Year: 2001 Vol. 67 Ed. 3 - (17º)
Relato de Casos
Pages: 411 to 414
Ludwing's Angina: Report of Two Cases.
Author(s):
Julio Rodrigues*,
Lara B. Coelho**,
Rodrigo G. S. Bastos**,
Michella C. L. Chayamiti**,
Rosemary M. Delegido***,
Cristina M. J. M. Finamore***.
Keywords: Ludwig's angina, sublingual space, submaxilary space, angina
Abstract:
The authors describe two cases of Ludwig's angina (LA) with -a review of the articles. A clinical diagnosis is realized without difficulty. The patients are hospitalized in order to receive antibiotics intravenously. The permeability of the superior respiratory tract is monitored and maintained. In the case where AL was caused by dental infection the treatment required an emergency tracheotomy.
![]()
INTRODUCTION
Ludwig's angina is a cellulite of submandibular space that may rapidly progress into upper respiratory obstruction, requiring emergency surgical intervention to guarantee permeability of upper airways. Infections of submandibular space may involve two different compartments - the sublingual compartment, that corresponds to the floor of the mouth and the submylohyoid space, limited superiorly by the lingual mucosa and inferiorly by the anterior layer of the deep fascia7. The floor of the mouth consists of the region limited by the mandibular gingival border, tongue inferior face and anterior pillars of faucial arch. It is deeply supported by the mylohyoid and geniohyoid muscles, which form the oral diaphragm. It has connections with the suprahyoid region, tonsil site and laryngeal walls1. These two sub-compartments communicate posteriorly through the mylohyoid muscle and that is why they are frequently affected7. Owing to the potential risk of death-related complications, patients with Ludwig's angina are hospitalized and medicated with powerful intravenous antibiotics.
The objective of the present case report was to show that, even under close hospital monitoring, some cases progress to emergency tracheotomy.
REVIEW OF LITERATURE
Ludwig's angina is a rare and poorly defined disease considered in many occasions a severe complication of dental infections of lower molars. It is correct to describe it as the involvement of suprahyoid space, classically showing an edema of hardened, wood-like and non-fluctuating consistency3.
As to incidence, it is more common in male subjects, aged between 21 and 30 years, and it normally evolves for 1 to 10 days before coming for medical assistance7. Etiology is attributed to dental alterations or recent dental manipulation in 44% of the cases, according to a study by Pynn et al. (1997). The dental cause may be either periodontal or periapical, and the latter is the most probable and can be easily differentiated at periapical tooth x-ray studies3. Schulman and Owens (1996) believed that Ludwig's angina after dental treatment could be a result of preexisting medical conditions, such as diabetes mellitus, malnutrition, alcohol abuse, neutropenia, systemic lupus erythematosus, aplasic anemia, glomerulonephritis - and not necessarily a direct result of dental manipulation6. Other uncommon etiologies include upper respiratory infections, trauma of the floor of the mouth, mandibular fractures and sialoadenitis2.
Differently from adults, there is no correlation between Ludwig's angina and dental decay in pediatric patients, as reported in a study by Kurien (1997), in which among 24 pediatric patients studied, none presented dental decay as the main cause. Conversely, adults presented dental decays as the main cause in 16 out of 31 studied cases3,5.
Predisposing factors are poor oral hygiene, local trauma and nutritional deficits6. The clinical presentation consists of hyperemia and hardened edema in the submandibular region, no fluctuation point, marked swelling of the floor of the mouth, pushing the tongue upwards and backwards, and progressive trismus. Depending on the size of the edema, it progresses to dysphagia, hoarseness and dyspnea. Fever and shivers may be associated8.
Lower molar odontogenic infections may cause a number of complications, in addition to Ludwig's angina, such as dental-cutaneous fistulae, osteomyelitis and cavernous sinus thrombosis. Cavernous sinus thrombosis and Ludwig's angina are associated with significant mortality and morbidity, whereas the other two complications are associated with morbidity and cosmetics. Nevertheless, mortality rate has declined considerably since the advent of effective antibiotics and invasive handling of upper airways (oral intubation, optic fiber intubation, cricothyroidectomy, tracheotomy)2.
Descending necrotizing mediastinitis is a rare and severe combination of Ludwig's angina, characterized by a large area of necrosis that starts from the neck and rapidly expands through the pre vertebral fascia, invading the thoracic cavity5.
Other complications include tongue necrosis, aspiration pneumonia and pulmonary abscess. The most common cause of death is asphyxia secondary to upper airway obstruction. That is the reason why we should control it before the onset of cyanosis and stridor8.
