Year: 2001 Vol. 67 Ed. 3 - (12º)
Artigos Originais
Pages: 372 to 379
Validation of Computer Tomography in the Study of Mandibular Invasion in Tumors of the Tonsillar Fossa and Retromolar Regions.
Author(s):
Maria B. N. Pascoal*,
Abrão Rapoport**,
José F. S. Chagas***,
Ricardo P. Souza****.
Keywords: computorized tomography; neoplasias aropharynx, martinal mandibulectomy, tonsil, carcinoma
Abstract:
Introduction: The segmental resection of the ramus and angle of the mandible has been recommended since fortiers by Martin (1941), Slaugter (1949), Ward and Robben (1951), as part of the surgical treatment of the oropharynx tumors. This argument had been questioned based on the microscopic studies of the real mandibular bone involvement in tumors of oral cavity and oropharynx performed by Marcheta, Sako e Badillo (1964). The radiological findings has fundamental in the decision of the maintenance the continuity of the mandibular arch. Aim: Based on computer tomography evaluate, the extension of the bony mandibular involvement and of the pterygoid muscles, the relationship between the clinical presence of trimus and mandibular bony invasion and to quantify the real involvement and its relationship with the extension of the mandibular resection. Study design: Clinical prospective. Material and method: It was assessed mandibular invasion of 18 patients with squamous cell carcinoma of tonsillar fossa and retromolar region, prospectively. The trismus presence was also evaluated, associated to the evaluation previous radiological findings, through the tomography assessment of the mandibular bone invasion. The histopatological parameters of the resected bone was compared on to the tomography findings, as well as the presence of trismus. Results: There were two false-positives and 16 coincident evaluations. The statistical study through the Fisher's test demonstrated significant correlation for the two appraised approaches, with a value of p < 0,05. Conclusion: Tomography was an effective method to evaluation of the mandibular bone involvement and the previous evaluation of trimus also demonstrated correlation with the histopatological findings.
![]()
Summary
Introduction: The segmented resection of the ramus and angle of the mandible has been recommended since the 40's by Martin (1941), Slaugter (1949) and Ward and Robben (1951) as part of the surgical treatment of oropharynx tumors. This argument has been questioned based on the microscopic studies of real mandibular bone involvement in tumors of oral cavity and oropharynx performed by Marcheta, Sako and Badillo (1964). The radiological findings are essential in the decision making of preserving the continuity of the mandibular arch. Aim: Based on computer tomography, the purpose of the present study was to evaluate the extension of bone mandibular and pterygoid muscles involvement, the relationship between clinical presence of trismus and mandibular bone invasion and to quantify real involvement and its relation with the extension of mandibular resection. Study design: Clinical prospective. Material and method: Mandibular invasion of 18 patients with squamous cell carcinoma of tonsillar fossa and retromolar region was prospectively assessed. Presence of trismus was also evaluated, associated to the evaluation of radiological findings, using tomography assessment of mandibular bone invasion. The histopathological parameters of the resected bone were compared to CT scan findings and presence of trismus. Results: There were two false-positives and 16 coincident evaluations. The statistical study through Fisher's test demonstrated significant correlation for the two approaches, with a value of p < 0.05. Conclusion: CT scan is an effective method to evaluate mandibular bone involvement and previous evaluation of trismus also demonstrates correlation with histopathological findings.
INTRODUCTION
Up to the 70's, advanced tumors of tonsillar fossa and retromolar region were treated only with radiotherapy. Only tumors limited to the tonsillar fossa and radiotherapy resistant had surgical indication14,28. Disappointing results in patients with advanced lesions encouraged combined surgery-post surgical radiotherapy, improving survival rates4,16. Technically, the approach of posterior regions of the oral cavity and oropharynx through oral access was compromised by the difficulty to reach the deep limits of the lesion, and laterally it was affected by the presence of the ascending ramus of the mandible.
