Year: 2001 Vol. 67 Ed. 3 - (18º)
Relato de Casos
Pages: 416 to 421
Paranasal Sinus Schwannoma: Case Report and Literature Rewiew.
Author(s):
Líscia, L. A. Ferreira*,
Ana L. A. Brandão*,
José A. M. Silveira**,
Marco A. M. Name*,
Sílvia R. M. Do Pratto***,
Fabiana Sperandio****,
Fabiana Gonçalez*****.
Keywords: schwannoma, nasal cavity, paranasal sinus, endoscopic sinus surgery
Abstract:
Schwannoma is the originary tumor of the myelin sheath support cells, which in general, involves either the axon of the spinal nerve root or the brain. It can barely involve the axon of the cutaneous nerve. In the nose and paranasal sinus, these tumors arise from the trigeminal maxillary trunk branches or from the autonomous nervous system intranasal schwannoma is rare, and comprises 4% of the nerve tumors of the head and neck. Clinically, the tumor is diagnosed by means of rhinorrhea and non-specific nasal obstruction. Pain, facial edema and proptosis are less commonly found, though. In patients with nasal tumor mass without history of allergy it is likely to be considered the intranasal neoplasia. The authors report a case of schwannoma of sphenoid sinus, and another of maxillar sinus with extension to the ethmoid sinus and nasal fossa of the committed site. Markedly regards were taken to the clinical, radiologic and histopathologic findings, as well as for surgical approach and post-operative follow-up.
![]()
INTRODUCTION
Intranasal schwannoma is a rare tumor that corresponds to only 4% of the neural tumors of the head and neck1. Although it is rare, schwannoma is still the most common peripheral nerve tumor that affects the upper airways18. It is considered by the literature as a benign tumor of slow growth, although it rarely experiences malignant transformation18.
In 1972 Iwamura et al.18, in a review of the international literature, reported 45 cases of nose and paranasal sinuses schwannomas, seven located intranasally, five located in the maxillary sinus, and 33 located concomitantly in the ethmoid cells and nasal fossa. There were only three cases of sphenoid sinus schwannoma reported in the literature3,15.
Schwannoma is a tumor originated from the supporting cells of myelin sheath, which generally involves the root axon of the spinal nerve or the brain, but it rarely involves the axon of the cutaneous nerve1. In the nose and paranasal sinuses, these tumors originate from the branches of the maxillary trunk of trigeminal and autonomic nervous system. There are no schwannoma of olfactory nerve because of the absence of Schwann cells around its axon18.
Macroscopically, the tumor is encapsulated, well delimited, spherical or ovoid. It has firm consistency and multinodular external surface. Histology of the tumor shows spindle and neoplasic Schwann cells entangled in various directions or forming spirals. The presence of Verocay corpuscles is typical. Nuclei are normally elongated, with bundles at the same plane, in palisade format1. Malignant schwannomas have a higher number of cells with a significant number of epitheliod elements. Histologically, schwannoma should be differentiated from neurofibroma, fibrosarcoma, fibrous hystiocytoma, osteosarcoma, fibrous dysplasia and ossifying fibroma1,5,14.
There is discrepancy in the reports of prevalence of this kind of lesion, which is probably due to the confusion concerning terminology and etiological classification of these tumors, shown by the variety of names used to refer to the lesion in the past. Although the terms neurinoma, neuroma, neurolemoma, neurilemnoma have been used as synonym of schwannoma, the correct designation, that is schwannoma, is based on histopathologic and etymological criteria18.
Intranasal and paranasal schwannomas present non-specific nasal obstruction and sometimes rhinorrhea. Pruritus and sneezes associated or not to epistaxis, pain, facial edema and proptosis are uncommon1,9,15. Diagnostic suspicion is based on anamnesis, ENT examination, nasal fibroscopy and imaging diagnosis, such as computed tomography (CT scan) and magnetic resonance imaging (MRI) of paranasal sinuses. Imaging diagnosis also provides information about extension of tumor into the intracranial compartment1. Differential diagnosis of a single intranasal lesion is complex and we should take into account that the lesion might be a lymphoma, esthesioneuroblastoma, squamous cell tumor or adenocarcinoma, hemagioma, pyogenic granuloma, gestation granuloma, inverted papilloma, intranasal extension of juvenile angiofibroma, intranasal glioma, and encephalocele2,4. Only pathology is definite for the diagnosis of schwannoma.
The advocated treatment is surgery, with complete exeresis of the tumor; access route depends on location and extension of lesion. Before the advent of endoscopic sinus surgery, surgical approach of nasal and sinusal tumors was lateral rhinotomy, lateral ethmoidectomy or skull base surgery13. Prognosis concerning this tumor is excellent, provided that it is completely removed.
