Year: 2001 Vol. 67 Ed. 4 - (11º)
Artigos Originais
Pages: 519 to 525
The Use of Autologous Grafts of the Nasal Mucosa and inferior Turbinate Bone to Correct the Nasal Dorsum in Rhinoplasties Experimental Study in Rats.
Author(s):
Celina S. B. Pereira*,
José E. L. Dolci**,
Daniel E. L. Destailleur***,
Carmem L. P. Lancelotti****.
Keywords: mucosa, conchal bone, nasal turbinate, graft, rhinoplasty
Abstract:
Introduction: Many materials have been used as grafts to correct the nasal dorsum in rhinoplasties. The literature prefers autologous grafts due to high rates of extrusion, rejection, reabsorption and infection reported for other grafts. Study design: Experimental. Aim: The objective of the present study was to report the results of an experimental study with rats where mucosa was implanted under the skin. Such an experiment had not been reported in the literature to date. This paper also reports a number of patients that were grafted with mucosa removed from the own patients nasal cavity (inferior turbinate and/or conchal bone) who presented good aesthetic and functional results after three years and five months maximum follow-up period. The procedure has also decreased operative time. Material and method: Twelve wistar rats were submitted to biopsy of the nasal mucosa under sedation, and the specimen was implanted under the skin of the rat's scalp. The animals were sacrificed after four months and the area of the implanted mucosa was removed and histologically studied. Results: Healing occurred in a regular fashion with restitutio ad integrum. No signs of the mucosa were found between the skin and the muscle layer. Discussion: It seems that the mucosa served as an interface for uniform healing process, avoiding retractions where there were irregularities of the nasal dorsum.
![]()
INTRODUCTION
The use of grafts in rhinoplasty is a widely adopted procedure to correct esthetically and functionally noses that have lost substance due to trauma, chronic infection or iatrogenic problems resulting from previous surgeries. However, the choice of graft is still under debate, because the grafted material is easily absorbed in the postoperative period. There are different kinds of grafts described in the literature that may be subdivided into autologous, homologous, heterologous and alloplastic. Homologous grafts are those collected from cadavers or tissue banks (material collected from other subjects during functional surgeries). Among them, we may list fragments of cartilage or bone, which are normally irradiated to prevent contamination or infection4,14, in addition to reducing its antigenic capability. However, there are high rates of reabsorption as a result of the use of these grafts, as described by different authors. Heterologous grafts are obtained from other species than the human. The use of bovine cartilage processed in glutaraldehyde and then irradiated3 has been described, but the issue of postoperative reabsorption is still present. Alloplastic materials, such as silicone, mersilene, surgicel11, polyethylene, Teflon and carbon10, among others, are also used in nasal surgeries. The problem concerning this kind of graft is the likelihood of extrusion of the material and reaction to foreign body, as well as infections16. Therefore, autologous grafts (removed from the subject) are the most recommended ones for correction of nasal irregularities. Among the most frequent ones, we may list coastal, concha2,6,8 and nasal septum5,7,9 cartilage, bones (calvaria, ethmoid, vomer, iliac crest), fascia temporaliss.6,8 subcutaneous tissue existing between the inferior and superior lateral cartilages13, or galea. The three latter ones are used to correct minor irregularities of the nasal dorsum, after the placement of some other kind of graft.
The purpose of the present study was to show the use of another autologous material that had not been described yet; it is easy to handle and harvest and it is collected from the nasal fossa12.
MATERIAL AND METHOD
We selected 12 wistar rats and submitted them to nasal mucosa biopsy under microscopy and after sedation. From the removed fragments, we separated the mucosa from the submucosa in order to remove the abundant glands present in the tissue. The mucosa was implanted through a small incision made with conventional surgical knife, in the same surgical time, under the skin of the animal and between the two ears, since it was a difficult region for the rats to manipulate the wound with either frontal or hind paws. The incision was sutured with mononylon 4-0 and the site was marked with radiotherapy-like ink. Stitches were removed one week later. The rats were sacrificed four months after the procedure, by high dose anesthetic intracardiac injections. The region between the ears of the animals in which the mucosa had been implanted, from the epidermis to the muscle layer, was collected for histopathological analysis. The collected samples were processed according to the conventional standardization, with buffered formol 10%, inclusion in paraffin, microtomy, and staining with hematoxylin-eosin, Masson's trichrome and toluidine blue.
RESULTS
Out of the total 12 rats submitted to the surgical procedure, one died during the surgery because of respiratory depression. The remaining 11 rats were well for the other 4 months; after sacrifice, we collected samples from the mucosal implanted region for histopathological analysis.
