Year: 2004 Vol. 70 Ed. 2 - (3º)
Artigo Original
Pages: 164 to 170
Surgical approaches to the paranasal sinuses osteoma
Author(s):
Fernando O. Balieiro 1,
André Bordash 1,
Aldo E. C. Stamm 2,
Bruno B. Sebusiani 3,
Iulo S. Baraúna Filho 3
Keywords: osteoma, paranasal sinuses, surgery.
Abstract:
Osteomas are the most common benign tumors arising in the paranasal sinuses, they are slow growing tumors and most part of them are assymptomatic. The surgical treatment is a controversial issue concerning their indications and surgical approach. There are several options for surgical approaches ranging from classical external surgery to intranasal endoscopic surgery. There are no formal indications for each approach and we must consider the tumor size when indicating the best approach. Aim: In this paper we will present six cases of paranasal osteomas operated at Hospital Edmundo Vasconcelos, São Paulo-SP, Brazil, with different approaches. We are also going to discuss the indications for the surgery and these approaches concerning the advantages and disadvantages of each procedure. Study design: Series review.
![]()
INTRODUCTION
Osteoma is the most common benign neoplastic disease of paranasal sinuses. 1. It is a slow-growth bone tumor which is typically an occasional finding in imaging tests requested for other reasons.2. In 1993, Earwaker (apud Hear and Jones)2 reviewed 1500 CT scans of facial sinuses and found 46 osteomas.
Osteoma are generally asymptomatic presenting unlimited growth and could be locally aggressive with compression and/or affect surrounding structures, primarily the orbital extension and skull base leading to severe complications such as eyeball diplopia and proptosis if the tumor affects the orbit, displacing it and compressing the optical nerve. It may have increased growth rate affecting CNS with cerebrospinal fluid fistula, cerebral abscess and even mucocele 3, 4, 5, 6, 7.
Symptoms of osteoma include headache and facial pain 2, 3, 4, followed by rhinorrhea, nasal obstruction, secondary sinusitis and, more rarely, epistaxis 2. It may also present anterior growth causing aesthetic deformity of the face. 1
It is more common in frontal sinuses accounting for approximately 57 to 75% of all paranasal sinuses osteomas 3, 4, followed by ethmoidal sinuses, maxilla and more rarely sphenoid sinuses 5. Its incidence is higher in the 3rd and 4th decades of life, but it can be found at any age being slightly predominant in males 1,5.
Histological findings are described in 3 distinct forms of osteoma: compact or eburneous in which few amount of fibrous tissue is found, spongy osteoma, with increased amount of fibrous trabeculae, and finally combined osteoma, which is a combination of the two previous types 3, 4, 8. Most osteomas are eburneous.
Three theories were postulated to explain the etiology of this tumor, but none has been proved yet. The first theory is the embryological theory stating that osteomas were originated from embryo debris present in embryological distinct bone joints (e.g. frontal bone of membranous calcification and ethmoidal bone of endochondral ossifying process) 1, 4, 8. However, this theory does not explain the origin of osteoma in other sites3. The second theory states that osteoma may have a post-traumatic origin 1, 3, 4, 8, but only 30% of patients have former record of trauma1. The last theory is the infection theory, in which osteomas were bone hypertrophy formed as a reaction to existing paranasal sinuses infections. This theory is also arguable because it is quite difficult to define cause-effect, since many cases of sinusitis may be an effect of the tumor itself3. The scientific literature data available present high variation regarding osteomas and infection 4.
The treatment of nasosinusal osteomas is still controversial in the scientific community. Some authors advocate expectant management if the patient is asymptomatic and surgical treatment if the patient has symptoms. Others believe that depending on the tumor location it should be treated with surgical approach due to potential complications aforementioned.
This paper will review scientific literature of the most common surgical approaches and major surgical management indications. Additionally, six surgery cases of Centro de Otorrinolaringologia e Fonoaudiologia de Sao Paulo/ Hospital Prof. Edmundo Vasconcelos will be presented as an attempt to correlate these cases with the scientific findings.
MATERIAL AND METHODS
This study will present six cases of surgery to remove tumors of different sizes and locations to exemplify different types of surgical access that may be used to manage these tumors. Patients were operated on through distinct approaches according to peculiarities of each case. The reasons that led us to operate the patients will also be pointed out.