The authors report a case of sphenoid sinus schwannoma and one case of maxillary sinus tumor with extension into the sphenoid sinus and nasal fossa on the affected side, emphasizing clinical, radiological and histopathologic data, surgical approach and postoperative follow-up.
CASE REPORT
Case 1
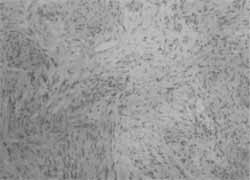
D. J. G. E, female 40-year-old patient, was admitted to Clinica Otorhinus presenting intermittent and moderate headache on the frontal region and superior-internal angle of the orbit, progressing for about 8 months. The pain was non-responsive to common analgesic and non-hormonal antiinflammatory drugs. Nasofibroscopy showed tumor on the left superior meatus, presenting polypoid non-obstructive aspect. CT scan of paranasal sinuses showed the presence of a solid mass that occupied anterior and posterior ethmoid cells and left sphenoid sinus, invading the nasal fossa but not intracranial or intraorbital spaces (Figures 1, 2 and 3). Histopathologic analysis of biopsy showed a tumor of Schwann cells (schwannoma) with no signs of malignancy (Figure 4).
The patient was submitted to tumor exeresis via endonasal approach. Postoperative follow-up was uneventful and after 11 months of follow-up there are no signs of recurrence according to endoscopic control.
Case 2
J. S. C., male 63-year-old patient, was admitted to Clinica Otorhinus complaining of right unilateral nasal obstruction for 10 years, moderate intermittent hemicranial right headache and throat clearing. In the past three years, nasal obstruction became bilateral followed by dyspnea in horizontal supine position, epiphora, poor visual acuity, phlogistic signs on the right maxillary region, right ear fullness, anosmia and objective cascomia.
Figure 1. CT scan at coronal section: observe the mass occupying the nasal fossa and left anterior ethmoid cells.
Figure 2. MRI (sagittal section): preserved floor of the anterior cranial fossa and no intracranial invasion.
Figure 3. MRI (coronal section): absence of continuity solution with anterior cranial fossa.
Figure 4. Presence of spindle cells with nuclear palisade, sometimes sparse. Cells are disposed in bundles.
At nasofibroscopy we observed a tumor mass of solid aspect occupying the right vestibule and nasal cavity, involved by foul odor purulent secretion. Pathology of the biopsy revealed Schwann cell tumor (schwannoma) with no signs of malignancy. CT scan of paranasal sinuses showed a solid mass occupying the right maxillary sinus, invading the ipsilateral nasal fossa and choana, pressing the nasal septum and causing erosion of posterior and medial walls of maxillary sinus and floor of the orbit with no intrachoanal or intracranial invasion (Figures 5, 6 and 7).
The patient was submitted to surgical exeresis via expanded Caldwell-Luc technique associated with endonasal approach. Intraoperatively, we noticed a brownish and smooth lesion, occupying the right maxillary sinus, with dehiscence of the floor of the orbit with extension into the nasal cavity, ethmoid sinus and rhinopharynx.
Early postoperative care was uneventful; throughout the nine months we did no detect tumor recurrence based on endoscopic control.
Figure 5. The CT scan at axial section shows a mass occupying the nasal fossa and the right maxillary sinus, displacing the nasal septum to the left and showing retention of secretion in the left maxillary sinus.
Figure 6. MRI (coronal section) showing mass occupying the right nasal fossa and the right maxillary sinus, displacing the nasal septum to the left.
DISCUSSION
Verocay described the neural sheath tumor in 1908, when it was believed that it derived from Schwann cells with a possible ectodermic origin. In 1910, the lesion was named neurinoma17. Teylanes and Rudosky, in 1926, reported the first case of neurinoma in the left nasal cavity and ethmoid sinus16. Donnelly et al., in 1992, in a review of the literature, observed that 32 cases of paranasal sinuses schwannoma had been described and only three of them had affected the sphenoid sinus5,15. It is interesting to point out that in Case 1 the schwannoma had originated from the sphenoid sinus and progressed into the ethmoid cells. As far as we know, this is the fourth case of sphenoid sinus schwannoma reported in the literature3,15.
Intranasal and paranasal sinus schwannomas are extremely rare and do not affect any specific age, sex or race18. The lesions are similar to other intranasal and paranasal sinuses neurogenic tumors, defining a variety of signs and symptoms that depend on the affected site, nerve of origin and/or compression of nerves and adjacent structures. Nasal obstruction, epistaxis, mucopurulent rhinorrhea, hyposmia, localized facial edema, pain and proptosis may be related to the tumor12. Robitaille et al.14 observed that nasal bleeding was frequently associated with ethmoid sinus and nasal fossa tumors, whereas pain was more common in maxillary sinus tumors. In the involvement of sphenoid sinus, the 3rd, 4th and 6th cranial nerves may be compromised by tumor growth12. In the cases described by the present study, initial symptoms were vague, with T zone headache and nasal obstruction in Case 2.