It is important to highlight that conservative treatment is more frequent in pediatric patients, with low incidence of tracheotomy. The rate of mortality is the same in adult and pediatric patients4.
One of the treatment options of Ludwig's angina is intravenous cephazoline 50 mg/kg/day TID, associated with metronidazole 30 mg/kg/day TID for a minimal period of 14 days, converting the drug for oral administration when the patient is ready for hospital discharge7.
In cases of mediastinitis, aggressive surgical interventions are required, including mediastinial drainage or more invasive surgical procedures, due to high mortality rates associated with the complication5.
CASE REPORT
Case 1
J.. C. N., 58-year-old man, came to the ambulatory complaining of severe odynophagia for 3 days and diffuse edema, especially in the submandibular region, that extended into the region of sternal furcula. He did not report fever. The patient reported systemic hypertension and previous history of renal stone.
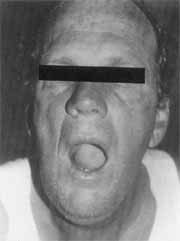
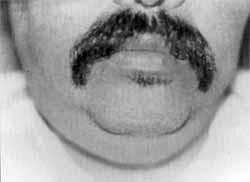
He presented significant submandibular and sublingual edema, elevating the tongue. At palpation, the neck had hardened consistency, showing wood-like aspect and drainage of purulent secretion by the ostium of right submandibular gland (Photos 1 and 2). Otoscopy and anterior rhinoscopy showed no alterations.
Photo 1. Elevation of tongue on the floor of the mouth of Ludwig's angina case. Case 1.
Photo 2. Lateral view of edema in submandibular and sublingual regions. Case 1.
The patient was hospitalized with diagnosis of Ludwig's angina secondary to sublingual gland infection. Intravenous medication was immediately introduced: cefuroxime 750 mg, metronidazole 500 mg and dexamethasone TID.
Laboratory tests showed slight deviation to the left at complete blood count, without leukocytosis. Lateral neck and mandible x-rays were normal.
The patient progressed to reduction of edema, pain and oropharyngeal secretion. There was no fever throughout hospitalization. The patient remained in hospital for 5 days and was discharged with oral medication and referred to outpatient follow-up.
He was reevaluated after treatment and presented completely resolution of the case.
Case 2
J. S. S., 46-year-old man, came to the ambulatory complaining of pain in the right lower molar region for 7 days and in the left region for 5 days. He also presented submandibular and sublingual edema, resulting in dysphagia, fever, intensification of pain and increase of edema.
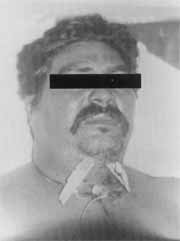
We observed a significant sublingual edema, projection of tongue upwards, followed by submandibular edema with wood-like aspect, enlargement of parotids and severe pain at palpation. There was drainage of purulent secretion from the second lower molars on the right and left side (Photo 3).
The patient was hospitalized with diagnosis of Ludwig's angina secondary to dental abscess.
At complete blood count, we detected anisocytosis, leukocytosis of 17,400/ mm³ (reference value [RV] 4,000 to 11,000/mm³), and toxic granulation of neutrophils (++), glucose 113 mg % (RV 70 to 110 mg %), Blood SR 27 mm (RV 3 to 8 mm for men). Lateral neck and chest xray did not demonstrate alterations. We did not perform periapical x-ray of affected teeth.
We introduced intravenous medication - initially crystal penicillin 4,000 000 UI QID, metronidazole 500 mg TID, amicacyn 500 mg BID and dexamethasone 4 mg TID.
After two hospital days, there was worsening of odynophagia, dysphagia and severe dyspnea, with no reduction of local edema. Blood SR was 73mm and leukocytosis was maintained.
We decided to conduct an emergency surgical drainage, under general anesthesia, through an external incision. A profusion of purulent secretion was drained and we also performed tracheotomy (Photo 4). We introduced intravenous vancomycin 500 mg QID and ceftriaxone 1 g BID and suspended amicacyn. We carried out culture of secretion, but there was no growth of microorganisms. Owing to feeding difficulties, we introduced a nasogastric tube. After the surgical procedure, there was reduction of edema and a great quantity of serous-blood secretion drained with Penrose drain. On the 5th day, we removed the drain and the nasogastric tube.
The patient was discharged on the 12th day showing good general status and significant improvement of sublingual and submandibular edema. The medication was kept up to the 21st day (ceftriaxone IM and metronidazole PO), with complete regression of the case.
