Analysis Center in the City of Sao Paulo, University of Sao Paulo, upon previous consent by the Ethical Committee of our institution.
The study included only samples with the following preserved anatomic structures: sigmoid sinus, dura of the medial and posterior fossa , petrous apex, and the inner structures the IAC. Initially, the study included 48 bones of adult individuals from both genders, victims of nonviolent death. The bones were fixed in 10% formaldehyde solution until handling. Temporal bones that underwent accidental burring of the labyrinth bone during the process of drilling away to IAC exposure (vestibule or posterior or anterior semicircular canal) were the main factors of exclusion of eight bones from this study. Pieces with anatomical anomalies such as: perforation, tympanic membrane retraction, tumor, signs of previous surgical procedure and presence of fracture traces were also excluded.
Temporal bones were collected from 23 male and 17 female corpses. Races were as follows: 32 Caucasian, six pardo (Brazilian native) and two African-descendents. Average age ranged from 62.8 ± to 13.3 years (ranging from 25 and 93 years). Twenty bones were studied for each side.
METHOD
All IAC content was removed using surgical microscope before burring the mastoid. Next, temporal bone was placed into operative position over a support for retrolabyrinthine approach. Extended mastoidectomy was then performed with removal of up to 3 cm of the cortical bone posteriorly to the sigmoid sinus, which was exposed from the jugular bulb to the petrous apex. All three semicircular canal were skeletized and after sectioning the endolymphatic duct and retracting the dura posteriorly and the sigmoid sinus, the bone wall was burred posteriorly to the IAC for an 1800 exposure of its inner portion.
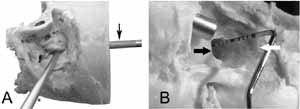
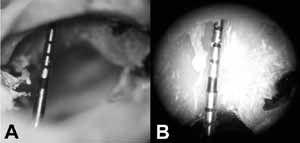
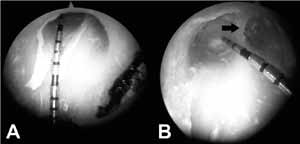
In order to measure the IAC depth, we used angled-measuring device with 15 mm of useful length (model PUNC 15, G. HARTZELL & SON, CA, USA). Although it was graduated in millimeters, the image magnification of the measuring device with the surgical microscope or with the endoscopes allowed us to define, based on visual assessment, the tenth of millimeter in each measure. The measuring device was introduced in the IAC, according to its larger axle and was kept parallel to the walls, in four different positions: anterior-superior, anterior-inferior, posterior-superior and posterior-inferior (figure 1). This introduction occurred until central portion of the fundus was touched in each quadrant of the IAC. Next we reported, under the best angle of view possible through retrolabyrinthine approach, the most distal point to the measuring device that was visible in each one of the assessed quadrants, first with the surgical microscope (25 X magnification) and then with rigid endoscopes (4 mm external diameter and 18 cm of working length, KARL STORZ, Germany) angled as follows: 0o degree (model 7210AA), 30o (model 7210BA) and 70o (model 7210CA) (figures 2 and 3). Therefore, the invisible distance was measured up to the fundus of the IAC in each one of its quadrants using these different optic devices. Additionally, the number of samples that allowed us to see the IAC fundus in at least one quadrant was also reported with each one of the optic devices. We also measured the smaller distance in millimeters from the sigmoid sinus to the posterior semicircular canal (SS CSCP).
The variables analyzed in this study presented normal distribution, therefore data were subjected to parametric tests.
Corpses from both genders were compared in regards to all measures taken from all temporal bones using Student's t-Test controlled by Levene test for variance equality. The same test was used to compare the measures of samples from the right side against those of the left side. In order to evaluate the impact of age over the measures taken and to check the relation between the distances of the sigmoid sinus from the posterior semicircular canal through IAC measurement we used Pearson's correlation coefficient. Then each instrument was compared across the mean measures of the IAC for each quadrant through paired data Student's t-Test. The same test was applied to compare each quadrant against each other according to the measures taken using the same optic instrument.
Variance analysis controlled by Dunnet test was applied to evaluate likely differences in the capacity of viewing the fundus of the IAC demonstrated by the different instruments.
The level of significance adopted was below 0.050.