Figure 7. MRI at axial section: note the presence of a mass on the left and right nasal fossa and absence of intracranial and orbital invasion.
Histologic diagnosis of schwannoma is a challenge. Macroscopically, it is usually presented as an encapsulated solitary mass. The section surface of the tumor varies from white-grayish homogenous solid mass to red-yellowish masses with or without cystic areas. Microscopically, two distinct cellular regions are observed: Antoni A and Antoni B. Antoni A areas are regions with increase cellularity, spindle cells and retorted nuclei that do not frequently have distinguishable cytoplasmatic margins. Antoni B cells are frequently arranged in bundles and palisade. Components of Antoni B are entangled with Antoni A areas, and they are less organized areas, with low cellularity. Electronic microscopy and immunehistochemistry may be conducted in order to differentiate neurofibroma and other connective tissue tumors5.
Malignant schwannomas are aggressive tumors. They normally consist of a pre-existent area of neurofibroma. The malignant component consists of innumerous groups of spindle cells with significant epithelioid elements and moderate mitotic activity. Recurrence rate is usually high and there may be metastases into the lungs, but rarely into regional lymph nodes11.
The imaging techniques are available to assess the extension and the limits of schwannomas. Simple paranasal sinuses x-ray shows thinness or bone erosion with unilateral velamentum of one or more paranasal sinuses. CT scan is a radiological exam that provides more detailed information about bone structures and compromise of adjacent tumor areas10. High resolution CT scan with administration of intravenous contrast is the best modality to identify the presence of intraorbital and intracranial extension or soft tissue involvement. MRI is more efficient than CT scan to differentiate schwannomas from the other nasosinusal tumors, as well as from retention of secretion, inflammatory processes, glioma and encephalocele. The use of gadolinium enables precise delimitation of normal tissue from tumor tissue, which is useful for the assessment of intracranial and intraorbital extensions15. In the cases described here, diagnosis and definition of surgical approach were supported by these two exams.
Definite treatment of schwannoma is always exeresis of tumor, whenever possible en bloc, with preservation of adjacent structures, but access route depends on location and extension of tumor. In nasal fossa, ethmoid sinus and pterygoid maxillary fossa schwannomas, the surgical approach may be lateral rhinotomy external ethmoidectomy and endoscopic sinus surgery with preservation of infraorbital nerve and lachrymal system. Maxillary sinus lesions may be approached by Caldwell-Luc technique, with Denker extension, if necessary18.
In 1974, Calcaterra et al.3 reported that the extracranial approach of benign schwannomas of sphenoid sinus provided lower morbidity and more exposure than transcranial access. The authors also suggested the transantral approach with eccentric lateral extension for these tumors, but small intracranial extensions are contraindications for this approach. According to Calcaterra, in cases with more intracranial involvement, extradural craniotomy is necessary, followed by ipsilateral transantral approach3.
In Case 1, the endoscopic sinus surgery was enough to completely remove the tumor, but in Case 2 it required association with extended Caldwell-Luc approach.
Postoperative complications are rare, but CSF fistulae have already been reported18.
Radiotherapy is reserved as a palliative form of treatment for malignant schwannomas and in large intracranial extensions, combined or not with surgical resection; it may also be the only treatment intervention if surgeries are clinically contraindicated3.
The prognosis of benign schwannoma is normally good, differently from malignant schwannomas, which tend to be aggressive and have high recurrence rates3. Ghosh et al.6, in a review of 115 cases of malignant schwannomas reported 16 cases of head and neck tumor, with five-year survival rates of 65.7%. According to the authors, there was association with Von Recklinghausen disease in 30% of the cases, and these patients had worse prognosis and reduction of 5-year survival rate to 30%6.
In the follow-up of the patients reported here, there were no signs of tumor recurrence 11 months after surgery in Case 1 and nine months after surgery -in Case 2, confirming the good prognosis of benign schwannomas after complete resection of the lesion.
FINAL COMMENTS
In conclusion, benign schwannoma should be considered a non-usual mass found in the nasal fossa and paranasal sinuses. The nose and ethmoid cells are the most frequently affected sites; the presence of this tumor in the sphenoid sinus, such as in Case 1, is very rare and there have been only four cases (including ours) described in the literature.
Schwannomas should be differentiated from other benign lesions normally found in the region. CT scan usually suffices to define the evolution of these lesions; however, MRI enables the assessment of intracranial and pterygoid maxillary fossa extensions, in addition to differentiating schwannomas from other lesions, such as nasal glioma and encephalocele. However, the definite diagnosis comes from the result of the pathology and surgical resection within the safety margins is the treatment advocated.