In this series, 2 isolated ethmoid osteomas, 2 frontoethmoid osteomas, and 2 frontal osteomas were operated on. Ethmoid osteomas were removed through videoendoscopy-assisted endonasal route. Frontoethmoid osteomas were removed with different techniques - one with midfacial degloving and the other through external fronto-ethmoidectomy. Frontal sinus osteomas were resected, being one through coronal approach with osteoplastic flap and the other through videoendoscopy-assisted transnasal approach.
CLINICAL DATA
Case 1
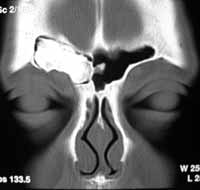
Male, 43 years old, with symptoms of left nasal obstruction and mild headache. Patient has undergone turbinectomy previously due to nasal obstruction performed in another care center. As symptoms did not improve, CT scan was performed and a large-sized osteoma completely occupying the left ethmoid sinus was detected (figure 1), respecting the orbital extension and skull base and displacing nasal septum to the contralateral side. The patient was referred to our service and underwent tumor resection through videoendoscopy-assisted transnasal approach. Semi-cutting drill was used to split the osteoma in the middle due to its excessive size. Its implantation, however, was located in a small region of the ethmoidal fovea and did not damage skull base after removal. Figure 2 shows fragments of the surgical specimen. The patient had good outcome and was discharged from hospital on the second day after the surgery. He had moderate bleeding on the 14th postoperative day due to a lesion to a left middle concha vessel.
Case 2
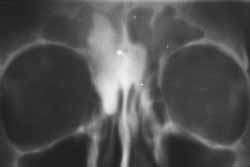
Female, 35 years old, complaints included headache and left nasal obstruction, paranasal sinuses CT showed septum deviation to the left and small-sized osteoma located in the left ethmoid sinus (figure 3). Patient has undergone septoplasty and osteoma resection through videoendoscopy-assisted transnasal approach; the surgery was eventfulness since the tumor had good cleavage plan and its insertion was detached simply by moving it. It was difficult to remove the tumor through the nostril due to its size; therefore, it had to be partially fragmented. The patient recovered well without postoperative complaints. Figure 4 displays postoperative follow-up CT scan.
Case 3
Female, 21 years old, with complaint of left eye proptosis without diplopia for more than 6 months. CT showed an osteoma of gigantic proportions occupying the entire left ethmoid sinus, with frontal sinus and orbital extension and affecting the anterior skull (figure 5). The tumor was approached through mid-facial access (Degloving) with broad ethmoidectomy and full tumor exposure. Since tumor implantation was extensive and strong, we used semi-cutting and diamond burs to properly define osteoma borders in relation to the orbit and skull base. During the removal of this tumor, the patient presented small cerebrospinal fluid fistula in the ethmoid fovea, which was promptly identified and corrected with fascia lata, muco-periosteum and fibrin glue. Patient recovered without postoperative complaints and the follow-up CT showed comprehensive resection of tumor, but there was a small limited residual tumor in the frontal sinus, which did not affect the nasal-frontal duct (Figure 6).
Case 4
Female, 31 years old, complaints of right moderate supra-orbital pain for three months. CT scan showed osteoma occupying the entire right frontal sinus with orbital implantation and extension (figure 7). The tumor was approached through bitemporal coronal incision with osteoplastic flap. After exposing the tumor, the implantation observed was located in a small area of the right orbit roof. The tumor was easily removed with no fracture of orbital roof. The patient had bipalpebral ecchymoses and mild subcutaneous emphysema of spontaneous regression, without any aesthetic change. Figure 8 shows the control tomography with complete resection of the tumor, clearly showing the points in which frontal sinus was opened.
Case 5
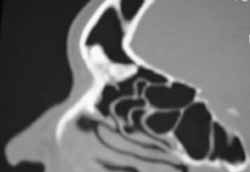
Male, 35 year old, with complaint of hemicranial headache. The CT scan showed left frontoethmoid osteoma completely occupying left ethmoid sinus and extending itself to the anterior base of the skull, but not affecting it (figure 9); no orbital extension was found although the tumor was implanted in the mid-orbital wall. Tumor was approached through external route, with front-ethmoidectomy being performed through Lynch incision. Surgery was eventfulness and tumor was completely removed. In this case, the tumor detached itself from its insertion only by using a small scope. Patient had good postoperative recovery with palpebral ecchymosis and edema.