RESULTS
No statistically significant gender-related differences were found in the measurements of the temporal bones except for the invisible mean distance of the IAC in the posterior-inferior quadrant with the 70o angled endoscope, which was higher in female samples (mean ranged from 3.1 ± 1.8mm in females and from 1.4 ± 1.8mm in males; p=0.007). In regards to anatomic piece, we reported that most of the measurements of the IAC performed in the right side were significantly higher than those from the left side. SS-CSCP distance, however, was not significantly different in both sides (mean ranged from 6.4 ± 2.9mm on the right side and from 6.3 ± 1.7mm on the left side; p=0.947).
No correlation was found between age and measurements of IAC performed for all optic instruments. Positive correlation was found between the age and SS-CSCP distance (r=0.405; p=0.010). The same distance was also found to be positive and significantly related to the invisible distance of the IAC measured from both upper quadrants with the surgical microscope and such relation was not found in the assessment performed with endoscopes.
Mean of the measurements performed in the IAC are described in Table 1. We could observe that the mean hidden distance of the IAC in each one of the four quadrants was significantly higher if it was performed with surgical microscope against those performed with endoscopes. Likewise, the mean distances of those measures were significantly higher if performed with 0o angled endoscope against those performed with 30o angled endoscope whose means were also significantly higher against those performed with 70o angled-endoscope. Graph 1 shows the reduction of the hidden distance of the anterior-posterior quadrant of IAC with the use of optic devices sequenced as follows: microscope, 0o, 30o and 70o angled endoscope. This pattern was found in all quadrants.
The number of samples in which the IAC was visible in different quadrants with each optic instrument is described in Table 2. Only the 70o angled endoscope allowed visualization of the fundus in all quadrants of the IAC of the same temporal bone. It occurred in 11 bones (27.5%). This same endoscope allowed visualization of the fundus in at least one of the IAC quadrants in 27 bones (67.5%). The number of samples in which the IAC funds was visible with the 70o angled endoscope was statistically higher than the number of samples in which the fundus was visible through other optics (p<0.005).
The 30o angled endoscope allowed visualization of the fundus only in two quadrants of the IAC and in only five samples (12.5%); therefore, no statistically significant difference was found between the surgical microscope and the 0o degree-angled endoscope that did not allow visualization of the fundus in any of the IAC quadrants of the dissected pieces.
Measurements performed with surgical microscope showed that the mean hidden distance of the IAC was significantly higher for the anterior-superior quadrant against the anterior-inferior one (p=0.007), with the latter being significantly higher than that of the posterior-superior quadrant (p=0.022), which, in turn, was significantly higher than that of the posterior-inferior quadrant (p=0.001) (table 1). Measurements performed with 0o angled endoscope demonstrated that the mean hidden distance of the IAC was statistically higher in the anterior-superior quadrant than that of other quadrants (p<0.005 in three comparisons), and the mean hidden distance of the IAC was statistically higher in the posterior-superior quadrant than in the posterior-inferior one (p=0.007), with no statistically differences found in paired comparisons among the other quadrants.
Contrarily to the surgical microscope and the 0o angled endoscope, the 30o and 70o degree-angled endoscopes allowed closer view of the fundus of the IAC in the anterior quadrants. Thus, with the 30o angled endoscope, the mean hidden distance of the IAC was significantly higher in the posterior-superior quadrant of both anterior quadrants (p<0.050 in two comparisons); this distance was higher in the posterior-inferior quadrant against the anterior-inferior one (p<0.001), and was also higher in the anterior-superior quadrant against the anterior-inferior one (p=0.009), with no statistically significant differences found in paired comparisons among the other quadrants.
In the 70o angled endoscope, however, this mean was significantly higher in the posterior quadrants against the other two anterior quadrants (p<0.001 in these four comparisons), without significant differences found in other comparisons.
DISCUSSION
Human IAC shows high degree of bilateral symmetry 9, with no differences found in its length in both genders, with no correlations between size and age10. We did not check IAC dimensions previously to drilling in our study; but it is likely that those dimensions would explain why we found hidden portions in bones of the right side against those of the left side. No correlation was found between our IAC measurements and the age of subjects; however, a positive correlation of the SS-CSCP distance and age was observed, with no plausible explanations for this fact. No differences were found in any of the measurements related to gender except for those performed in the posterior-inferior quadrant of the IAC with the 70o angled endoscope, which had mean hidden distance higher in female samples. Since this was the only one out of 16 parameters with differences between genders, we believe that this is simply an occasional fact.
