Year: 2004 Vol. 70 Ed. 3 - (21º)
Relato de Caso
Pages: 423 to 426
Localized laryngeal amyloidosis: case report and literature review
Author(s):
Fabiana C. P. Valera 1,
Denílson S. Fomin 1,
Gilberto S. Maggioni Jr. 2,
Marcos Grellet 3
Keywords: amyloidosis, larynx
Abstract:
Localized laryngeal amyloidosis is a rare disease, corresponding to less than 1% of benign tumors in larynx. However, localized amyloidosis occurs mostly in larynx, being of great importance its diagnose by Otorhinolaryngologists. It is related to monoclonal production of light chain immunoglobulins, mainly l and k. This study has the purpose of relating a case of laryngeal amyloidosis assisted in Laryngology and Voice Clinics at Clinics Hospital FMRP - USP, and discussing literature as well.
![]()
Introduction and Literature Review
Amyloidosis is characterized by a group of diseases of protein deposits that have fibrillar nature and specific staining properties. They can be classified into localized or systemic, according to fibrillar protein precursors. The most widely accepted classification is that of International Amyloidosis Society, in 19901, which divided amyloidosis into:
- type AA (or secondary): comprises reactive systemic amyloidosis, associated with chronic inflammatory disease and occasionally neoplasms, and family Mediterranean fever. Formed by serum A amyloid.
- type AL (or primary): formed by monoclonal light chain ( or ) of immunoglobulin. They comprise primary systemic amyloidosis, amyloidosis associated with myeloma, monoclonal gamopathy, or occult dyscrasia and localized amyloidosis.
- type ATTR: comprising senile systemic amyloidosis, and family amyloid polyneuropathy and cardiomiopathy. Formed by transtiretin (or pre-albumin).
- type A 2M: formed by microglobulin 2. Comprising periarticular amyloidosis and systemic amyloidosis associated with renal failure and dialysis for prolonged periods of time.
- type A : formed by protein precursor. Comprises Alkheimer's disease and some cases of Down Syndrome.
Localized amyloidosis is a rare disease (amounting to less than 1% of benign laryngeal tumors 2) and of unknown cause. It is located especially in the aerodigestive tract 3, 4 (in special the larynx) and skin 5.
Since 1875, when Burow and Neumann first described laryngeal amyloidosis, just about 300 cases have been reported in the literature 6. Even though laryngeal amyloidosis is rare, the larynx is the most commonly affected site by localized amyloidosis, especially in the supraglottic region 7.
Case Report
UMPC, 33-year-old female patient, she came to Hospital das Clínicas, Medical School, Ribeirão Preto, with history of dysphonia for 6 months, without dyspnea, apnea, swallowing disorders or other symptoms. She did not report vocal abuse, smoking or quick weight loss.
Fibroscopy showed yellowish subepithelial nodular small lesion in the anterior commissure, without other laryngeal affections (Figure 1).
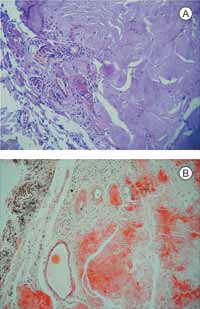
In 1999, the patient was submitted to biopsy under direct laryngoscopy, and the biopsy showed extensive and dense amorphous eosinophilic material, stained with Congo red, which resulted in the diagnosis of laryngeal amyloidosis (Figures 2a and 2b).
We conducted neck CT scan which evidenced mild thickness at the level of the anterior commissure, without affection of the other portions of the larynx and upper third of the trachea, and absence of adenomegalia.
We used tests to exclude systemic amyloidosis (chest and abdomen x-ray, abdominal ultrasound, liver and renal function, glucose level, reactive protein C, protein electrophoresis, routine urine tests, and biopsy of umbilical fat), immune diseases (rheumatoid factor, ANCA and ANA) and multiple myeloma (Bence Jones protein), being that all of them were normal.
Owing to the small residual size of the lesion after biopsy and the benign behavior of the disease in most cases, we decided to clinically follow-up her every month for six months and then started 6-month interval follow-up, with fibroscopy. The patient remained with mild dysphonia, and no other symptoms. The last fibroscopy, three years and a half after the initial diagnosis, showed mild synechia in the anterior commissure, without increase in dimension of lesion.
Figure 1: Laryngeal endoscopic image, evidencing amyloid lesion in vocal fold anterior commissure.
Figures 2a and 2b: Biopsy of laryngeal amyloid tissue, Hematoxylin-Eosin staining (figure 2a) and Congo Red (figure 2b).
Discussion
Localized laryngeal amyloidosis type AL has as precursor monoclonal dyscrasia of plasma cells, which leads to formation or protein subunit of fibrils derived from light chain immunoglobulin (or)5, being that the light chain is more prone to forming amyloids than chain.
Amyloidosis may occur owing to production of immunoglobulins, both structurally abnormal or in excessive number, by monoclonal plasma cells. Amyloid deposits would occur owing to difficulty to metabolize the produced fibrils.
Larynx is the most commonly affected site by localized amyloidosis, especially the vocal folds. The multiple location in the airways may also be detected, being that it is frequently associated with tracheal affection 8.