Case 6
Female, 55 years old, with complaints of headache and recurrent sinusitis, mentioning that recently she had drainage of large amount of purulent discharge through left nasal cavity with improvement of headache symptoms. CT scan showed middle-sized osteoma originating from left frontal sinus and partially blocking nasal-frontal duct (figure 10). The patient was informed about the best surgical approach, but she formally refused to undergo any kind of procedure that could result in aesthetic changes, expressing that she would prefer the surgery to be performed transnasally. The procedure was carried out and partial tumor resection and total clearing of nasal-frontal duct were successful, with just part of the tumor that was inserted in the anterior portion of the frontal bone remaining. In this case, the use of a cutting bur associated with angled pen was key for the success of the surgery.
DISCUSSION
Surgical management of paranasal sinuses osteomas is still a controversial issue in the scientific literature 9, whether regarding its indication or the preferred approach.
In 1990 criteria to indicate surgery management of paranasal sinuses osteomas were reviewed by Savic and Djeric 10 and they suggested that all oteomas that exceeded the borders of frontal sinus and were near nasal-frontal recess with symptoms of concomitant infection and all cases of ethmoid osteomas regardless of size should be treated with surgery. In 1999 Mansour et al.7 also mentioned that all sphenoid sinus osteoma should be operated, since any tumor growth could compress optical nerve or internal carotid artery. In patients with single complaint of headache comprehensive investigation should be carried out with exclusion of all the other possibilities before indicating surgery, since there are patients that still had headache symptoms after the surgery and improved with migraine and/or tension headache treatment 2,10.
Following all such criteria, surgery was indicated to our patients. In cases 1 and 2, tumors were removed because they were ethmoid tumors and the growth was likely to extend to the orbit and skull base. In case 1, the tumor was already large and in contact with the skull base, but did not affect it. In case 3 patients already presented orbital extension with ocular proptosis and surgery was indicated in order to preserve visual integrity. In case 4 the patient showed tumor that exceeded the frontal sinus borders, even though only mildly. In case 5, surgery was indicated because it was an ethmoid tumor extended to frontal sinus.
In our opinion the success of surgical management is related to the ability to evaluate and choose the proper approach that allows us to totally remove the tumor and avoid potential intra-operative complications. The choice of an approach route should primarily take into account size, location and lesion extension 11, 12, however, whenever possible, we should also consider aesthetical deformities resulting from surgical procedures.
Conventionally, this tumor is treated with external incisions. The approach used for frontal osteoma is coronal incision with osteoplastic flap and supraciliary incision can be used for bald patients. To resect ethmoid tumors it is possible to use external front-ethmoidectomy with Lynch incision 4, 13. Depending on the extension of the tumor and mid-third of the face, it is possible to extend the original incision, following the lateral margin of the nose, performing a lateral rhinotomy 7. This could also be enlarged with an incision that passes by the inferior margin of the nose opening and by the upper lip filter (Weber-Fergusson) creating and extensive skin "flap" with broad exposure of the mid-third of the face.
Some authors suggest the use of cranial-facial approaches, since they believe that this is the only way to perform total resection of the tumor, without causing postoperative aesthetical deformities, primarily in cases of frontal osteomas inserted in the anterior wall. In cases of intracranial complications they believe that the direct view of brain tissue and meninges helps to protect these tissues and prevent postoperative complications1,14. This procedure was also suggested to treat forehead aesthetical deformities1, 11.
In our opinion, most of the cases of paranasal osteomas do not require cranial-facial approaches, morbidity of such procedures is high and it is not justified. As a result of current development of skull base transnasal surgeries, we can prevent most intra-cranial complications without performing craniotomy. However, we agree with Chang et al. 1 when they say it is difficult to treat frontal tumors implanted in the anterior wall without causing aesthetical deformities.
Recently, some descriptions were found in the literature related to videoendoscopy-assisted transnasal approach to remove this kind of tumor 4.
To choose videoendoscopy-assisted transnasal approach it is key to be able to view all tumor borders 15 and, therefore, we agree with Schick et al.15 when they say that tumors exclusively confined to the ethmoid sinus could be removed endoscopically, as demonstrated in cases 1 and 2. Safe use of this access during tumor removal will essentially depend on the use of semi-cutting and diamond burs, particularly if the tumor does not easily detach from its insertion. The advantages of transnasal resection of ethmoid osteomas are the fact that patients are not exposed to increased morbidity and the likely aesthetical deformities of open procedures such as Lynch external ethmoidectomy, required in such cases4.