Crile10 created a monobloc surgery for malignant head and neck tumors, advocating the resection of the lesion, associated to segmented mandibulectomy and resection of lymph nodes, named composite surgery, based on the principles of resection of malignant breast, colon and rectum tumors, as published by Halsted and Miles23. The technique was abandoned because of high perioperative mortality rates. As from 1930, thanks to the advance in the area of antibiotics and anesthetic techniques, Ward in 1932, advocated the composite surgery for resection of oral cavity tumors, and Martin in 1941, proposed the composite resection for retromolar and tonsillar fossa tumors28. At that time, the concepts of tumor spread relied on the premise that mandibular periosteum would be an important route for tumor spread, reporting rates of up to 50%29. It was believed that esthetical and functional damage resultant from the resection of mandible bone would be secondary to the treatment of such an aggressive pathology23,28,29.
The poor quality of diagnostic methods - both histologic and radiological - at that time did not accept the concept of conservative resection. Ward and Roben created the so-called pull-through operation, advocating the maintenance of an intact mandibular arch. Despite its revolution at that time, the surgery was limited to less advanced tongue tumors or those extended into the gums, with minimum healthy tissue margin longer than 1cm29.
In addition to oncologic radical nature, the absence of mandible facilitated significantly the access and closure of soft parts. In some cases, the access was the only reason for its removal, because the removal of the lateral mandibular segment enabled access directly to the tonsillar fossa. Its absence reduced the "blank space", facilitating primary closure. It is important to point out that rehabilitation resources were equally limited at the time, based on approximation of soft parts with flaps of adjacent area, such as frontal flaps, skin flaps and prosthetic rehabilitation23,28,29.
In the beginning of the 60's, detailed and consistent studies about the mechanism of mandibular invasion showed that mandibular affection was noticed only in cases of mandible-fixed lesions. Even in very close lesions (3mm), the periosteum was free from tumor affection, questioning the spread of tumor tissue from the mandibular periosteum17. However, there was still the argument of easy closure, which was resolved as from the end of the 70's, thanks to the creation of the pectoralis major flap3.
All over Brazil, in the 70's, it was confirmed that the conservative surgery of mandibular arch, the pull through operation, for oral cavity advanced tumors did not compromise cure and survival, presenting rates similar to the data published by-the international literature1.
The theory of lymphatic spread through the mandibular periosteum was replaced by the concept of bone affection by contiguity, emphasizing other aspects, such as lesion site, its relation with mandibular bone and the degree of cortical infiltration, relevant for decision making about the most appropriate type of bone resection5,7,8,26.
The purpose of the present study was to evaluate through computed tomography, using pre-defined sections, the extension of compromise of mandibular bone and pterygoid muscle in squamous cell carcinomas of the retromolar region and tonsillar fossa. In addition, we aimed at correlating the clinical presence of trismus and mandibular bone affections, quantifying the real affection of the bone and its correlation with the extension of resection.
MATERIAL AND METHOD
The study comprised 18 patients (17 male and one female patients) with squamous cell carcinoma of tonsillar fossa and retromolar region treated at the Service of Head and Neck Surgery, Hospital a Maternidade Celso Pierro (HMCP), Pontifícia Universidade Católica de Campinas (PUCCAMP), between March 1999 and July 2000. As to age, the youngest patient was 36 years old and the oldest was 70; mean age of 51.3 years and median age of 51.5 years. The service started with a form containing general clinical data, collection of personal data and anamnesis. Next, patients were submitted to physical exam of oral cavity and oropharynx, by direct pharyngolaryngoscopy, using a rigid 2mm laryngoscope with 70° ocular lenses. We also performed bilateral palpation of oral cavity, oropharynx and neck to determine the degree of lymph node compromise. In the physical exam of oral cavity, in addition to evaluating the limits of the lesion, we analyzed the teeth and the presence of trismus. Absence of dentition was detected in 10 patients. Out of 8 dentulous patients, only two had posterior teeth, without metallic restoration. The six remaining patients had only anterior dentition. The diagnosis of presence of trismus was conducted through a subjective evaluation of mouth opening. Difficulty to open the mouth, secondary to painful reflex, was solved by collaboration of patients and infiltration of xilocaine anesthetic solution at 2%, with no vasoconstrictor. In patients in whom mouth opening was limited by pain after the infiltration, the opening was enough to conduct oroscopy The clinical sign of trismus, observed in 7 patients of the series, was considered an important factor to determine the affection of pterygoid muscles, and consequently, enabling mandibular invasion.
