Year: 2004 Vol. 70 Ed. 2 - (21º)
Relato de Caso
Pages: 278 to 282
Isolated laryngeal candidiasis in a immunocompetent patient: a case report and a literature review
Author(s):
Paulo S. L. Perazzo 1,
Luiz Ricardo L. Martin 2,
Milton Pamponet da Cunha Moura 3,
Max Adrian M. Melo 4,
Márcio da Silva Carvalho 5
Keywords: candidiasis, larynx, isolated
Abstract:
After a literature revision it is confirmed that the larynx candidiasis is rare and usually associated with lungs infection or systemic candidiasis. The larynx isolated form is more rare and seldom associated to immunological disease. It is known that through endoscopic examination, the candidiasis of larynx can show a single local erythema or leucoplasy, simulating G.E.R.D. or even neoplasia, which are the main differential diagnosis. We reported in our hospital an immunocompetent patient with isolated laryngeal candidiasis. There was an important involvement of larynx with degenerative lesions on epyglote, simulating a neoplasic process. The diagnosis was confirmed by biopses and histophatologic analyses. We crossed off hypotheses corticosteroids and antibiotics abuse. We followed up during and after the treatment with antifungeal by the use of endoscopic and clinical improvement.
![]()
INTRODUCTION
By means of literature review, we can confirm that laryngeal infection by candida is a rare disease 1. Clinical manifestation of candida laryngitis can mimic pathologies such as GERD, granulomatous diseases and even carcinomas 2, 4. In fact, Forest and Weed described a case of laryngitis with hyperemia and leukoplasia, initially treated as GERD, diagnosed as isolated laryngeal candidiasis after therapeutic failure. Thus, laryngeal infection by candida can manifest as simple hyperemia, edema leukoplasia, as well as vocal dysphonia and fatigue 2.
Isolated laryngeal candidiasis is not a common pathology as secondary form of systemic disease or associated pulmonary impairment 3, 5, 6. Mycotic infections involving the larynx as secondary infection are relatively common in immunocompromised patients, which is part of the differential diagnosis of infections that affect upper airways of these patients 3, 5-7. Conversely, laryngeal impairment is not frequent in immunocompetent patients, and in these patients, it is even more rare to find cases of isolated laryngeal infection 1, 2, 7. The literature has reports of few cases of laryngitis by candida as isolated infection in patients that did not present immune deficiency 1, 2, 4, 6, 8. In immunocompetent patients, mycotic infections tend to have a chronic or subacute character. Therefore, quick evolution of mycotic infectious process favors immunodeficiency. The typical clinical pattern of manifestations of upper airways' mycotic infections is impairment to mucosa with ulceration, even though other diseases can cause the same characteristics 2, 4, 6, 8.
Most mycotic infections in humans are secondary to fungi inhalation. Opportunistic fungi, such as candida albicans, are found as part of the normal flora of the area. Infections caused by these fungi are normally opportunistic because they reveal a rupture in the natural defense mechanism of the host, inducing active infection.
The diagnosis of mycotic laryngitis is confirmed through direct laryngoscopy with biopsy of tissues, elucidating the diagnosis 1-9. The material sent to histopathological analysis, routinely stained with hematoxylin-eosin (HE) does not show fungi. In case of candida, it evidences nonspecific findings of keratosis, hyperplasia and large mononuclear infiltrate 6, 9. When we suspect of mycotic infections, the histopathological analysis should be made with periodic acid schiff or silver methionamine staining, which allows visualization of the whole fungal cell wall. However, it is difficult to differentiate the various types of fungi based on the morphology of the visualized hyphae, requiring in many situations the clinical history of the patient and culture analysis to confirm the diagnosis 1-9.
Oral and esophageal candidiasis are normally successfully treated with topical agents; however, as topical agents do not normally reach the larynx, infection by candida in this region normally requires administration of systemic anti-fungal agents, even in immunocompetent patients or in those that do not have associated systemic infection.
