Year: 2003 Vol. 69 Ed. 3 - (18º)
Relato de Caso
Pages: 415 to 419
Acute sphenoid rhinosinusitis and third cranial nerve involvement: case report and review of the literature
Author(s):
Francini G. M. Pádua 1,
Marcus Lessa 2,
Sandra M.Peres 1,
Elder Goto 2,
Richard L.Voegels 3,
Ossamu Botugan 4
Keywords: acute rhinossinusitis, sphenoid sinus, complications, oculomotor nerve, functional endoscopic sinus surgery
Abstract:
Cavernous sinus is located adjacent to sphenoidal sinus and presents close relationship with internal carotid artery and some important nerves (abducent, troclear, oculomotor and ophthalmic branch of the trigemic nerve). Since the sphenoid lateral wall is too thin, adjacent structure involvement is more frequent and dangerous when this sinus is disease. The purpose of this study is to report a case of an acute rhinosinusitis complicated with the involvement of the third cranial nerve. A 53-year-old woman was complaining about frontal headache one month before hospital admission. An acute sphenoiditis associated with exclusive involvement of oculomotor nerve was diagnosed. She received intravenous antibiotics and underwent Functional Endoscopic Sinus Surgery (FESS) with total recovering of the signs and symptoms. Sphenoiditis misdiagnosis or delay in the treatment of this condition may increase the risk of neurological complications. The initial clinical suspicion is important to start a specific treatment improving the outcome of these patients. In our experience FESS is a safe and efficient surgical approach for the treatment of acute rhinosinusitis complications.
![]()
Introduction
Rhinosinusitis can be classified as acute, subacute and chronic, according to duration of up to 4 weeks, between 4 and 12 weeks, or over 12 weeks, respectively 1. Ethmoid and sphenoid rhinosinusitis cases are those that present the greatest risk for orbital complications 2, whereas affection of the sphenoid sinus increases the incidence of complications of the nervous system 3.
Among orbital complications of acute rhinosinusitis, there are 5 clinical pictures according to the classification by Chandler4 (1970): periorbital cellulitis, orbital cellulitis, subperiosteal abscess, orbital abscess and cavernous sinus thrombosis. The cavernous sinus is adjacent to the sphenoid sinus and presents a close relation with the internal carotid artery and the abducent nerve, being that, close to its lateral wall, it is crossed by the trochlear and oculomotor nerves and the ophthalmic branch of the trigeminal nerve 5-8. Since the sphenoid wall is very thin, the involvement of adjacent structures is more frequent and dangerous when the sinus is affected. In a study conducted by Lawson9, 7.5% of the patients with isolated disease of the sphenoid sinus presented affections that corresponded to the 3rd nerve involvement, that is, the oculomotor nerve. Sawaya10, in 2000, described the first case of trigeminal neuralgia associated with sphenoid sinusitis, whereas in 1999, Chotmongkol11 described the first case of oculomotor paralysis secondary to acute sphenoid sinusitis.
In children, the affection of posterior ethmoid and sphenoid sinuses is uncommon 12. The affection of the 3rd nerve should suggest trauma, post-viral neuropathy, increase in intracranial pressure, meningitis and neoplasm 13.
The authors reported a case of complicated acute rhinosinusitis with isolated affection of the 3rd nerve, seen by the Division of Clinical Otorhinolaryngology, Hospital das Clínicas, Medical School, University of São Paulo. They present literature review and discuss the complications related to sphenoid sinus affection, its diagnosis and treatment.
CASE REPORT
Female patient aged 53 years, hypertensive taking enalapril and hydrochlorotiazide, with history of untreated chronic rhinosinusitis. One month before, she developed continuous frontal headache that waked her up during the night and improved partially with analgesics. It was followed by nasal obstruction, worse on the left, purulent rhinorrhea and 37.8o C fever. Five days before hospitalization she presented left palpebral ptosis associated with diplopia.
She was initially assessed by the neurosurgery department, considering the hypothesis of intracranial impairment, which ordered a head CT scan. It showed normal presentation, as well as the CSF analysis. In order to rule out cerebral aneurysm, angioresonance was requested (Figure 1), evidencing pervious Willis polygon, which ruled it out.
An ENT assessment was ordered and the following observed in the physical examination: polypoid mass on the left nasal fossa, absence of purulent secretion; oroscopy within normal range; palpebral ptosis on the left associated with mydriasis and ocular motility affections, with left diverging strabismus.
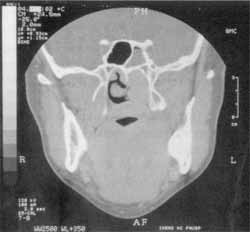
A paranasal sinuses CT scan was performed (Figures 2 and 3) which evidenced velamentum of frontal, sphenoid and maxillary sinuses and anterior ethmoid cells on the right; obliteration of the left nasal fossa and ostiomeatal complex; and air-liquid level on the right maxillary sinus.