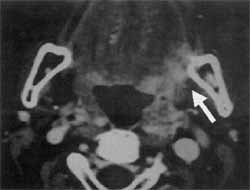
Figure 1. Axial CT section, with mandibular invasion.
Figure 2. Axial CT section in a "bone window" with mandibular invasion.
Most of the patients had lesions of the tonsillar fossa, comprising 14 subjects, and the other 4 cases had retromolar lesions. All patients were staged based on the classification table of malignant tumors by ILIAC (International Union Against Cancer-1997) and they were all at advanced cancer stages.
Out of 18 patients, five were T3 and the other 13 cases were T4. Lymph nodes impairment was noticed in 14 patients: in eight of them, there were ipsilateral lymph nodes smaller than 3cc (N1); in one cases, there were bilateral lymph nodes smaller than 6cm (N2c); in two cases, there were multiple ipsilateral lymph nodes smaller than 6cm (N2b), and in three cases they were larger than 6cm (N3). As to parameter M, no patients showed distant disease at thorax conventional x-rays. After the physical exam and clinical staging, the patients were referred to CT scan. In the present study, we standardized parapharyngeal space CT scan. usine 5mm-thick axial and coronal sections, parallel to the hard palate or the hyoid bone, with window for soft tissues and bone. The device used was a spiral tomographer SYTEC- SRI (General Electric), with images printed on the film brand AGFA, measuring 45cm X 35 cm. CT sections with contrast were obtained after forearm vein puncture with iodine contrast Meglumine 30. The mean number of contrasted phases was two. In the interpretation of CT scan sections, we emphasized the presence of tumor extension into pterygoid muscles, through a radiological sign of reduction and displacement of fatty contents in mastication space, and also by the presence of bone lysis evidenced by discontinuity of cortical surface at the level of mandible ramus and angle. The presence of positive radiological signs indicated mandibular affection. For such patients, we indicated segmented mandibulectomy. Biopsy was conducted in the first visit.
After signing the informed consent, approved by the Research Ethics Committee of Pontifícia Universidade Católica de Campinas, patients underwent surgical treatment and the surgical pieces were submitted to analysis in the same institution. Resected bone segments were submitted to previous process of decalcification with formic acid at 0.07% for smaller segments, and nitric acid at 1% for larger segments. The used staining method was hematoxillin-eosin.
All patients underwent surgical approach with monobloc resection, through bucopharyngectomy, associated with laryngectomy in two patients. The four patients without metastatic lymph nodes were submitted to neck dissection of levels I, II and III (supra-omo-hyoid dissection), and in one patient it was associated with contralateral supra-omo-hyoid dissection, because he had a lesion close to the palate midline. The rest of the series was submitted to modified radical neck dissection, unilateral in 9 patients and bilateral in two patients. Segmented mandibulectomywas conducted in 10 patients, and marginal mandibulectomy was performed in 8 cases.
Statistical analysis used exact Fisher's test, in 2x2 table, through the software SPSS (Statistical Package for Social Science), version for Windows 6.0 (1985-1993).
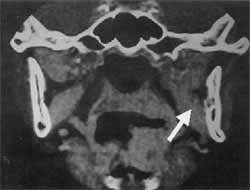
Figure 3. Axial CT section with no evidence of bone lysis.