As a principle, the closer to the intracranial lesion the craniotomy is performed, the better will be surgical handling. The retrolabyrinthine craniotomy provides direct approach to CPA, but the linear view of the IAC is hindered through this approach. The lowest hidden distance obtained with otomicroscopy was 5.0 mm (mean distance was 10.4 mm in the anterior-posterior quadrant). Otomicroscopy was inadequate for the assessment of IAC to check the presence of residual tumors.
One of the possibilities to improve the angle of the linear view of IAC was through retrosigmoid craniotomy 11,12, which does not expose to otomicroscopy 3 to 4 mm of IAC lateral portion 13,14,15. On the other hand, in suboccipital approaches, this obscure part varies from 2mm16,17 to zero18,19, according to the approach used it gets closer to the median sagittal line of the skull. Thus, progressive retraction of the cerebellum is required in this kind of approach.
Technically speaking, it is possible to anteriorly extend the retrolabyrinthine craniotomy 20,21,22, and count on the chance of hearing preservation, as exeresis of the posterior semicircular canal 23. Even with such extension, this approach could assess only 61% of the medial portion of the IAC with surgical microscope24. It is important to point out the difficulty in drilling the IAC and to preserve the bone labyrinth through retrolabyrinthine approach. Due to this fact, eight out of forty-eight bones studied (16.7%) were excluded.
The lack of reliable anatomic parameters to identify drilling limits of the IAC in this approach was one of our major difficulties in this study.
It is also important to highlight that some authors consider the retrolabyrinthine approach excessively exiguous for the exeresis of tumor lesions of the IAC portion1,11,25, emphasizing that tumor extension inside IAC could be underestimated in Magnetic Resonance Imaging (MRI) 26.
Besides sigmoid sinus retraction we also performed sectioning of the endolymphatic duct of the studied pieces, since it allowed us to extend drilling of the posterior wall of the IAC without damaging hearing or vestibular functioning 5,6,7. The SS-CSCP distance was not related to any measurements evaluated with endoscopes, since such endoscopes exceeded the narrowing caused by sigmoid sinus during IAC assessment. Surgical microscope, however, showed a positive correlation between hidden distances in the two superior quadrants of the IAC and SS CSCP distance, indicating that the angle of view of the IAC became more favorable in those pieces with sigmoid sinuses closer to the posterior semicircular canal.
Some authors have been using rigid endoscopes to assess inside the IAC in retrolabyrinthine approaches and optic devices used were 0o 6, 30o 7 or 70o 8 angled endoscopes. Others used such devices to assess IAC 27 after tumor exeresis in retro-sigmoid or sub-occipital29 approaches 3,28. As far as we know, this study is the first one to measure the hidden distances of the IAC using endoscope with different angulations.
In spite of the fact that the 0o angled endoscope was statistically better than the microscope in the assessment of the IAC, it still leaves 6mm hidden in all quadrants through retrolabyrinthine approach. Therefore, it was proved to be a low capacity optic device to assess IAC lesions, which could be misinterpreted as sectioned vestibular nerves30.
The 30o degree-angled endoscope was statistically better for IAC assessment than 0o angled endoscope and the microscope. Its advantage against the 70o degree-angled endoscope was that it was easier to handle, since it allows linear visualization which makes its introduction in the skull presumably safer.
The 30o angled endoscope or the microscope were not statistically better than the 0o degree model in terms of ability to view the fundus of the IAC. If we take into account that the 30o model had, on average, more than 4mm hidden in all quadrants of the IAC, in our opinion it is a low capacity instrument to assess this structure through retrolabyrinthine approach.
We found out that the 70o angled endoscope showed the shortest hidden distances in all quadrants. This optic could show the IAC fundus in 67.5% of all bones studied. The greatest hidden distance measured with this instrument was on average 2.1mm in the posterior quadrants of the IAC, achieving 1.0 and 1.1 mm in the anterior-posterior quadrants. Considering that retrolabyrinthine approach is indicated for vestibular schwanomas surgeries with small intracanalicular tumor extension, in our opinion, the 700 optic met the needs for proper assessment of inner IAC through retrolabyrinthine approach. Although it is an instrument tougher to be handled than the others - it does not provide linear view - practice in using it for anatomic dissections of IAC through this approach could turn it into a useful tool in operative routine.