Magnetic resonance imaging (MRI) (Figure 4) evidenced greater contrast in the small area of the left cavernous sinus.
She was hospitalized and intravenous antibiotics were administered (maximum dose crystalline penicillin and metronidazole), the patient was submitted to maxillary sinus punch and the purulent secretion was sent to culture and later diagnosed the growth of Streptococcus viridans and Peptostreptococcus micros (anaerobe), sensitive to the administered antimicrobial agents.
A functional endoscopic sinus surgery was performed on the left and it was uneventful, with approach of the anterior and posterior ethmoid, sphenoid, frontal and maxillary sinuses. There was no purulent secretion during the surgical act, only edematous mucosa. The patient was discharged on the 7th postoperative day taking oral antibiotic (clindamycin) for two weeks, presented good evolution and total regression of the clinical picture. Currently, she is followed up as an outpatient and has no complaints.
Figure 1. Angioresonance demonstrating pervious Willis polygon.
Figure 2. Paranasal sinuses computed tomography, axial section, showing velamentum of ethmoid and sphenoid sinuses.
Figure 3. Paranasal sinuses computed tomography, coronal section, showing velamentum of left sphenoid sinus.
Figure 4. Magnetic resonance imaging, coronal section, showing mild enhancement of left cavernous sinus.
Discussion
The term sinusitis refers to the inflammation of the paranasal sinuses mucosa, regardless of the etiology. Once sinusitis is invariably followed by nasal mucosa inflammation, rhinosinusitis is the most appropriate term 1.
Most of the cases of rhinosinusitis involve more than one sinus, more commonly the maxillary and ethmoid sinuses, being rare and dangerous to have isolated involvement of the frontal and sphenoid sinuses 1, 3. Ethmoid and sphenoid rhinosinusitis cases have more risks of orbital complications 2. Infectious diseases of the sphenoid sinus normally occur together with the other sinuses and presents risk of infection to the central nervous system, especially in diabetic, debilitated and immunocompromised subjects 3, 5.
There are 13 important structures adjacent to the sphenoid sinuses: dura mater, pituitary gland, optical chiasm, cavernous sinus, internal carotid artery, oculomotor nerve (3rd nerve), trochlear nerve (4th nerve), abducent nerve (6th nerve), ophthalmic division (V1) and maxillary division (V2) of the trigeminal nerve (5th nerve), sphenopalatine ganglion, vidian nerve and pterygoid canal 5, 6, 8. Since the nasal mucosa invaginates in the fetus, some of the listed structures may not be separated from the sinus by bone tissue, but rather by a thin layer of mucosa 6, 8. Fuji et al.5, in a study with cadavers, showed that 78% of them presented less than 0.5 mm of bone between the sphenoid sinus and the optical nerve and 8% presented bone dehiscence between the internal carotid artery and the sphenoid. Thus, owing to its proximity with the cortical venous system, cranial nerves and meninges, sphenoid sinus infections can reach such structures, imitating other neurological diseases and leading to serious complications 6, 8.
The main symptom related to affection of the sphenoid is headache, present in 70 to 90% of the cases. Normally of long duration and variable location, it may present a retro-orbital, frontal, parietal-occipital or vertex position, being refractory to medication treatment 3, 6, 9. In the case reported here, the patient had frontal headache for one month, with partial improvement after the use of analgesics.
Secondly, visual disorders such as vision blurring and loss of visual acuity may vary from mild to total. The optical nerve is the cranial nerve that is most frequently affected in sphenoid sinus infections. Lawson9 (1997) obtained 12% of ocular affection in inflammatory lesions, 60% in benign tumors and 50% in malignant tumors. Visual alterations are attributed probably to optical neuritis 12.
The cranial nerve most frequently affected second to the optical nerve is the 6th nerve (abducent nerve), being diplopia the main complaint. Its affection is attributed to its long pathways, in addition to its intracavernous medial position, closer to the lateral wall of the sphenoid sinus 5, 9. Lawson8 found 6% of involvement in inflammatory cases and 50% in neoplasm. Lana-Peixoto7, in 1992, reported a case of isolated unilateral paralysis of the abducent nerve caused by sphenoid sinus aspergillosis, which was initially attributed to the patient's diabetes, emphasizing the importance of the differential diagnosis by imaging methods.
The affection of the 5th nerve can occur by involving its first (V1) and second (V2) divisions, producing retrobulbar pain and pain or paresthesia of the midfacial region 9. Generally speaking, the etiology of the trigeminal neuralgia varies considerably. In about 90% of the times, the cause is unknown, and in 2% of the cases the etiology can be defined, being most of them secondary to the obstruction of a vessel, normally the upper cerebellar artery, over the emergence of the trigeminal nerve 10. Sawaya10 described the first case of sphenoiditis with trigeminal neuralgia symptoms, which normally occurs with maxillary rhinosinusitis.