RESULTS
Previous analysis of CT scan sections suggested extension of lesion into the limits of mandibular bone in 4 cases. By correlating CT scan findings and results of pathology we found only 2 patients with extension into the mandibular bone. Fourteen patients did not present bone compromise, confirmed by histopathologic results. Two patients were considered positive for mandibular affection (false-positive); however, pathology did not confirm mandibular involvement. Statistical analysis, conducted by exact Fisher's test, found 100% sensitivity and 87.5% specificity, and predictive positive and negative values of 50% and 100%, respectively. Value of p was below 0.05. In the clinical assessment, 4 patients presented trismus. When submitted to surgical approach, only two patients had mandibular bone affection, showing the false positive nature in the other cases. The exact Fisher's test was applied once again and found the same correlation between radiological signs and results of pathology, that is, sensitivity of 100% and specificity of 87.5% . As to evaluation of the correlation between presence of trismus and involvement of mandibular bone, the test presented a p value below 0.05.
Figure 4. Coronal CT section without bone lysis (the same patient).
TABLE 1 - Types of surgeries.
Key: ECU - unilateral neck dissection; ECB - bilateral cervical dissection; ECSOH - supra-omo-hyoid dissection; RR - rotation of flaps (pectoralis major myofascial flap); MS - segmented mandibulectomy; MM - marginal mandibulectomy.
DISCUSSION
As from the 70's, there were many publications in the international literature about the preservation of mandibular arch for oral cavity and oropharynx tumons4,15,20,21. The arguments reported as barriers to access the tonsillar region were compensated through the rebirth of median and paramedian mandibular osteotomy techniques, initially advocated by Roux (1836) and made popular by several authors13,18. There was significant advance in the methods of bone synthesis, through the use of metallic plaques that reconstructed the contiguity of mandibular arch. We had the opportunity to conduct marginal mandibulectomy associated with paramedian mandibulectomv in 8 patients of the series- and we confirmed the easy access to deep oropharyngeal regions and the easy handling of metallic plaques.TABLE 2 - Comparative analysis of the presence of mandibular bone damage, evaluated by computed tomography and histopathology.
Fisher's test: 0,040 P< 0.05
Sensitivity = 100 %
Specifications = 87.5 %
Positive predictable value = 50%
Confidence interval: [9.2% to 90.8%]
Negative predictable value = 100%
Confidence interval: [73.2% to 100%]
The maintenance of an intact mandibular arch started to be defended because it facilitated functional rehabilitation, produced an esthetical effect close to ideal, reduced hospital length of stay and recovery time, and above all, did not compromise cure rates.
There is only one technical inconvenience: in edentulous mandibles, absorption of alveolar bone leads to superficialization of the alveolar canal. The authors argued that in their researches the marginal techniques of resection on the limits of the canal affect the oncologic radical nature, because of its facility to perineurally spread. Therefore, segmented resection is indicated in tumors with mandibular bone compromise whose limits are close to the mandibular canal. In addition, the maintenance of the remains of a very thin mandibular arch, that is, thinner than 1cm, in marginal mandibulectomy may cause fractures1,5,8,15. The performance of 10 segmented mandibulectomy in our sample confirmed the theory reported above. Despite the indication of marginal mandibulectomy based on the criterion of bone affection, because of the thin mandible, we preferred segmented resection. In fact, in 3 cases, the fracture occurred during the mandibular osteotomy. But in all patients submitted to segmented resection, despite the unfavorable local criteria, the absence of bone involvement was noticed.