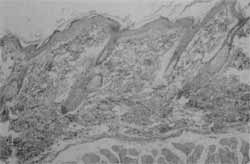
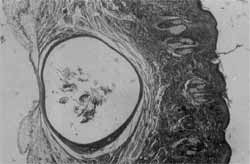
The epidermis was preserved in all fragments, as well as the subepithelial connective tissue (dermis) and the skeletal muscle layer (Figure 1). In none of the 12 studied cases did we find any signs of the mucosa between the skin and the muscle layer (Figure 2). In the fragments obtained from six animals the tissue was structurally normal. In one of the 11 cases, we observed focal mononucleated inflammatory infiltrate. In one sample, we noticed the existence of fibrin leukocytarian crust, with retraction of epidermis and presence of a large quantity of neutrophils and bacteria (coccus) on the surface. In samples from 3 animals we found inclusion epidermoid cysts, showing large amount of keratin and some hairs inside it (Figure 3).
We did not find any indication of the implanted mucosa, nor local inflammatory reaction, except for one case.
DISCUSSION
In the experimental study, we did not find signs of the mucosa implanted under the skin in the 11 studied cases. The finding of inclusion epidermoid cyst may be a result of the mononylon stitch used to close the incision, which might have carried some epidermis cells into the tissue. The fibrin leukocytarian crust was probably a result of the manipulation of the incision by the animal, leading to secondary bacterial infection.
These results led us to the conclusion that the mucosa seems to be a guide for uniform healing, restitutio ad integrum, preventing the epidermis from getting retracted in the region in which the nasal dorsum has small irregularities.
Figure 1. Overlaid skin and skeletal muscle, no signs of implanted mucosa (HE AOX63).
(FIGURA 2, PÁG. 521)
Figure 2. Detail from the previous Figure at the level of the implant.
The mucosa was probably reabsorbed by the organism and did not leave any remains. Since in rhinoplasties we do not apply stitches on the nasal dorsum, we prevent the complications that were noticed in this experiment, such as secondary infection and inclusion epidermoid cyst.
There are a number of reports of the use of middle concha to correct CSF fistula15, but there is no literature report of the use of this kind of graft in rhinoplasty. As to the use of concha bone, we believe that it is extremely useful because the nasal concha is at the same operation field and it is easy to manipulate, preventing another surgical time to harvest a structure that would be used for the correction of the nasal dorsum.
We performed a number of surgeries in the Department of Otorrhinolaryngology at Santa Casa de São Paulo using this technique, with positive esthetical results. For this reason, we decided to conduct the experimental study in order to learn more about the behavior of the mucosa under the skin. Next, we report some cases in which we used only mucosa and others in which we combined the use of mucosa and concha bone. The purpose of conducting the experimental study and presenting these cases was to open the perspective of the use of inferior nasal concha, making the surgical procedure easier, since inferior partial conchotomy is a procedure frequently conducted during rhinoseptoplasty. Post-operative results of patients were extremely favorable and they are all satisfied with the surgical esthetical results. Three of the patients have been operated on for over 2 years, with a maximum follow-up of 3y5m.
Figure 3. Inclusion epidermoid cyst in the hypodermis (HE AOX25).
CASE REPORT
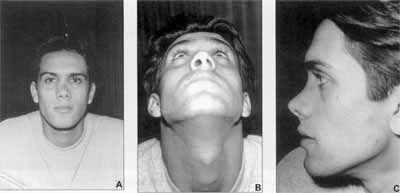
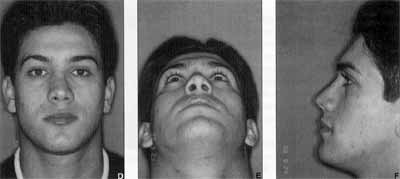
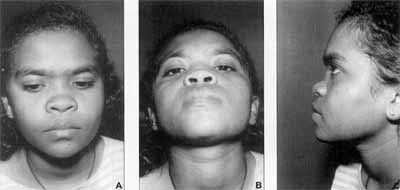
FC, 22-year-old male, was admitted on 19/May/97. Constant nasal obstruction, worse on the left nasal fossa and deviated nose to the right after a car accident that had taken place two months before. At ENT examination, he presented laterorrhinia, deepening of the nasal bone on the left and wedge septal deviation, occluding the left nasal fossa. The patient was submitted to rhinoseptoplasty in August 1997, with septal straightening, inferior partial conchotomy, median and paramedian osteotomies to centralize the nasal pyramid and placement of multiple cartilage fragments collected from the nasal septum to correct the deepening of the bone. The nasal dorsum was extremely irregular upon palpation and in order to repair the defect, the authors used inferior concha mucosa. The patient was extremely satisfied with the esthetical and functional postoperative result12 (Figures 4A, 4B, 4C, 4D, 4E and 4F).