CONCLUSION
The ability to assess the IAC with different optic instruments through retrolabyrinthine approach demonstrated that hidden distances found in each quadrant were progressive and significantly smaller according to the following sequence of instruments: surgical microscope, 0o, 30o and 70o angled endoscopes. The 70o endoscope proved to be significantly better against the other instruments for visualization of IAC fundus.
REFERENCES
1. Hitselberger WE, Pulec JL. Trigeminal nerve (posterior root) retrolabyrinthine selective section. Operative procedure for intractable pain. Arch Otolaryng 1972;96:412-5.
2. Prott W. Cisternoscopy - Endoscopy of the cerebellopontine angle. Acta neurochir 1974;31:105-13.
3. Magnan J, Chays A, Caces F, et al. Contribution of endoscopy of the cerebellopontine angle by retrosigmoid approach. Apport de l'endoscopie de l'angle ponto-cérébelleux par voie rétro-sigmoïde. Ann Otolaryngol Chir Cervicofac 1993;110:259-65.
4. Bento RF, De Brito RV, Sanchez TG, et al. The transmastoid retrolabyrinthine approach in vestibular schwannoma surgery. Otolaryngol Head Neck Surg 2002;127:437-41.
5. Darrouzet V, Guerin J, Portmann D, et al. La voie rétro-labyrinthique élargie: application à la chirurgie du neurinome de l'acoustique. Rev Laryngol Otol Rhinol (Bord) 1993;114:207-11.
6. Prades JM, Martin C, Chelikh L, et al. Voie d'abord retro-labyrinthique "Optimisée". Intérêt dans l'endoscopie de l'angle ponto-cérébelleux. Ann Otolaryngol Chir Cervicofac 1995;112:46-51.
7. Martin C, Pradres JM, Loubeyre A, et al.. La voie rétrolabyrinthique élargie. Intérêt dans la chirurgie du neurinome de l'acoustique avec tentative de conservation auditive. Rev Laryngol Otol Rhinol (Bord) 1995;116:119-22.
8. Darrouzet V, Tessier B, Guerin J, et al. La voie rétrolabyrinthique élargie: application à la chirurgie du neurinome de l'acoustique. A propos de 55 cas. Ann Otolaryngol Chir Cervicofac 1996;113:307-19.
9. Amjad AH, Scheer AA, Rosenthal J. Human internal auditory canal. Arch Otolaryngol 1969;89:51-56.
10. Papangelou L. Study of the human internal auditory canal in relation to age and sex. J Laryngol Otol 1975;89:79-89.
11. Silverstein H, Norrell H, Haberkamp T. A comparison of retrosigmoid IAC, retrolabyrinthine, and middle fossa vestibular neurectomy for treatment of vertigo. Laryngoscope 1987;97:165-173.
12. Glasscock ME, Thedinger BA, Cueva RA, et al. An analysis of the retrolabyrinthine vs. the retrosigmoid vestibular nerve section. Otolaryngol Head Neck Surg 1991;104:89-95.
13. Blevins NH, Jackler RK. Exposure of the lateral extremity of the internal auditory canal through the retrosigmoid approach: a radioanatomic study. Otolaryngol Head Neck Surg 1994;111:81-90.
14. Tatagiba M, Matthies C, Samii M. Microendoscopy of the internal auditory canal in vestibular schwannoma surgery. Neurosurgery 1996;38:737-40.
15. Haberkamp TJ, Meyer GA, Fox M. Surgical exposure of the fundus of the internal auditory canal: anatomic limits of the middle fossa versus the retrosigmoid transcanal approach. Laryngoscope 1998;108:1190-4.
16. Domb GH, Chole RA. Anatomical studies of the posterior petrous apex with regard to hearing preservation in acoustic neuroma removal. Laryngoscope 1980;90:1769-76.
17. Palva T, Troupp H. Suboccipital removal of vestibular neurinoma with preservation of the labyrinth. Ann Clin Res 1986;18:33-6.
18. Laine T, Johnsson LG, Palva T. Surgical anatomy of the internal auditory canal. A temporal bone dissection study. Acta Otolaryngol 1990;110:78-84.
19. Mazzoni A, Calabrese V, Danesi G. A modified retrosigmoid approach for direct exposure of the fundus of the internal auditory canal for hearing preservation in acoustic neuroma surgery. Am J Otol 2000;21:98-109.