The oculomotor nerve, the 3rd pair, is the fourth most affected nerve 9. It is a motor nerve that penetrates the orbit through the superior orbital fissure, distributing itself to the extrinsic muscles of the ocular bulb, to wit: upper lid elevator muscle, superior rectus muscle, inferior rectus muscle, medial rectus muscle, and inferior oblique muscle. The lateral rectus muscle is innervated by the abducent nerve, whereas the superior oblique muscle is innervated by the trochlear nerve. In addition to these muscles, the 3rd pair has fibers responsible for pre-ganglionar innervation of the intrinsic muscles of the ocular bulb: the ciliary muscle regulates the convergence of the lens, and the pupilary muscle 7. The nerve divides into superior and inferior portions on the most anterior region of the cavernous sinus. Therefore, divisional paresis is classically located on the anterior portion of the cavernous sinus or on the posterior orbital region. The isolated affection of the superior portion, involving the lid elevator muscle and the superior rectus muscle leads to ptosis and ocular motility compromise by paresis, or even to superior rectus muscle paralysis, which is relatively uncommon. In the case described here, the patient presented complete and isolated impairment of the oculomotor nerve presenting ptosis, mydriasis and diverging strabismus on the left., indicating an affection of the nerve before its division on the most anterior region of the cavernous sinus.
According to Lawson9, 7.5% of the patients with isolated disease of the sphenoid sinus present alterations corresponding to 3rd pair affections. Out of these, 1 patient presented mucoceles, 3 had benign tumors and 6 had malignant lesions. In his whole study, he observed neurological affection in decreasing order of the optical nerve, followed by the 6th, 5th and 3rd cranial nerves, being 12% of inflammatory origin, 60% of benign tumor origin and 40% of malignant tumors. Conversely, Lew6 observed that the most frequent neurological affection was hypoesthesia and hyperesthesia of the ophthalmic or maxillary dermatomes of the 5th cranial nerve.
In children, the posterior ethmoid and sphenoid sinuses affections is rare and different from that in adults, normally presenting with neck rigidity 9, 12. Since symptoms are generally non-specific, normally the diagnosis is delayed, suggesting other neurological diseases 12.
Acquire 3rd cranial nerve paralysis had as differential diagnosis: aneurysm, ischemic pain, trauma, post-viral neuropathy, intracranial pressure increase, meningitis and neoplasm, being all associated with headache 11, 13. The aneurysm may be compressing the pathways of the nerve, being the internal carotid artery or even the basilary apex. The involvement of the pupil occurs almost universally in children. In two large series, the involvement of the pupil was seen in 64% of the adults and in 90% of the children. Out of the total, 41% of the adults and only 7% of the children presented aneurysms 13. When pupil affection is followed by extrinsic ocular impairment, the presence of an aneurysm as causal factor becomes improbable 13. The reported patient presented complete affection of the 3rd nerve, which reduced the likelihood of an aneurysm, which was definitely ruled out after the conduction of an angioresonance. Sphenoid sinus aspergillosis has also been described associated with cavernous sinus thrombosis, as well as painful ophthalmoplegia of the oculomotor nerve paralysis 3. The involvement of the cranial nerves that are not the 2nd, 3rd, 5th and 6th nerves are a sign of neoplastic disease of the sphenoid 9.
The diagnosis of rhinosinusitis complications is made based on the clinical history, physical examination and imaging methods, which make it possible to have great diagnostic information and guide treatment 9. Sphenoid sinus infection is frequently diagnosed after the initial assessment 6. Located deeply in the apex of the nasal cavity, this sinus is not directly accessed by the physical examination and frequently it is not well visualized by routine conventional radiological exam (paranasal sinuses x-rays)6.
CT scan is considered the gold standard in the diagnosis of orbital complications of rhinosinusitis and in assessing the sphenoid disease, normally showing hypoattenuation material or thickening of the sinuses, bone involvement or not, which are images that suggest abscess and compromise or not of the orbital cavity structures 3, 6, 9. In the case of aspergillosis, it can be visualized as a calcium image suggesting fungal infection 3. Lew6 detected there was no correlation between the extension of opacification or bone sclerosis and severity of complications.
MRI is an essential complement in assessing the suspicion of cavernous sinus or vascular and adjacent nervous structures impairment. Angioresonance is indicated in cases in which there is suspicion of aneurysm or compression of the cranial nerves 13, as ruled out by the initial neurological assessment of the patient reported here.