Once again, it is important to highlight that proper preoperative evaluation is crucial for surgical success, since it is of no use to prevent aesthetical lesions without being able to completely remove the tumor. Thus, in case 5, although the patient had ethmoid osteoma (indication of transnasal surgery) it was a large-sized tumor with frontal extension. We preferred external ethmoidectomy and succeed. If we had chosen to perform transnasal surgery, the opposite of what had just been described above would have happened, in other words, transnasal surgery would have, in this case, increased morbidity due to the extension and size of the tumor.
Another advantage that videoendoscopy-assisted transnasal approach has is that it can easily identify and treat spinal fluid fistulas. Duraplasty may be safely performed with the support of surgical microscope, as required in case 3.
We believe that ethmoid osteomas could be exclusively treated through transnasal approach. These patients should be carefully screened and should meet the following criteria: tumors should be exclusively confined to ethmoid sinus and should be small, once they have to be taken out through the nostril. Some larger tumors could be removed initially through transnasal access (case 1); in such case, the use of drills to fragment the tumor is essential. It is also very important for the team to be prepared to switch to external surgery whenever required.
Schick et al.15 reported that through videoendoscopy- assisted transnasal access it is possible to performed resection of frontal osteomas creating a Draf Type II or III (removal of high portion of nose septum and floor of frontal sinus). We believe that in such cases morbidity of external procedure (coronal incision with osteoplastic flap) is lower than of transnasal access because of the challenge that transnasal surgery of frontal sinus still represents. External surgery seems to be an excellent choice for exclusively frontal osteomas, especially with lateral implantation, allowing broad view and total resection of the tumor with minimal complications and deformities, as exemplified in case 4 of our case studies. Recently we had the opportunity to successfully operate on a tumor that occupied nasal-frontal duct (case 6) through transnasal access. Therefore, we believe that depending on the expertise of the surgeon and the availability of proper materials, it is possible to perform total resection of frontal tumors through transnasal access with low morbidity, provided that some principles are followed, such as sparing of duct mucosa. Thus, in such cases, we do not think it is required to create Draf II our III drainages.
Reports of cases operated through mid-facial access (degloving) were not found in the literature; however, in our opinion, this is an excellent option, once it enables broad exposure of surgical field with perfect view of the mid-third of the face, an approach that allows total resection of large-sized tumors, such as in case 3. Degloving still has an advantage over external ethmoidectomy, since it allows similar exposure but with enhanced surgical field to pass to surgical piece, without requiring external incision because it is performed through sublabial incision.
CLOSING REMARKS
Surgical treatment of nasosinusal osteoma is still a topic of discussion in the medical literature, especially regarding its indications. In our opinion, symptomatic tumors and those located in regions that are likely to result in severe complications or aesthetical deformities should be surgically managed.
There are several options of surgical approaches to treat paranasal sinuses osteomas and all of them have their own characteristics. And ideal approach does not exist and the size and location of the tumors are the main factors that should be taken into account. Videoendoscopy-assisted surgery has been proven to be an excellent option to treat small ethmoid osteomas, and conventional external surgeries are still the best option to treat larger tumors. However, as a result of enhanced familiarity with surgical anatomy and improved skills in handling new instruments, we think there is a possibility of major development in transnasal procedures to treat this and other types of tumors.FIGURE 1: Paranasal sinuses CT scan showing left ethmoid osteoma.
FIGURE 2: Surgical piece of ethmoid osteoma.
FIGURE 3: Paranasal sinuses CT scan showing left ethmoid osteoma.
FIGURE 4: Paranasal sinuses CT scan showing postoperative transnasal resection of paranasal sinuses osteoma.
FIGURE 5: Paranasal sinuses CT scan with 3-D reconstruction showing frontoethmoid osteoma.
FIGURE 6: Postoperative CT scan appearance of frontoethmoid osteoma.
FIGURE 7: Paranasal sinuses CT scan with frontal osteoma.
FIGURE 8: Postoperative appearance of frontal osteoma resection.
FIGURE 9: Paranasal sinuses x ray with frontoethmoid osteoma.