The traditional treatment for systemic mycosis is therapy with intravenous amphotericin B. Alba, Molina, Ortega and Várques3 reported in their experience that parenteral amphotericin B as anti-fungal agent is effective in managing laryngeal candidiasis, but they also stated that other agents could be successfully used. However, administration of amphotericin B is associated with many significant side effects, with confirmed renal, heart and liver toxicity. Conversely, other oral anti-fungal agents that are less toxic have demonstrated efficiency in many different laryngeal mycosis, as confirmed by Selkin9, Fletcher and Prussin10.
Many anti-fungal oral agents have been successfully employed in the therapy against mycosis, such as ketoconazole and fluconazole, and more recently, there have been successful reports of the use of itraconazole, including the treatment of histoplasmosis 10. Treatment of mycosis can be difficult and normally requires long-term therapy such as 4 to 6 weeks or even more in refractory cases before complete resolution of infection is achieved.
CASE REPORT
Male, 76-year-old patient, born in Sao Gonçalo/BA, came to the Service of Otorhinolaryngology, Hospital Otorrinos, with single complaint of marked odynophagia. He reported onset of symptoms about one month before and complained of progressive worsening of pain. He did not report any other symptoms. He had smoked for over 50 years, 3 to 10 cigarettes a day. The patient did not report any other symptoms suggestive of gastroesophageal reflux. He did not report medical treatment such as surgery or hospitalizations in the past 10 years, as well as use of antibiotics for treatment of any infectious process in the past six months or use of corticoids. He had good nutritional status, despite referring weight loss owing to odynophagia (he could not specify how much), and did not have diabetes or hypertension.
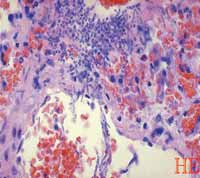
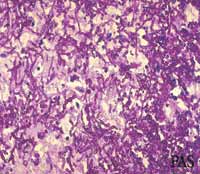
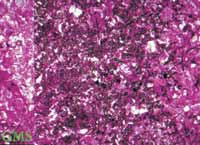
We conducted complete head and neck examination, as well as oral cavity inspection and did not find any significant clinical findings. There was no oral candidiasis. Indirect laryngoscopy revealed signs of epiglottitis with marked hyperemia. Next, we conducted direct videolaryngoscopy to better analyze the pathology and we observed deforming lesions in the epiglottis and involvement of the superior laryngeal region, which made us consider a neoplastic process, based on the age of patient and chronic smoking (Figure 1). We scheduled microlaryngoscopy under general anesthesia to biopsy the region. The material collected for hematoxylin-eosin staining showed hyperplasia with large acute inflammatory region and mononuclear infiltrate (Figure 4). A new biopsy was then scheduled with collection of material from more than one lesion site and the same nonspecific histopathological finding. Only when the slide was stained with Periodic acid schiff that the characteristics signs of candida hyphae were detected (Figure 5). A new slide from a different fragment was obtained in the last biopsy and it was also stained with periodic acid schiff and silver methionamine (GSM) confirming the presence of candida hyphae (Figure 6).
Chest x-ray did not show lung involvement. We also investigated immunodeficiency including viral etiology through serology analysis.
We started the therapeutic regimen with fluconazole 150mg/day. Treatment was maintained for a period of 3 weeks. The patient was instructed and stimulated to stop smoking, since it plays the role of predisposing agent by destroying the mucosa. Progression and clinical improvement were followed up by videolaryngoscopy. The regression of the laryngeal lesion was well documented (Figures 2 and 3) through imaging exams and showed complete regression at the end of treatment. During the 6-month follow-up we did not detect new episodes of the disease.
DISCUSSION
The first line defense of the body against infections is formed by barrier mechanisms represented by the skin or the mucous epithelium. The upper airway epithelium is, thus, a physical barrier that is supported by mucous recover and protects the organism against potential pathogens that can get established there. If there are mucosa surface lesions, there is activation of second line defense, represented by nonspecific response from the immune system.