The failure to perform an accurate diagnosis and treatment of sphenoid sinusitis may lead to severe neurological sequelae 5, 6. Therefore, early and aggressive treatment is crucial to prevent fatal complications 6. Intravenous antibiotic therapy may be initiated if there is isolation of the specific microorganism, high doses of penicillinase-resistant penicillin are indicated since the sphenoid impairment increases the likelihood of having Staphylococcus aureus, whose behavior is even more aggressive 5, 6. In the case reported here, the culture of maxillary sinus secretion detected the presence of Streptococcus viridans and Peptostreptococcus micros (anaerobe).
If symptoms persist or neurological signs are detected despite treatment, surgical drainage is indicated 6, 11.
In the literature review conducted by Hnatuk5, there are 5 different surgical techniques being transnasal sphenoidectomy the most frequent one. The same author observed that in cases in which there is no surgical approach, prognosis is clearly worse. Our patient was submitted to functional endoscopic sinus surgery on the left, uneventful, with approach of the anterior and posterior ethmoid, sphenoid, maxillary and frontal sinuses. She progressed well after the surgery and restored completely the oculomotor nerve function and was released from hospital on the 7th postoperative day taking oral antibiotics for two more weeks. She is currently being followed up in the outpatient unit and has had no complaints.
Conclusion
The failure to perform accurate diagnosis and treatment of sphenoid sinusitis may lead to severe neurological sequelae, therefore, early and aggressive treatment is crucial to prevent fatal complications and even death. In our experience, functional endoscopic sinus surgery has proven to be a safe and effective approach to manage acute rhinosinusitis complications.
References
1. Hickner JM et al. Principles of Appropriate Antibiotic Use for Acute Rhinosinusitis in adults: Background. Annals of Emergengy medicine jun 2001;37(6):703-10.
2. Botugan O, Balbani APS, Voegels RL. Classificação das Complicações Orbitais das Rinossinusites. Revista Brasileira de Otorrinolaringologia julho/agosto 2001; parte 1 67(4):551-5.
3. Lana-Peixoto MIV, Lana-Peixoto MA. Aspergilose invasiva do seio esfenoidal e paralisia do sexto nervo. Arq Neuro-Psiquiat 1992;50(1):110-5.
4. Chandler JR, Langenbrunner DJ, Stevens ER. The pathogenesis of orbital complications in acute sinusitis. Laringoscope 1970;80:1414-28.
5. Hnatuk LAP, Macdonald RE, Papsin BC. Isolated Sphenoid Sinusitis: The Toronto Hospital for Sick Children Experience and Review of the Literature. The Journal of Otolaryngology 1994;23(1):36-41.
6. Lew D et al. Sphenoid Sinusitis - A Review of 30 Cases. New England Journal of Medicine nov 1983;10:1149-54.
7. Machado ABM. Neuroanatomia Funcional. Rio de Janeiro, São Paulo: Livraria Atheneu Editora; 1991. p. 59-98.
8. Nelson DA et al. Neurological syndromes produced by sphenoid sinus abscess - with neuroradiologic review of pituitary abscess. Neurology oct 1967;17:981-7.
9. Lawson W, Reino A. Isolated Sphenoid Sinus Disease: An Analysis of 132 Cases. Laringoscope dec 1997;107:1590-5.
10. Sawaya RA. Trigemial Neuralgia Associated with Sinusitis. ORL 2000;62:160-3.
11. Chotmongkol V, Chainunsamit S. Superior Branch Palsy of the Oculomotor Nerve Caused by Acute Sphenoid Sinusitis. J Med Assoc Thai april 1999;82(4):410-2.
12. Bitsori M et al. Neurological manifestations of deep sinus infection. Acta Paediatr 2000;89:490-1.
13. Yang YC, Laws DE, Chandna A. The rules of third nerve palsy in children. Eye 1997;10(Pt 5):761-2.
1 Resident, Division of Clinical Otorhinolaryngology, Hospital das Clínicas, Medical School, University of São Paulo.
2 Post-graduate studies under course, Discipline of Otorhinolaryngology, Medical School, University of São Paulo.
3 Ph.D., Professor of the Discipline of Otorhinolaryngology, Medical School, University of São Paulo.
4 Associate Professor, Discipline of Otorhinolaryngology, Medical School, University of São Paulo.
Study conducted at the Discipline of Otorhinolaryngology, Medical School, University of São Paulo.
Address correspondence to: Francini Grecco de Melo Pádua - Rua Pará, 270 ap. 111
Higienópolis 01243-020 São Paulo SP
Tel (55 11) 3661-9332 / 9136-7016 - E-mail: fpadua@uol.com.br
Study presented at 2º Congresso de Otorrinolaringologia da Universidade de São Paulo, Nov/2001.
Article submitted on June 18, 2002. Article accepted on December 20, 2002.