REFERENCES
1. ARTHUR, B. D.; HERBERT, H. D.; WILLIAM, H. B. Intranasal Schwannoma: Magnetic Resonance and Computed Tomography Appearance. Am. J. Otolaryngology, 16(4): 251-4, 1995.
2. BARKOVICH, A. J.; VANDERMARCK, E; EDWARDS, M. S. B. et al. - Congenital nasal masses: CT and MR imaging features in 16 cases. Am. J Neuroradiology, 12: 105-116, 1991.
3. CALCATERRA, T. C., RICH, R., WARD, P W Neurilemnoma of the Sphenoid Sinus. Arch. Otolaryngol., 100: 383-5, 1974
4. DILLON, W E; SOM, E M.; ROSENAU, W - Hemangioma of the nasal vault: MR and CT feature. Radiology, 180: 761-765, 1991.
5. DONNELLY, M. J.; AL-SADER, M. H.; BLAYNEY, A. W Benign nasal schwannoma. Journal of Laryngology and Otology, 106: 1011-1015, 1992.
6. GHOSH, B. C.; GHOSH, L.; HUVOS, A. G.; FORTNER, J. G. - Malignant schwannoma, a clinicopathologic study. Cancer, 31: 184-90, 1973.
7. HILLSTROM, R. E; ZARBO, R. J.; JACCOBS, J. R. - Nerve sheath tumours of the paranasal sinuses: Electron microscopy and histopathologic diagnosis. - Otolaryngology - Head and Neck Surgery, 102: 257-263, 1990.
8. IWAMURA, S.; SUGIUR, S.; NOMURA, Y - Schwannoma of the nasal cavity. Archives of Otolaryngology, 96: 176-177, 1972.
9. JARROD, J. H.; NICK, S. J.; PATRICK, J. B. - The role of endoscopy in the management of nasal neoplasia. Am. J. of Rhinology, 11(1): 41-46, 1995.
10. MARTIN, J. D., MOHAMED H. A. S., ALEXANDER, W B. - View from beneath: pathology in focus. Benign nasal schwannoma. The Journal of Laryngology and Otology, 106: 1011-1015. 1992.
11. PERZIN, K. H., PANYU, H., WECHTER, S. - Nonepithelial tumours of the nasal cavity, paranasal sinuses and nasopharynx Cancer, 50: 2193-2202,1982.
12. RAMZIS, T. Y., CHARLES, W G., RANDE, H. L. Schwannomas of the paranasal sinuses: case report and clinicopathologic analysis. Arch. Otolaryngol. Head Neck Surg., 117: 678-680, 1991.
13. RICE, D. H. - Endonasal surgery for nasal wall tumors. Otolaryngologic Clinics of North America, 28: 1117-1125, 1995.
14. ROBITAILLE, Y, SEEMAYER, T. A., DEIRY, A. E. Peripheral nerve tumors involving paranasal sinuses: a case report and review of the literature. Cancer, 35: 125-48, 1975.
15. SRINIVASAN, V et al. - Sphenoid sinus schwannoma treated by endoscopic excision. The Journal of Laryngology and Otology, 113: 466-8, 1999.
16. TERPLAN, K.; RUDFSKY, F. - Uber zwei neurogene Tumoren in der Nasen and Mundhohle. Z Hals Nasen-Ohrenheilkd, 14: 260-8, 1926.
17. VEROCAY, J.; ZUR KENNTNIS der - "Neurofibrome." Beitr Pathol Anat Allg Pathol., 48: 10, 1910
18. WILLIAM, W M.; MARTIN, A. S.; EDWARD, J. R. Management of paranasal sinus schwannomas. Ann. Otol., 91: 63-69, 1982.
* Collaborating Physician, Discipline of Clinical Otorhinolaryngology, Faculdade de Medicina da Universidade de São Paulo (HCFMUSP).
** Director of Clinica Otorhinus, Ph.D., Assistant of Clinical Otorhinolaryngology, HCFMUSP, Assistant of Clinical Otorhinolaryngology, Casa de Saúde Santa Marcelina.
*** Otorhinolaryngologist.
**** Doctorate studies under course, Discipline of Clinical Otorhinolaryngology Faculdade de Medicina da Universidade de São Paulo (HCFMUSP).
***** Physician, Resident Preceptor, Clínica Otorhinus, responsible for seminars on Otorhinolaryngology at Clínica Otorhinus and Casa de Saúde Santa Marcelina.
Study conducted at Clínica Otorhinus - Centro de Estudos Alexandre Médicis da Silveira (CEAMS).
Address correspondence to: Clinica Otorhinus - Rua Cubatão, 1140 - 04013-044 São Paulo /SP - Tel: (55 11) 572-0025 - Fax: (55 11) 572-7373.
E-mail: otorhinus@ig.com.br
Article submitted on October 27, 2000. Article accepted on January 15, 2001.