The most common symptom of laryngeal amyloidosis is dysphonia, rarely followed by other symptoms such as dyspnea, odynophagia, inspiration stridor, aspiration, chocking or pharyngeal fullness.
The examination of the lesion should comprise endoscopic analysis, direct laryngoscopy, and imaging tests (MRI or preferably, CT scan) to identify the lesion extension. At fibroscopy, the aspect of the lesion is yellowish nodular non-ulcerated damage with subepithelial deposits.
The diagnosis is confirmed by biopsy, evidencing extracellular homogenous amyloid, amorphous and eosinophilic deposits. During Congo red staining, we can see typical greenish birefringence by polarization microscopy.
Immunohistochemistry evidences monoclonal amyloid deposits for light chain immunoglobulins or , whereas plasma cells producers of immunoglobulin have polyclonal pattern for chains that are both and 8.
Owing to slow evolution and mild symptoms of localized amyloidosis, the treatment of choice is removal of the lesion via endoscopic access (preferably with carbon dioxide laser), only in symptomatic cases 5, 6, 7, 8. The initial objective of the surgery should be to remove the visible amyloid, without wide resections.
In rare cases in which the extension of the disease is very wide, in cases of frequent recurrence, we indicate external surgical resections. Kennedy et al.6 suggested that the most appropriate external surgery is lateral supraglottic external surgery, since it is more conservative, preventing complications such as swallowing and voice affections.
Most authors in the literature 6, 8, 9, 10, 11 agreed that treatment with immunomodulators (chemotherapy, corticoids or radiotherapy) should be avoided because of impairment of immune response of the patients, which can speed up the process of amyloid deposit.
According to Lewis et al.8, recurrence of localized amyloidosis is variable, and it may occur many years after the first surgery. It is more expressive in cases in which we can observe the diagnosis of more extensive lesion. However, cases that lead to death owing to respiratory obstruction are very rare or they are cases of systemic amyloidosis 2, 6, 8.
Closing Remarks
Laryngeal amyloidosis is a rare affection, however it should be considered in the differential diagnosis of laryngeal benign lesions. The management should always be less aggressive as possible, indicating surgery only in symptomatic cases. Clinical follow-up should be made for long periods of time, since recurrence may occur late.
References
1) Husby G, Araki S, Benditt EP et al. The 1990 guidelines for nomenclature and classification of amyloid and amyloidosis. In: Natvig JB, Förre Husby G et al, eds. Amyloid and amyloidosis. Vth International Symposium on Amyloidosis. Norway. Dordrecht: Kluwer Acamedic, 1990: 5-11.
2) Godbersen GS, Leh JF, Hansmann ML, Rudert H, Linke RP. Organ-limited laryngeal amyloid deposits: clinical, morphological and immunohistochemical results of five cases. Ann. Otol. Rhinol. Laryngol, 1992; 101: 770-775.
3) Simpson GT II, Strong MS, Skinner M, Cohen AS. Localized amyloidosis of the head and neck and upper aerodigestive and lower respiratory tracts. Ann. Otol. Rhinol. Laryngol. 1984; 93: 374-9.
4) Mufarrij AA, Busaba NY, Zaytoun GM, Gallo GR, Feiner HD. Primary localized amyloidosis of the nose and paranasal sinuses. Am. J. Surg. Pathol. 1990; 14: 379-83.
5) Berg AM, Troxler RT, Grillone G, Kanznica J, Kane K et al. Localized amyloidosis of the larynx: evidence for light chain composition. Ann. Otol. Rhinol. Laryngol. 1993; 102: 884-889.
6) Kennedy TL, Patel NM. Surgical management of localized amyloidosis. Laryngoscope 2000; 110: 918-23.
7) Clark JM, Weissler MC. Localized laryngotracheobronchial amyloidosis: case report and review of the literature. Ear Nose Throat J. 2001; 80: 632-637.
8) Lewis JE, Olsen KD, Kurtin PJ, Kyle RA. Laryngeal amyloidosis: a clinicopathologic and immunohistochemical review. Otolaryngol. Head Neck Surg. 1992; 106: 372-7.
9) Mitrani M. Biller HF. Laryngeal amyloidosis. Laryngoscope 1985; 95: 1346-7.
10) Rubinow A, Celli BR, Cohen AS et al. Localized amyloidosis of the lower respiratory tract. Am. Rev. Respir. Dis. 1978; 118: 603-11.
11) Friedman I. Nose, throat and ears. In: Symmers WS, ed. Systemic Pathology. 3rd ed. New York; Edinburgh: Churchill Livingstone, 1987: 203-5.
1 Associated physician, Discipline of Otorhinolaryngology, Medical School, Ribeirão Preto - University of Sao Paulo
2 Associated physician, Discipline of Pathology, Medical School, Ribeirão Preto - University of Sao Paulo
3 Full and associated professor, Medical School, Ribeirão Preto - University of Sao Paulo
Affiliation: Hospital das Clínicas, Medical School, Ribeirão Preto- University of Sao Paulo
Av. Bandeirantes, 3900 - Bairro Monte Alergre - Ribeirão Preto - SP
e-mail: facpvalera@uol.com.br