The theory of resection of mandibular arch in oropharynx tumors is still even more questionable than for the tumors of the oral cavity, because they are considerably distant from the mandibular arch. Even in advanced tumors, with affection of parapharyngeal space structures, and especially of the mastication space, the extension of the lesion into this region affects primarily the pterygoid muscles, before it approximates the ascending ramus of the mandible. The affection of pterygoid muscle leads to the clinical sign of trismus. We found only 4 cases of trismus among our patients, and only two of them presented histology evidence of bone compromise. The statistical analysis correlating presence of trismus and bone involvement was statistically significant. As highlighted in the material and method section; all our patients had advanced stages of cancer. The absence of trismus in the other 14 cases, as well as the negative evidence of mandibular bone affection, made us believe that even in advanced stages the disease remains restricted to the pterygoid muscle, sparing the mandibular bone. As previously reported, in the mechanisms of tumor extension, invasion of retromolar area and tongue base, with involvement of lingual sulcus, locally predisposes to invasion of mandibular bone, because they are areas adjacent to the lesion. In these regions, it is necessary to evaluate the interface between tumor tissue and mandibular bone on the internal face of the mandible and on the mandibular oblique line, which is the anatomical area that corresponds to the retromolar region.TABLE 3 - Distribution of patients with trismus correlated with the pathology.
Fisher's test: 0.040 P< 0.05
Sensitivity = 100%
Specificity = 87.5%
Positive predictive value = 50%
Confidence interval: [9.2% to 90.8%]
Negative predictive value = 100%
Confidence interval: [73.2% to 100%]
Therefore, the focus of preoperative assessment is not limited to the decision of sparing the mandible, but rather as how to assess its affection and level of extension. Radiological assessment of the mandible bone through the use of conventional x-ray, such as intra-buccal x-rays, panoramic x-rays and periapical films, among others, was widely debated in the literature, but there was no consensus about its use25,30. Lesions with massive destruction of the bone are easily diagnosed, even with clinical assessment. Minimal invasions are not early visualized. Conventional radiology is not capable of differentiating cortical lesions deriving from tumor infiltration from cortical alterations caused by bone remodeling resultant from dental loss, or by the presence of lesions resultant from benign pathological processes at the level of insertion periodontium. In addition, conventional x-rays provide a bidimensional image, whose overlapping of both cortical structures impair the visualization of bone reabsorption processes. In view of these limitations, bone scintigraphy presented as an alternative and effective method. However, subsequent studies showed that there were high rates of false positives. Bone scintigraphy could not differentiate benign inflammatory processes from tumor invasion30.
Computed tomography appeared in the beginning of the 70's and changed considerably the scenario of radiology as an evaluation method for oral cavity and oropharynx tumors. The first main advantage brought by CT scan was the possibility to visualize anatomical structures in deep spaces of the cervical region and its contiguity with the bone mandible structure, in addition to the possibility of acquiring very thin series of sections at axial and coronal planes. Magnetic resonance imaging surged as from the 80's and brought about technical advantages when compared to CT scan, but did not replace it.
The poor resolution of tomographers in the 70's might have initially discouraged its use. Thanks to the improvement and the development of modern devices and the creation of specific software to work with tridimensional images, the resources of CT scan multiplied, especially for the assessment of bone involvement11,12,19.
In our opinion, CT scan is an excellent method to evaluate and classify tumors of tonsillar fossa, because it provides detailed information about local and regional extension. Lateral displacement of structures in the parapharyngeal space, resulting in lack of precision or absence of fatty contents, loss of limits of muscles in the mastication space and, above all, the interface between soft tissues and ascending ramus of mandible, are considered relevant aspects to be investigated in the delimitation of malignant lesions of tonsillar fossa and retromolar region 2,12,19.
Disadvantages of CT scan include the need to use potentially toxic contrast, the generation of image distortion in the presence of metallic artifacts (restoration of amalgam, metallic crowns, osteosynthesis plaques, etc.), the difficulty to evaluate perineural involvement of mandibular canal, the difficulty to evaluate cortical irregularities after dental extraction and the need to change the patient's position to obtain coronal sections, as well as the impossibility of obtaining sagittal sections6,9,22,24.
Magnetic resonance has the advantage of capturing image at the three spatial planes and the patient does not have to change positions. The patient is submitted to lower doses of radiation and, as far as the assessment of the limits of lesion and healthy soft tissue is concerned, MRI presents more precision and does not have the inconvenience of producing distorted images because of metallic objects.
