Year: 2004 Vol. 70 Ed. 2 - (19º)
Relato de Caso
Pages: 268 to 271
Schwannoma of the larynx: case report
Author(s):
Erich Christiano M. Melo 1,
Romualdo Suzano L. Tiago 2,
Osíris de Oliveira C. Brasil 3,
Soraia El Hassan 3,
Lupércio Luz Brito 4,
Paula Magalhães de Sá 4
Keywords: larynx, Schwannoma, neurinoma, dysphagia
Abstract:
Schwannomas are benign, slow-growing, encapsulated tumors, which appear on the sheath of sensitive or cranial motor nerves Schwann cells, and having no nervous elements. They rarely appear on the larynx, and there are sporadic reports in the literature. This work has as purpose to report a case of laryngeal schwannoma. A 82 years-old woman, born and residing in the city of Sao Paulo, SP, went to the Hospital, suffering from slowly progressive, long-term dysphagia for solids and globus sensation. The indirect laryngoscopy with a 70º rigid telescope revealed a submucous tumor, rounded, at the interarytenoid region. A neck computed tomography was made, revealing an apparently solid lesion, with no central necrosis and no extension to deeper levels, the greatest diameter of which was of 2.5 cm. The patient underwent a larynx microsurgery with tumor full removal. The histological analysis revealed a laryngeal schwannoma. The patient recovered well with no no signs of recurrence or residual tumor until now.
![]()
INTRODUCTION
Schwannomas are benign, slow growth, encapsulated tumors that arise from the sheath of Schwann cells of motor or sensitive cranial nerves, without nervous elements. About 65% of these tumors occur in the central nervous system, being most of them in the 8th cranial nerve 1. The incidence rate in the head and neck ranges from 25 to 37%, among other possible locations. The lateral region of the neck is the most common site, originating from the neck nervous roots and the cervical sympathetic chain 2. The laryngeal location is rare and there are few sporadic literature reports only 1, 3, 4. Laryngeal schwannoma amounts to about 0.1% of all benign laryngeal tumors 5. Most of the described cases are located in the aryepiglottic fold 6 and the therapy of choice is surgical approach. Malignant degeneration of these tumors is extremely rare 7.
The purpose of the present study was to report a case of laryngeal schwannoma in a location that has never been described in the literature, as well as to conduct literature review on the topic.
LITERATURE REVIEW
In a review of 722 cases of laryngeal benign tumors, New and Erich (1938)8 found only one case of schwannoma, whereas Holinger and Johnston (1942)9 found one case among 1,197 cases of laryngeal benign tumors.
It has been described in almost all age ranges and with slight predominance to female gender 10. Malignant schwannomas are very rare, especially in the larynx, being that the first case was reported in 1982 7.
The most frequent site (80%) of laryngeal schwannoma is aryepiglottic fold 6. Owing to that, it is inferred that the most common nervous origin is the internal ramus of superior laryngeal nerve, after the penetration into the thyrohyoid membrane 3. The origin from recurrent laryngeal nerve has also been described, which can lead to vocal fold paralysis 11, 12. However, the exact identification of the nervous origin is difficult to find, even intraoperatively.
The growth pattern is slow and laryngeal symptomatology is related to the mass effect caused by the tumor. The sensation of pharyngeal globus can be the first symptom, sometimes followed by dysphagia and dysphonia, when tumor size hinders vocal fold normal movement. If the tumor takes on exaggerated proportions, there may be respiratory discomfort characterized by inspiration stridor. In some cases, it may require conduction of tracheotomy to maintain permeability of the airways. Pain is rarely a significant symptom 11.
Diagnosis is based on videolaryngoscopy and imaging exams, especially computed tomography (CT). The macroscopic aspect is of a regular, smooth, pinkish and rounded or oval tumor, normally sessile, which can take a polypoid aspect. CT scan is very useful to determine the dimension and extension of the tumor mass 10.
The histologic diagnosis is based on cell pattern observed by optical microscopy. Cell and edematous regions are alternated in varied proportions and are named cell type Antoni A and Antoni B 4. Pattern Antoni A is more cellularized and presents structural organization in palisade. Pattern Antoni B is not characterized by any structural organization. Both types can be found in the same tumor. Immunohistochemistry can confirm the diagnosis showing reactivity to protein S-100.
As to treatment, it is a consensus that surgery is the first option. However, surgical approach is controversial and two options have been frequently reported: external classical approach and transoral approach (direct laryngoscopy) 4. The latter has the advantage of presenting low incidence of laryngeal complications, being indicated in smaller tumors. In larger tumors, external approach is normally preferred (lateral pharyngotomy or laryngofissure) 10, 13. Therapeutic approach should be planned according to site, extension and presentation of the lesion 4.
CASE REPORT
G.A., 82-year-old female subject, born in Sao Paulo-SP, came to the Service of Otorhinolaryngology, Hospital do Servidor Público Estadual, in July 2000, and referred dysphagia for solids for a long time, of slow progression, associated with globus pharyngeal, without dysphonia or dyspnea. She did not report smoking, alcohol abuse or associated dyspeptic symptoms.
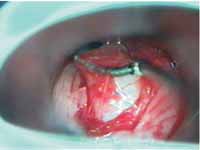
The physical ENT examination by indirect laryngoscopy showed submucous lesion in the interarytenoid region. We conducted videolaryngoscopy with rigid telescope 70o, which showed submucous rounded tumor on the interarytenoid region, with displacement of the mucosa that recovered the lesion during phonation (Figure 1). Vocal folds were normal in morphology and mobility. Both hypopharynx and the remaining portions of the larynx were normal. We conducted neck CT scan and it showed a lesion that was apparently solid, without central necrosis and no extension to deep plans, measuring approximately 2.5cm in the largest diameter. CT scan was very useful to determine dimension and extension of tumor mass.