FIGURE 10: Paranasal sinuses cross-sectional CT scan showing frontal osteoma with occlusion of nasal-frontal duct.
REFERENCES:
1-Chang SC, Cheng PK, Chen YR, Chang CN; Treatment of frontal sinus osteoma using a craniofacial approach. Ann Plast Surg 1997; 38(5): 455-459.
2-Hehar SS, Jones NS; Frontoethmoid osteoma: the place of surgery. J Laryngol and Otol 1997; 111(4): 372-375.
3-Fobe LP, Melo EC, Cannone LF, Fobe JL; Cirurgia de osteoma de seio frontal. Arq Neuropsiquiatr 2002; 60(1): 101-105.
4-Brodish BN, Morgan CE, Sillers MJ; Endoscopic resection of fibro-osseus lesions of the paranasal sinuses. Am J Rhinol 1999; 13(2):111-116.
5-Summers LE, Mascott CR, Tompkins JR, Richardson DE; Frontal sinus osteoma associated with cerebral abscess formation: a case report. Surg Neurol 2001; 55:235-239.
6-Nakajima Y et al; A giant intracranial mucocele associated with an orbitethmoidal osteoma. J Neurosurg 2000; 92: 697-701.
7-Mansour AM, Salti HS, Uwaydat S, Dakroub R, Bashshour AZ; Ethmoid Sinus Osteoma Presenting as Epiphora and Orbital Cellulitis: Case Report and Literature Review. Surv Ophthalmol 1999, 43(5): 413-426.
8-Stamm AC, Watashi CH, Malheiros PF, Harker LA, Pignatari SSN; Micro-Endoscopic surgery of benign sino-nasal tumors; In: Stamm AC, Draf W; Micro-endoscopic surgery of the paranasal sinuses and skull base, Springer-Verlag Berlin Heidelberg 2000: 489-514
9-Huang HM, Liu CM, Lin KN, Chen HT; Giant ethmoid osteoma with orbital extension, a nasoendoscopic approach using a intranasal drill. Laryngoscope 2001; 111: 430-432.
10-Savic DLJ, Djeric DR; Indications for the surgical treatment of osteomas of the frontal and ethmoid sinuses. Clin Otolaryngol 1990, 15: 397-404.
11-Ciappetta P, Delfini R, Iannetti G, Salvati M, Raco A; Surgical strategies in the treatment of symptomatic osteomas of the orbital walls. Neurosurgery 1992; 31(4): 628-635.
12-Koivunen P, Lopponen H, Fors AP, Jokinen K, The growth rate of osteomas of the paranasal sinuses. Clin Otolaryngol 1997, 22: 111-114.
13-Al-sebeih K, Desrosiers M; Bifrontal endoscopic resection of frontal sinus osteoma. Laryngoscope 1998; 108(2):295-298.
14-Blitzer A, Kalmon D, Conley J; Craniofacial resection of ossifying fibromas and osteomas of the sinuses. Arch Otolaryngol Head Neck Surg 1989; 115: 1112-1115.
15-Schick B, Steigerwald C, Tahan AERE, Draf W; The role of endonasal surgery in the management of frontoethmoidal osteomas. Rhinology 2001; 39:66-69.
(1) Assistant Physician of Otorhinolaryngology and Speech Therapy; Centro de Otorrinolaringologia e Fonoaudiologia de Sao Paulo/ Hospital Professor Edmundo Vasconcelos.
(2) Head of Otorhinolaryngology and Speech Therapy; Centro de Otorrinolaringologia e Fonoaudiologia de Sao Paulo/ Hospital Professor Edmundo Vasconcelos.
(3) Internist of Otorhinolaryngology and Speech Therapy; Centro de Otorrinolaringologia e Fonoaudiologia de Sao Paulo/ Hospital Professor Edmundo Vasconcelos.
AFFILIATION: Hospital Professor Edmundo Vasconcelos.
ADDRESS CORRESPONDENCE TO: Rua Borges Lagoa 1450, Vila Clementino, Sao Paulo - SP, CEP 04038-905.
Tel (55 11) 5080-4357 Fax: (55 11) 5080 4097
E-mail: centrodeorl@osite.com.br
Study presented at 36th Brazilian Congress of Otorhinolaryngology, Florianópolis - SC, Brazil, November 2002.