The authors that defend the use of CT scan state that in their studies MRI is still an expensive method and not readily accessible for routine assessments. It is not feasible in patients with claustrophobia, impossible to be conducted in patients with pacemakers and endoprostheses, and limited to assess small cortical infiltration9,22.
In our standardization of CT scan we decided to conduct tests of the parapharyngeal space. Although the tumors were not primary lesions from this space, parapharyngeal space CT scan was selected because it is capable of providing visualization of deep spaces of the cervical area. The standardization of sections at 5mm thickness clearly showed the interface between lesion and ascending ramus of the mandible in 14 patients, who were considered negative for mandibular involvement. In one of the patients with false-positive result for mandibular involvement, there was presence of trismus and invasion of hard palate. Therefore, we decided to conduct segmented resection of the mandible, but the histology revealed negative result for mandibular involvement.
Upon the submission of data to statistical analysis, we found correlation between CT scan and intraoperative findings, with 100% sensitivity, 87.5% specificity, positive predictive value of 50% and negative predictive value of 100%, which were findings in accordance with the international literature9,11,24,27.
As to disadvantages of CT scan, we could not analyze the distortions of images in the presence of metallic objects because in our sample there was a low incidence of posterior dentition and presence of metallic restorations. We found that sagittal sections were not relevant for the study of tonsillar region, especially for the assessment of mandible bone, and we did not find any different opinions reported in the literature. The change in position, requiring cervical hyperextension to obtain coronal sections, was not a limiting factor in our study because there were no patients who had functional limitations that prevented them from taking coronal sections. We believe that, except for patients with severe articular dysfunction, the "effort" of hyperextension is compensated by the registration of coronal sections, which helped us to evaluate mandibular involvement close to the condyle region. There is a international trend to consider CT scan more effective to detect cortical involvement and MRI more effective to evaluate medullar involvement. The explanation is based on the presence of fewer hydrogen nuclei in the cortical bone, producing an image of subtraction that is sometimes imperceptible in minimal invasions9.
We also agreed that CT scan has already become an accessible test to a large subset of patients, and even in public health care systems there are CT scan devices in the main oncology treatment centers, whereas MRI is still a privilege of some private institutions and it is costly to be performed if patients have to nay for it themselves.
One of the factors that seem to be more relevant for the success of the method is previous standardization of CT scan sections and good interaction of radiological and surgical team. We know that the anatomy of cephalic segment is very detailed and difficult to assess. A radiologist that is interested and familiarized with head and neck anatomical structures is capable of performing excellent CT scans to support investigation of bone invasion. In our opinion, the conduction of small CT scan sections (3mm), sections with "bone windows", supervision of the radiologist in order to reduce thickness of sections or modify cervical angle to reduce distortion caused by metallic objects, if necessary, seem to be capable of compensating the disadvantages that the exam present. The decision to preserve the continuity of the mandibular arch is an indisputable truth for oral cavity tumors, and it has become more acceptable for oropharynx tumors. We believe that in the near future, similarly to the innumerous reports for oral cavity tumors, studies defending the preservation of the mandibular contour will also confirm acceptable patients' survival rates. CT scan will undoubtedly have a key role to play in preoperative assessment.
CONCLUSIONS
1.) - CT scan presented significant correlation with histology and pathology results in 89% of the sample. Therefore, it was an effective evaluation method for the study of mandibular bone affection, motivating us to include it in our assessment battery of tests.
2.) There was correlation between clinical presence of trismus and bone involvement in 89% of the sample. Therefore, in the clinical absence of trismus, with no evidence of mandibular bone involvement, there is the possibility of conducting conservative surgical techniques, even in advanced cases.
REFERENCES
1. ANDRADE SOBRINHO, J. - Contribuição ao tratamento cirúrgico do câncer de língua, soalho da boca a gengiva inferior. [Tese de doutorado apresentada à Escola Paulista de Medicina SP], São Paulo, 1971.