20. Sekhar LN, Schessel DA, Bucur SD, et al. Partial labyrinthectomy petrous apicectomy approach to neoplastic and vascular lesions of the petroclival area. Neurosurgery 1999;44:537-50.
21. Magliulo G. Modified retrolabyrinthine approach with partial labyrinthectomy: anatomic study. Otolaryngol Head Neck Surg 2001;124:287-91.
22. Chanda A, Nanda. A Partial labyrinthectomy petrous apicectomy approach to the petroclival region: an anatomic and technical study. Neurosurgery 2002;51:147-59.
23. Molony TB, Kwartler JA, House W, et al. Extended middle fossa and retrolabyrinthine approaches in acoustic neuroma surgery: case reports. Am J Otol 1992;13:360-363.
24. Vrabec JT, Pachigolla R. A temporal bone study of endoscopy of the cerebellopontine angle posterior semicircular canal resection for exposure of the internal auditory canal (PSCC resection). Acta Otolaryngol 1999;119:858-62.
25. Sanna M, Falcioni M, Taibah A, et al. Treatment of residual vestibular schwannoma. Otol Neurotol 2002;23:980-7.
26. Selesnick SH, Rebol J, Heier LA, et al. Internal auditory canal involvement of acoustic neuromas: surgical correlates to magnetic resonance imaging findings. Otol Neurotol 2001;22:912-6.
27. Rak R, Sekhar LN, Stimac D, et al.. Endoscope-assisted microsurgery for microvascular compression syndromes. Neurosurgery 2004;54:876-81.
28. Wackym PA, King WA, Poe DS, et al. Adjunctive use of endoscopy during acoustic neuroma surgery. Laryngoscope 1999;109:1193-201.
29. McKennan KX. Endoscopy of the internal auditory canal during hearing conservation acoustic tumor surgery. Am J Otol 1993;14:259-262.
30. Driscoll CL, Jackler RK, Pitts LH, et al. Is the entire fundus of the internal auditory canal visible during the middle fossa approach for acoustic neuroma? Am J Otol 2000;21:382-8.
GRAPH 1 - MEAN AND STANDARD DEVIATION OF INVISIBLE DISTANCE IN THE ANTERIOR-POSTERIOR QUADRANT OF INTERNAL ACOUSTIC CANAL (IAC) ACCORDING TO THE OPTIC INSTRUMENT USED.
TABLE 1 - MEAN INVISIBLE DISTANCE OF THE IAC ACCORDING TO THE OPTIC INSTRUMENT USED IN EACH QUADRANT. (1)
(1) Data expressed in mm.
* p<0.001 in comparison with the instrument in the row immediately to the right.
TABLE 2 - NUMBER OF PIECES IN WHICH THE FUNDUS OF THE IAC WAS VISIBLE ACCORDING TO ITS QUADRANT.
1 Pieces in which IAC fundus was visible in at least one of its quadrants.
2 Pieces in which IAC was visible in all quadrants.
* p<0.001 if compared against the other instruments.
**p=0.003 if compared against other instruments.
Figure 1. A: insertion of the measuring device (arrow) and of the endoscope (*) on the left side of temporal bone. B: direct view of the internal auditory canal (IAC) with the measuring device inside it and the endoscope inserted through retrolabyrinthine (large black arrow: posterior rim of the IAC, white large arrow: anterior rim of the IAC).
Figure 2. A: View of the anterior-inferior quadrant with the measuring device under the microscope. B: View of the anterior-inferior quadrant with 00 angled endoscope measuring device.
Figure 3. A: Anterior-inferior view with 30o model endoscope. B: Anterior-inferior view of measuring device with 700 angled endoscope. Arrow indicating the transversal crest.
(1) PhD Studies under course, Discipline of Otorhinolaryngology, Hospital das Clinicas, Medical School, University of Sao Paulo- USP.
(2 )PhD in Otorhinolaryngology, Medical School, USP.
(3)Ph.D., Professor of Otorhinolaryngology, Medical School, USP. (4)PhD, Neurology, Medical School- USP .
Study carried out by Department of Otorhinolaryngology, HCFMUSP
Address correspondence to Rafael B. Cahali,
Rua Macau, 232. Sao Paulo, SP 04032-020, Brasil.
Phone: (55 11) 5579-1299
Fax: (55 11) 5579-1299
Email: rafaelcahali@terra.com.br