DISCUSSION
Based on the reported data, we observed that both cases presented the classic clinical picture of Ludwig's angina, comprising typical sublingual and submandibular edema, severe pain and projection of tongue upwards. It was easy to come to a diagnosis based on clinical history and comprehensive physical assessment.
Photo 3. Frontal view of edema in submandibular and sublingual regions. Case 2.
Photo 4. Patient with tracheotomy and Penrose drains. Case 2.
Owing to the severity of the condition, we preferred to resort to intravenous large spectrum antibiotics, regardless of the cause. As to bacteriology, gram positive germs, followed by anaerobic agents are the most common; in addition to few cases of gram negative involvement.
As already mentioned, Ludwig's angina may present some kind of dental affection as a complication and it may be associated with sialoadenitis, oral cavity trauma or mandible fracture. The infections spread, not through the lymphatic system, but rather through the facial plans, owing to direct anatomic extension8. We could observe a favorable evolution in the first case, which was triggered by a bacterial sialoadenitis, with no need for invasive measures. In the second case, which was caused by a dental problem, there was worsening of respiratory condition because of expanded edema, even after the introduction of medication, requiring indication of tracheotomy and emergency surgical drainage. A possible reason for aggravation of the clinical presentation could be the time between the onset of symptoms and the beginning of drug treatment, which was 3 days in the first case and 7 days in the second.
Upon comparing the experience obtained in our service, we observed that Ludwig's angina from dental cause is normally more severe than events from other causes, presenting higher complication rates. The association of dental decay and Ludwig's angina is more aggressive, spreads faster and requires surgical intervention and early tracheotomy in addition to clinical treatments.
In view of these cases, we believe that the basic otorhinolaryngologic training should include practice in tracheotomy techniques, because we may face situations in which there is imminent risk of life because of upper airway obstructions.
FINAL COMMENTS
Ludwig's angina from dental cause is correlated with potentially fatal complications, such as upper respiratory obstruction that requires emergency tracheotomy. The treatment of Ludwig's angina is based on three basic aspects: 1) antibiotic therapy; 2) maintenance of permeability of upper airways; 3) hospital monitoring of clinical evolution in order to prevent potentially fatal complications, such as upper airway infections, aspiration pneumonia and descending necrotizing mediastinitis. The use of intravenous systemic antibiotic therapy is essential. Otorhinolatyngologists should be trained on how to perform tracheotomy.
REFERENCES
1. COSTA, S.S. et al. - Otorrinolaringologia: Princípios e Prática. 1: ed. Porto Alegre: Artes Médicas, 1994.
2. CORDERO, L., et al. - Descending necrotizing mediastinitis and respiratory distress syndrome treated by aggressive surgical treatment. The Journal of Cardiovascular Surgery, 37: 87-88, 1996.
3. FERRERA, E C., et al. - Uncommon complications of odontogenic infections. The American Journal of Emergency Medicine, 14: 317-322, 1996.
4. HARADEN, B. & ZWEMER, L. Jr. - Ludwig's Angina. Annals of Emergency Medicine, 30: 713-713, 1997.
5. KURIEN, M. et al. - Ludwig's angina. Clinical Otolaryngology and Allied Sciences, 22: 263-265, 1997.
6. MANIGLIA, J. J. et al. - Angina de Ludwig - Revisão de 5 anos / 27 Casos. Rev Bras. Otorrinolaring., 63:346-349,1997.
7. MARRA, S. & HOTALING, A. J. - Deep Neck Infections. American Journal of Otolaryngology, 17: 287-298, 1996.
8. SHULMAN, N. J. & OWENS, B. - Medical complications following successful pediatric dental treatment. The Journal of Clinical Pediatric Dentistry, 20:273-275, 1996.
* Head of the Service of Otorhinolaryngology, Santa Casa de Santos (SCS), Master in Otorhinolaryngology, Hospital das Clinicas da Faculdade de Medicina de Ribeirão Preto (FMRP), USP; Doctorate studies in Clinical Otorhinolaryngology under course, Faculdade de Medicina da USP
** Intern Physician, Service of Otorhinolaryngology, SCS.
*** Former Intern Physician, Service of Otorhinolaryngology, SCS.
Address correspondence to: Julio Rodrigues - Rua Carvalho de Mendonça, 366 - 11070-101 Santos /SP - Tel: (55 13) 3235-3082 - Fax: (55 13) 3232-5528.
Article submitted on August 18, 1999. Article accepted on February 8, 2001.