2. APESTRAND, F.; KOBENSTVEDT, A.; BOYSEN, M. - Staging of carcinoma of the palatine tonsils by computed tomography. J. Comput. Assist. Tomog., 12 (3): 434-437, 1988.
3. ARIYAN, S. - Further experiences with the pectoralis major myocutaneous flap for the immediate repair of defects from excisions of head and neck cancers. Plast. Reconst. Surg., 64: 605- 609, 1979.
4. BARRS, D. M.; DeSANTO, L. W, O'FALLOW W- Squamous cell carcinoma of the tonsil and tongue base region. Arch. Otolaryngol., 105: 479-485, 1979.
5. BARTTELBORT, S. W; BARN, S. L.; ARIYAN, S. - Rim mandibulectomy of cancer of the oral cavity. Am. J. Surg., 154: 423-428, 1987.
6. BROWN, J. S:; GRIFFITH, J. F.; PHELPS, E; BROWNE, M.- A comparison of different imaging modalities and direct inspection after periostal stripping in predicting the invasion of the mandible by oral squamous cell carcinoma. Br. J. Maxillofac. Surg., 32: 347-359, 1994.
7. CARTER, R. L.; TASO, S.; BURMAN, J. F.; PITTAM, M. R.; CLIFFORD, E SHAW; H. J.-Patterns and mechanisms of bone invasion by squamous carcinomas of the head and neck. Am. J. Surg., 146: 451-455, 1983.
8. CLEARY, K. R.; BATSAKIS, J. G - Pathology consultation - oral squamous cell carcinoma and the mandible. Ann. Otol. Rhinol. Laryngol., 104: 977-979, 1995.
9. CLOSE, L. G.; BURNS, D. K.; MERKEL, M.; SCHAEFER, S. D.- Computed tomography in the assessment of mandibular invasion by intraoral carcinoma. Ann. Otol. Rhinol. Laryngol., 95: 383-388, 1986.
10. CRILE, G. - Excision of cancer of the head and neck with especial reference to the plan of dissection based on 132 operations. JAMA, 47:1780 1788, 1906.
11. CURRAN, A . J.; TONER, M.; QUINN, A.; WILSON, G. TIMON, C..- Mandibular invasion diagnosed by SPECT Clin. Otalaryngol., 21: 543-5454, 1996.
12. CURTIN, H. D. - Separation of the masticator space from the parapharyngeal space. Radiology, 163: 195-204, 1987.
13. DUBNER, S.; SPIRO, R.H. - Median mandibulectomy- a critical assessment. HEAD & NECI~ 13: 389-393, 1991.
14. KAJANTI, M. J.; MANTYLA, M. M. - Squamous cell carcinoma of the tonsillar region. Acta. Oncol., 30 (5): 629633, 1991.
15. KOMISAR, A.; BARROW; H. N.- Mandible preservation in cancer of the floor of the mouth. Arch. Otol. Head Neck Surg., 120: 1197-1200, 1994.
16. MALTZ, R.; SHUMRICK, D.; ARON, B.; WEICHERT, K. Carcinoma of the tonsil: Results of combined treatment. Laryngoscope, 84: 2172-2180, 1974.
17. MARCHETTA, F. C.; SAKO, K.; BADILLO, J. - Periosteal lymphatics of the mandible and intraoral carcinoma. Am. J. Surg., 108: 505-507 1964.
18. McGREGOR, L.; MacDONALD, D. G. - Spread of squamous cell carcinoma to the nonirradiated edentulous mandible- a preliminary report. Head Neck Surg., 9: 157-161. 1987.
19. MURAKI, A. S.; MANCUSO, A. A.; HARNSBERGER, H. R.; JOHNSON, L. E; MEADS, G. B. - CT of oropharynx, tongue base and floor of the mouth: normal anatomy and range of variations and applications in staging carcinoma. Radiology, 148: 725-731, 1983.