Figures 4A, 4B, 4C. Pre-operative
Figures 4D, 4E, 4F. Post-operative.
DC, 22-year-old female, was admitted on 27/July/ 95.
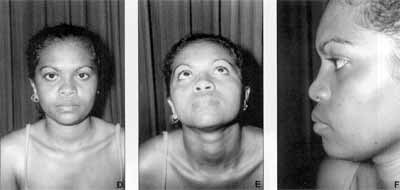
She reported pain on the nose and head, nasal obstruction, fever and hard palate lesion for 5 years. She had been hospitalized for 19 days in another hospital for clinical treatment with antibiotics, but she progressed with deepening of the nasal dorsum. At admission, she complained only of the appearance of the nose, no longer referring nasal obstruction. The ENT examination revealed lowered bone nasal dorsum. The septum was centered and turbinates were discolored and hypertrophied. There was no palatal sequela. We conducted serology for syphilis and leishmaniosis, which were both negative. In August 1996, the patient was submitted to rhinoplasty with placement of right auricular graft. However, she was not satisfied with the results because the nasal dorsum seemed to be lowered. She was operated on in November 1997 with implantation of left auricular tissue through transfixing septum and intercartilaginous incisions. Since the dorsum remained lowered, we decided to perform inferior conchotomy and use conchal bone and mucosa from the nasal concha, which were carefully dissected as grafts. The bone was placed on the cartilage of the auricle and the mucosa was positioned on top of the two grafts to correct irregularities. The patient was very satisfied with the esthetical result (Figures 5A, 5B, 5C, 5D, 5E and 5F).
Figures 5A, 5B, 5C. Pre-operative.
Figures 5D, 5E, 5F. Post-operative.
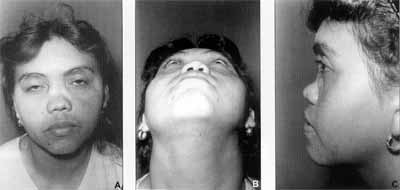
MMBCS, aged 34 years and born in Ceara, Brazil, admitted on 03/f anuary/96.
Nasal obstruction since childhood. The mother reported that the patient's nose had deepened when she was 3 months old. Since then, she had been complaining of bilateral nasal obstruction, worse on the left, and presenting rhinorrhea and crusts. She was a chronic user of topical nasal vasoconstrictor. At ENT examination, she presented lowering of nasal dorsum, mild wedge septal deviation to the left, as from zone I, and hypertrophied right nasal concha. The left nasal fossa was wide. Serology for syphilis and leishmaniosis were negative. In December 1996 we conducted rhinoplasty with placement of graft from both auricles, preserving the perichondrium. On the loth postoperative day the patient presented purulent secretion discharged through the intercartilaginous incision on the right. We introduced antibiotics (3rd generation cephalosporin) but on the 23rd postoperative day, there was a lcm-bulging on the right lateral nasal wall, close to the canthal ligament. After drainage and removal of serosanguineous secretion, we maintained the antibiotics. After 15 days, the infection regressed, but after some time she experienced graft reabsorption. In December 1998, the patient was reoperated on and we preferred to conduct right inferior conchotomy and placement of conchal bone over the nasal dorsum, recovered by carefully dissected nasal concha mucosa. Although the patient does not have esthetical complaints any longer, she still presents nasal fossa crusts (Figures 6A, 6B, 6C, 6D, 6E and 6F).
Figures 6A, 6B, 6C. Pre-operative.
Figures 6D, 6E, 6F. Post-operative
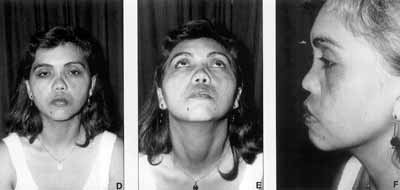
4) MFCM, 21 years old, admitted on 30/September/ 99.
Bilateral nasal obstruction since childhood, worse on the left side, plus deviated nose. She reported two minor surgeries, the first one two years before, but she still maintained the complaints of deviated and obstructed nose. At ENT examination, she presented deviation of the cartilaginous pyramid to the left, septal deviation to the left (Zones I and II), and moderately hypertrophied inferior nasal concha. We performed rhinoseptoplasty in December 1999, with displacement of dorsum, septoplasty, median and paramedian osteotomies, bilateral inferior conchotomy; placement of graft fragments of nasal septum cartilage and carefully dissected nasal concha mucosa over the dorsum, to correct irregularities. Postoperative result so far has been satisfactory.
VT, 16 years old, admitted and operated on in 1998.