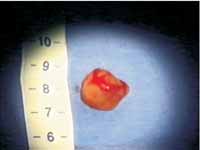
Patient was submitted to laryngeal microsurgery in August 2000, under general anesthesia. We conducted mucosa incision that recovered the lesion with displacement of the tumor and complete removal of the tumor (Figures 2 and 3). The excessive mucosa was conservatively removed. The excised material was sent to clinical pathology analysis and histology analysis revealed that it was laryngeal schwannoma.
The patient progressed well, no further complaint and normal phonation and swallowing. Early and late postoperative control videolaryngoscopy did not show signs of recurrence or residual tumor in the 2-year follow up (Figure 4).
DISCUSSION
Laryngeal schwannoma can affect any age range. In our study, the patient was aged 82 years. Plantet, Hagay, Maulmont et al, in a report of two cases, found one patient aged 30 and another one, 67 years 12.
The most frequent location is aryepiglottic fold 5. In our case, the tumor was located in the interarytenoid region, which had never been reported in the literature.
Fini-Storchi and Frosini (1997) reported that swallowing affections are the most characteristic symptoms 2. In our study, the patient presented foreign body sensation in the throat and dysphagia for solids.
As to surgical approach, we decided to go for transoral via as a result of presentation, location and extension of tumor. The external approach can be performed through lateral pharyngotomy 10 or laryngofissure 13.
Transoral approach is indicated in smaller tumors, and its advantage is smaller incidence of recurrent laryngeal nerve palsy after the surgery. However, complete exeresis of the tumor can be difficult 4.
Even though prognosis is good, there have been reports of recurrence; therefore, it is necessary to have prolonged follow-up 3. To present, we did not find signs of recurrence in the studied case.
CLOSING REMARKS
Laryngeal schwannoma is a benign, rare, slow growth tumor with symptoms associated with lesion mass effect. Our case was a patient whose main complaint was oropharyngeal dysphagia, which disappeared completely after surgical treatment. We decided to perform transoral approach using direct laryngoscopy, since it is more conservative and allows complete resection of the tumor. The patient has no signs of recurrence after two years of follow-up.
Figure 1 - Preoperative videolaryngoscopy.
Figure 2 - Laryngeal microsurgery, including submucous tumor dissection.
Figure 3 - Surgical piece, measuring about 2cm.
Figure 4 - Postoperative videolaryngoscopy (1st month).
REFERENCES
1. Palva T, Jokinem K, Karja J. Neurilemnoma (schwannoma) of the larynx. J Laryngol Otol 1975; 89:203-7.
2. Fini-Storchi I., Frosini P. Laryngeal neurinomas (a case report and review). ORL 1997; 59:182-5.
3. Phang WK, Raman R, Jayalaksmi E. Neurogenous tumour of the larynx (a case report). J Laryngol Otol 1987; 101:1209-10.
4. Takumida M, Taira T, Suzuki M, et al. Neurilemmoma of the larynx (a case report). J Laryngol Otol 1986; 100:847-50.
5. Barnes L, Ferlito A. Soft tissue neoplasms. In Ferlito A. Neoplasms of the larynx. Edinburgh, Churchill Livingstone, 1993; 277-9.
6. Supance JS, Quenelle DJ, Crissman J. Endolaryngeal neurofibromas. Otolaryngol Head Neck Surg 1980; 88:74-8.
7. Delozier HL. Intrinsic malignant schwannoma of the larynx: a case report. Ann Otol Rhinol Laryngol 1982; 91:336-8.
8. New GB, Erich JB. Benign tumors of the larynx: a study of 722 cases. Arch Otolaryngol 1938; 28:841-910.
9. Holinger PH, Johnston KC. Benign tumors of the larynx. Ann Otol Rhinol Laryngol 1951; 60:496-509.
10. Schaeffer BT., Som PM., Biller HF et al. Schwannoma of the larynx: review and computed tomographic scan analysis. Head Neck Surg 1986; 8: 469-72.
11. Jamal MN. Schwannoma of the larynx: case report and review of the literature. J Laryngol Otol 1994; 108:788-90.
12. Plantet MM, Hagay C, Maulmont C et al. Laryngeal schwannomas. Europ J Radiol 1995; 21:61-6.
13. Whittam DE, Morris TMO. Neurilemmoma of the larynx. J Laryngol Otol 1970; 84: 747-50.
1 - Collaborating physician, Division of Clinical Otorhinolaryngology, Hospital das Clínicas, Medical School, University of Sao Paulo. Former Resident Physician, Service of Otorhinolaryngology, Hospital do Servidor Público Estadual de Sao Paulo.
2 - Ph.D. studies under course, Post-Graduation in Otorhinolaryngology and Head and Neck Surgery, Federal University of Sao Paulo - Escola Paulista de Medicina. Assistant Physician, Service of Otorhinolaryngology, Hospital do Servidor Público Estadual de Sao Paulo.
3 - Ph.D. in Medicine, Federal University of Sao Paulo - Escola Paulista de Medicina. Assistant Physician, Service of Otorhinolaryngology, Hospital do Servidor Público Estadual de Sao Paulo.
4 - Resident Physician, Service of Otorhinolaryngology, Hospital do Servidor Público Estadual de Sao Paulo.
Affiliation: Hospital do Servidor Público Estadual - "Francisco Morato de Oliveira"-
Sao Paulo - SP
Address correspondence to: ERICH CHRISTIANO MADRUGA DE MELO. R. TTE GOMES RIBEIRO 30, APT 143, VL CLEMENTINO, SAO PAULO - SP. CEP: 04038-040
E-MAIIL: erichmelo@uol.com.br