20. O'BRIEN, C. J.; NETTLE, W J.; LEE, K.- - Changing trends in the management of carcinoma of the oral cavity and oropharynx. Aust. N. Zel. J. Surg., 63: 270- 274, 1993.
21. PINSOLLE, V; TRUILHE, Y; MAJOUFRE,C.; MICHELET, V; PINSOLLE, J. - Resection mandibulare partialle posterieure pour cancer de la cavite buccale et de l'orpharynx. Ann. Chirurgie Plastique Esthetique, 42:223 -227, 1997.
22. SCHAEFER, S. D.; MARAVILLA, K.; SUSS, R.; BURNS, D.; NUNNALLY, R.; MERCKEL, M. A.; CLOSE, L.G. Magnetic resonance imaging vs. computed tomography. Arch Otolaryngol, 111: 730 -734, 1985.
23. SLAUGTH, D. E; ROESER, E. H.; SMEJICAL, W F. Excision of the mandible for neoplastic disease. Surgery, 26(3): 509-522, 1949.
24. SMITH, D. A ; O'DWYER, T. P; KEANE, C. O, STACK, J. S. - Predicting mandibular invasion in mouth cancer. Clin. Otolaryngol, 21: 265 -268, 1996.
25. SWEARINGEN, A.; Mc GRAW J. E; PALUMBO, V D. Roetgnographic pathologic correlation of carcinoma of the gingival involving the mandible. Surgery., 96(1): 15 18,1966.
26. TSAO, S. W; BURMAN, J. F.; EASTY, D. M.; CARTER, R. L. - Some mechanisms of local bone destruction by squamous carcinoma of the head and neck. Br. J. Cancer, 43: 392-401, 1981.
27. TSUE, T. T.; Mc CULLOCH, J. M.; GIRODI, D. A; COOPER, D. J.; WEYMILLER, E. A.; GLENN, M. - Predictors of carcinomatous invasion of the mandible. HEAD & NECK 16: 116 -126, 1994.
28. WARD, G. E.; HENDRICK, J. W - Tumors of the tonsils, pharynx, and base of tongue & metastatic tumors of the neck In: Diagnoses & Treatment of Tumors of the head and neck. Baltimore, The Williams & Wilkins Company, 1950, Chapters MI and XIX.
29. WARD, G. E.; ROBBEN, J. A. - Composite operation for radical neck dissection and removal of cancer of the mouth. Cancer., 4: 98 -109, 1951.
30. WEISSMAM, R. A.; KIMMELMNAM, C. E - Bony scanning in the assessment of the mandibular invasion by oral cavity carcinomas. Laryngoscope. 92: 1-4, 1982.
* Intern, Service of Head and Neck Surgery, Hospital a Maternidade Celso Pietro, Pontifícia Universidade Católica de Campinas/SP. Master in Head and Neck Surgery, Hospital Heliópolis - São Paulo /SP
** Coordinator of the Post-Graduation in Head and Neck Surgery, Complexo Hospitalar Heliópolis; Full Professor of Head and Neck Surgery, USP
*** Head of the Service of Head and Neck Surgery, Hospital a Maternidade Celso Pierro, Pontifícia Universidade Católica de Campinas /SP; Doctorate studies at UNIFESP
**** Head of the Unit of Imaging Diagnosis, Complexo Hospitalar Heliópolis - São Paulo/SP; Ph.D. in Medicine, USP
The present study is an extract of the Master thesis in Head and Neck Surgery presented at Complexo Hospitalar Heliópolis, on November 17, 2000.
Address correspondence to: Maria Beatriz Nogueira Pascoal - Rua Dr. Arnaldo de Carvalho, 555 - Apt. 113 - 13070-090 Campinas /SP - Tel: (55) 3243-0642.
Article submitted on January 18, 2001. Article accepted on February 6, 2001.