Any alteration to the normal mechanism of defense of the organism favors development of infections. Thus, any factor that acts by causing changes to the mucosa barrier or depresses the immune response predisposes to infection by laryngeal candida. Forest and Weed listed these factors as shown in the charts below:CHART 1
Conditions associated with immune response affections
- Immunosuppressant drugs
o Corticoids
o Chemotherapy
- Immunodeficient syndromes
o Congenital
o Acquired
- Nutritional deficiency
- Diabetes
CHART 2
Conditions associated with mucosa barrier affections
- Antibiotic therapy with changes to local flora
- Inhalation corticoids
- Radiotherapy
- Smoking
- Local traumas
o Surgical
o Intubation
- Gastroesophageal reflux disease
- Chemical/thermal injury
The most frequent causal factor for laryngitis by candida is prolonged use of systemic antibiotics 8, owing to changes to the local flora that favor proliferation of the fungi. Thus, when we prescribe antibiotics, especially wide spectrum ones and associated with topical or systemic corticoids, the potential risk of laryngitis by candida should be considered. Isolated inhalation corticoids can also represent increased risk of development of oral, pharyngeal and laryngeal candidiasis.
In general, fungal laryngitis presents as ulceration of the mucosa, except in cases of superficial infection by candida in which the larynx presents only diffuse erythema of the areas with adherent white plaques. Candida represents part of the normal flora, being cultivated from the oral cavity in 7% of the population 11.
To treat fungal laryngitis we should use systemic anti-fungal agents, even though some authors consider initial treatment of immunocompetent patients with topical agents - such as nistatin, at least for three weeks before the use of systemic agents. It is obvious that topical agents have only local effect and are not absorbed after swallowing. To those that advocate this type of treatment, we question its real efficacy considering that there is no or little contact between the topical agent and the larynx, as previously reported. Thus, there are reports of successful applications of gentian violet to excise laryngeal lesions 4.
All patients with diagnosis of laryngeal candidiasis should necessarily be submitted to simple chest x-ray to rule out associated pulmonary involvement since there is a consensus that in cases of concomitant lung infection it is mandatory to use systemic anti-fungal agents in the treatment. In cases of immunocompromised patients, the therapy should necessarily be systemic, owing to the risks of dissemination of the infection from the laryngeal focus. In immunocompromised patients, we should consider the option of using amphotericin B as the agent of choice.
In the case reported here, we decided to start treatment with systemic therapy since it was an elderly patient, considering the grade of the laryngeal lesion upon diagnosis (simulating a neoplastic disease) and low incidence of adverse events caused by fluconazole in the dose used (150 mg/day), as reported by other studies 2, 9.
Fluconazole has low toxicity compared to other anti-fungal agents and only in severe or debilitated patients there are reports of liver toxicity, requiring monitoring of liver enzymes. There is good absorption that does not depend on gastrointestinal acid levels, differently from other oral agents. The use of fluconazole is recommended in doses of 100-400mg/day; we used 150mg/day since it is the presentation available in Brazil. Many other studies showed that most of the patients responded to an average dose of 100mg. As to mycotic laryngitis caused by other fungi, such as histoplasmosis or blastomycosis, the use of ketoconazole is recommended as the anti-fungal agent of choice at the same dose 10.
Another important factor that should be taken into account in the success of treatment is the fact that anti-mycotic agents only inhibit fungal growth; therefore, we should also treat or fight against the predisposing factors of the underlying diseases that could have contributed to the infection, otherwise there may be recurrence of the disease. Thus, we should try to strengthen the immune status of the patients, improving nutritional status or promoting better control of diabetes, for example. Aggression factors against the mucosa barrier should be strongly attacked, such as smoking, GERD and poor vocal hygiene.
CONCLUSION
We should bear in mind that mycotic laryngitis, especially candidiasis, may simulate many pathologies that occur together with local erythema, leukoplasia and ulceration of laryngeal mucosa; therefore, a certain level of suspicion should be considered in all cases to define the correct diagnosis. Laryngeal mycotic infection is not a common pathology, especially when isolated and in immunocompetent patients. Therefore, in order to come to the correct diagnosis, we should conduct good anamnesis and complete clinical examination of the head and neck, follow the logical reasoning lines and diagnostic investigation, which comprises all predisposing factors listed in the anamnesis to the immune status of the patient. The last diagnostic step is biopsy of the affected areas guided by direct laryngoscopy. The collected material should be specially stained for visualization of hyphae using Periodic acid schiff (or silver methionamine).