Nasal trauma five years before, showing deepening of nasal dorsum and anterior septal deviation to the left, causing a fracture of the quadrangular cartilage of the septum. We performed rhinoseptoplasty using conchal bone graft and inferior concha mucosa, presenting good esthetical results so far.
REFERENCES
1. BAKER, T M. & COURTISS, E. H. - Temporalis fascia grafts in open secondary rhinoplasty Plast. Reconstr Surg., 93: 802-10, 1994.
23 CONLEY, J. - Intranasal composite grafts for dorsal support. Arch. Otolaryngol., 111: 241-5, 1985.
3. DE CAROLIS, V A. - A newly designed minigraft to achieve angularity and projection of the nasal tip: the asymmetrical bipyramidal graft. Ann. Plast. Surg, 30: 12230, 1993.
4. DINGMAN, R. O. & GRABB, W C. - Costal cartilage homografts preserved by irradiation. Plast. Reconstr Surg., 50: 516-7, 1972.
5. FONTANA, A.; MUTI, E.; CICERALE, D.; RIZZOTTI, M. Cartilage chips synthesized with fibrin glue in rhinoplasty. Aesth. Plast. Surg., 15: 237-40, 1991.
6. GUERREROSANTOS, J. - Nose and paranasal augmentation: autogenous, fascia, and cartilage. Clin. Plast. Surg., 18: 65-86, 1991.
7. GUNTER, J. P & ROHRICH, R. J. - Augmentation rhinoplasty: dorsal onlay grafting using shaped autogenous septal cartilage. Plast. Recontr Surg., 86: 3945, 1990.
8. MAHÉ, E.; HARFAOUI-CHANAOUI, T.; FARGES, D.; BARRAULT, S.; ZOJAJI, A. - Le greffon cartilagineux conchal "delta"dans les rhinoplasties secondaires ou post traumatiques. Ann. Chir. Plast. Estbet., 36: 209-14, 1991.
9. MCKINNEY E - An aesthetic dorsum. The CATS grafts. Clin. Plast. Surg., 23: 233-44, 1996.
10. PATROCINIO, J. A. - O use do implante de carbono na correção cirúrgica do nariz em sela. São Paulo, 1985. (Tese - Mestrado - Escola Paulista de Medicina).
11. PEYNEGRE, R.; BOSSARD, B.; GILAIN, L.; DELACOUR, L; LACCOURREYE, O.; COSTE, A.; CHABARDES, E. - Le greffon de poudre d'os amalgame et arme dans la correction de Parke nasale. Ann. Otolaryngol, 107: 715, 1990.
12. PEREIRA, C. S. B.; DOLCI, J. E. L.; DESTAILLEUR, D. E. L. - Uso de enxerto autógeno de mucosa de concha nasal para a correção de irregularidades do dorso nasal em rinoplastias. Apresentação de um caso. Anais do 34° Congresso Brasileiro de Otorrinolaringologia (Porto Alegre), pg. 209, 1998.
13. ROMO III, T. & SHAPIRO, A. L. - Aesthetic reconstruction of the platyrrhine nose. Arcb. Otolaryngol. Head Neck Surg., 118: 837-41, 1992.
14. SCHULLER, D. E.; BARDACH, J.; KRAUSE, C. J. Irradiated homologous coastal cartilage for facial contour restoration. Arch. Otolaryngol. Head Neck Surg., 103: 125, 1977.
15. WAX, M. K.; RAMADAN, H. H.; ORTIZ, O.; WETMORE, S. J. - Contemporary management of cerebrospinal fluid rhinorrhea. Otolaryngol. Head Neck Surg.,116: 4429,1997.
16. WOLFE, S. A. - Autogenous bone grafts versus alloplastic material in maxillofacial surgery. Clin. Plast. Surg., 9: 539-40, 1982.
* Post-Graduate studies in Otorhinolaryngology under course (Doctorate), Faculdade de Ciências Médicas da Santa Casa de São Paulo.
** Joint Professor, Department of Otorhinolaryngology, Santa Casa de São Paulo.
*** Post-Graduate studies in Otorhinolaryngology under course (Master), Faculdade de Ciências Médicas da Santa Casa de São Paulo.
**** Ph.D., Head of the Department of Pathology, Santa Casa de São Paulo.
The first case reported here was presented at 34° Congresso Brasileiro de Otorrinolaringologia (see reference 12).
Address correspondence to: Departamento de Otorrinolaringologia da Santa Casa de São Paulo - Rua Cesário Mota Junior, 112 - Pavilhão Conde de Lara - 4° Andar.
Tel: (55 11) 3226-7235 - Fax (55 11) 222-8405.
Article submitted on February 13, 2001. Article accepted on April 27, 2001.