We should also emphasize the importance of attacking the predisposing factors as part of the treatment to prevent recurrence. In immunocompromised patients, we should use amphotericin B as the main agent, owing to the risk of systemic dissemination of the infection and because of the frequency of association with lung infection, associating oral agents such as ketoconazole or fluconazole 2,9. Even in immunocompetent patients, we recommend the use of systemic therapy together with the exclusion of aggressing factors to the mucosa, assessing the risk of possible complications and the low incidence of adverse effects on the recommended dose.
Finally, each case should be individually assessed according to severity of the disease and health status of the patient. However, in the case of mycotic laryngitis, we should always study the systemic infection or associated lung disease, as well as the immune status of the patient.
Figure 1. Epiglottis before treatment.
Figure 2. Epiglottis - 2 weeks after treatment.
Figure 3. Laryngeal aspect after treatment.
Figure 4. Staining - hematoxylin-eosin.
Figure 5. Periodic acid schiff.
Figure 6. Silver methionamine.
REFERENCES
1. Wang JN, Liu CC, Huang TZ, Huang SS, Wu JM. Laryngeal candidiasis in children. Scand J Infect Dis 1997; 29(4): 427-9.
2. Forrest LA, Weed H. Candida Laryngitis appearing as leukoplasia and GERD. J Voice 1998 Mar; 12(1):91-5.
3. Alba D, Perna C, Molina F, Ortega L, Várques JJ. Isolated Laryngeal Candidiasis: Description of 2 cases and review of the literature. Arch Broconeumol 1996 Apr; 32(4): 205-8.
4. Tedeschi LG, Cheren RV. Laryngeal Hyperkeratosis due to primary Monilia Infection. Arch Otolaryngol 1968; 87(1):100-2.
5. Yohkers AJ. Candidiasis of the Larynx. Ann Otol 1973;82: 812-15.
6. Tashjiam LS, Peacock JE. Laryngeal Candidiasis. Arch Otolaryngol 1984; 110(12):806-9.
7. Sataloff RT, Spiegel JR, Heuer RJ. Laryngeal sarcoidosis and candidiasis. Ear Nose Throat J 1995 Feb; 74(2):77.
8. Haberman RS, Becker ME, Ford CN. Candida Epiglottitis. Arch Otolaryngol 1983; 109(10):770-1.
9. Selkin SG. Laryngeal Candidiasis and Ketoconazole. Otolaryngol Head and Neck Surg 1985; 93(5):661-3.
10. Flecher SM, Prussim AJ. Histoplasmosis of the Larynx with Cetoconazol treatment: A case report. Otolaryngol Head and Neck Surg 1990; 103(105): 813-26.
11. Baum GL. The Significance of Candida Albicans in the Sputum. M Emg J Med 1960; 263:70-3.
1 Master studies in Otorhinolaryngology under course, Santa Casa de Misericórdia de Sao Paulo.
2 Resident Physician in Otorhinolaryngology, Hospital OTORRINOS.
3 Otorhinolaryngologist, Hospital OTORRINOS.
4 Resident physician in Otorhinolaryngology, Hospital OTORRINOS.
5 Resident Physician in Otorhinolaryngology, Hospital OTORRINOS
Study conducted at Hospital OTORRINOS - Doenças do ouvido, nariz, garganta e Cirurgia de Cabeça e Pescoço - Residence program in Otorhinolaryngology, Feira de Santana, BA.
Address correspondence to: Dr. Paulo Sérgio L. Perazzo - Rua Barão de Cotegipe, 1141 Centro, Feira de Santana BA 44025-030
Tel (55 75) 623-4455 Fax (55 75) 223-4117 - E-mail: otorrinos@uol.com.br