Year: 2001 Vol. 67 Ed. 3 - (5º)
Artigos Originais
Pages: 327 to 331
Tonsillectomy with CO2, Laser.
Author(s):
Lucas G. Patrocínio*,
José A. Patrocínio**,
Sônia Regina Coelho***,
Pérsio M. Amaral****,
Tomas G. Patrocínio*****.
Keywords: tonsillectomy, tonsillitis, CO2 laser
Abstract:
Introduction: The tonsillectomy is still the most common procedure in ENT. The modifications and the evolutions of the surgical technique aim to simplify and reduce the complications. The use of the CO2 laser is an innovation in the surgical treatment of these infections. Study design: Clinical prospective. Material and method: We operated 20 patient with diagnosis of chronic tonsillitis with debris and halithosis, adults, cooperative, without exacerbated nausea reflex. The procedure was executed under local infiltrated anesthesia, using 4 to 6 ml of lidocaine 2% with epinefrine 1:80.000, with the aid of the CO2 laser, 10 watts potency, superpulse continuous. The trans-operative bleeding incidence was smaller. Results: All the patients had developed with subjective improvement of the halitosis and without caseum elimination.
![]()
INTRODUCTION
Tonsillectomy is still the most common procedure in Otorhinolaryngology. The surgery has been modified through the years in order to simplify it and reduce the rate of complications8.
In Hindi scriptures, dated 3,000BC, there were descriptions of tonsillectomy. Celsius Cornelius, in Greece 50 years AD, described the surgery. At the same time, Paulo de Aegina demonstrated a procedure that consisted of the detachment of the mucous capsule with the finger and the enucleation of the tonsil. In 1958, Malecki wrote that the tonsillar tissue produced antibodies and consequently, surgical indications became more reliable7. In the 70's, thanks to the elucidation of immune functions, surgical decision became even more conscious, and the sole indication of tonsil or adenoid surgery was suggested because of the predominance of lymphoid tissue.
In children, tonsil hypertrophy is a result of the predominance of lymphoid tissue. In situations that take to upper airway obstructions, it is required to remove them. In adults, chronic tonsillitis results from the predominance of connective tissue and it may be necessary to remove them in pre-established cases.
Currently, tonsillectomy indications are well defined and are divided into absolute and relative. Absolute indications are: 1) tonsil hypertrophy with obstruction of upper airways; 2) sleep obstructive apnea; 3) suspicion of malignancy; 4) developmental deficit; 5) speech disorders; 6) eating and swallowing dysfunction; 7) dental malocclusion; 8) abnormalities of orofacial growth. Relative indications are: 1) recurrent infections; 2) carrier of group A (3-hemolytic Streptococcus; 3) halitosis; 4) peritonsillar abscess3,4,5.
The use of CO2 is an innovation in surgical treatment of these affections. There seems to be no advantage of its use under general anesthesia when compared to dissection, guillotine, electrocautery and high-frequency techniques, among others. Moreover, we should consider the strict care that must be taken when using CO2 laser in the operating room. Nevertheless, its use associated with local anesthesia makes the surgical act easier, and it is more comfortable and simpler for the patient and the surgeon. In order to confirm this fact and to identify further advantages or disadvantages of laser CO2 tonsillectomy, we conducted the present study.
MATERIAL AND METHOD
We operated on, 20 adult patients with caseous chronic tonsillitis and halitosis, who had surgical indication of tonsillectomy according to the appropriate indication criteria. They were all cooperative patients, did not present exacerbated nausea reflex and agreed to undergo tonsillectomy, under local infiltration anesthesia and CO2 laser.
Figure 1 - CO2, laser device, 20-watt power, used for tonsillectomy under local anesthesia.
Figure 2 - CO2, laser pen, 8mm-ceramic tip, used for laser tonsillectomy
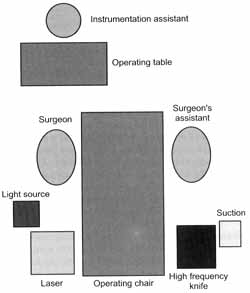
The equipment required for the surgery included a monitored ENT exam chair, 20-watt C02 laser device (Figures 1 and 2), smoke evacuator, frontal focus, high-frequency knife (Figure 3) and tonsillectomy material. Patients, as well as the whole surgical team, should wear protective glasses in order to avoid laser corneal damage. Layout of the team and the devices in the operating room is shown in Figure 4.
Figure 3 - High-frequency knives used as support in CO2 laser tonsillectomy.
The procedure was conducted under local anesthesia and the patient was semi-seated. The patient was informed that the back portion of his throat would be anesthetized and that there would be temporary absence of swallowing and breathing sensation. Next, we injected an intramuscular vial of anti-inflammatory (75mg diclofenaco) associated with an antiemetic (30mg dimenhydrinate). We sprayed twice to three times the posterior wall of oropharynx with lidocaine at 10% and infiltrated the palatine tonsil in three sites (Figure 5): in posterior and inferior pillars and in the middle of the anterior pillar, lateral to the tonsil, with 4 to 6mI of lidocaine at 2 % with epinephrine 1:80,000, overall. Before starting the surgery, we waited for the anesthetic effect and maximum vasoconstriction for 5 to 10 minutes after infiltration. There was no need for sedation.
During the procedure, the patient was instructed to breathe in deeply and to breathe out slowly and continuously for 10 to 20 seconds. Therefore, during expiration, we applied the laser in the pharynx, preventing the patients from aspirating smoke. The step was repeated until the end of the surgery. The controlled cycle of breathing elevated the soft palate, stabilized the tongue and reduced the risk of aspiration of smoke generated by the laser device, which may lead to nausea, cough and breathing difficulties.
We asked the patients to breathe in deeply and to open their mouths as much as possible. We also aspirated excessive saliva deposited in the pharynx. As a routine, we always started the surgery in the left tonsil. Using the curved tonsillar Allis clamp we grabbed the tonsil in the middle, pulling it to the middle line. We started the incision in the superior pole, in the space between the palatine tonsil and the anterior pillar, using 10 watt-power C02 laser at continuous super pulse, whereas the assistant operated the smoke evacuator. Gradually, we dissected towards the inferior pole, maintaining the anterior and posterior pillars. If there were major bleedings, uncontrolled by laser, we used an electrocautery or a high-frequency knife to cauterize the vessel or a number 1 silk thread to make a suture.
Figure 4 - Schematic representation of layout of team and equipment in the operating room.
Once the surgery was finished, we pressed a gauze soaked in bismuth subgallate on the surgical site for 2 to 3 minutes in order to control potential bleedings of minor vessels. We removed the gauze and made a last minute review, using the high-frequency knife to stop any other bleeding.
The surgery lasted 30 minutes in average and patients were immediately discharged from the hospital (Figure 6). Analgesic and anti-inflammatory were prescribed for one week. The patients received recommendations in writing about eating habits, general care and possible complications. Patients came back for post-operative evaluation 7 to 10 days later, when they were finally discharged.
Figure 5 - Schematic representation showing the sites (superior, medial-lateral and inferior) for infiltration of local anesthetic on the anterior pillar.
Figure 6 - Early post-operative care of a patient submitted to CO2 laser tonsillectomy under local anesthesia.
RESULTS
Out of 20 patients, 12 were male and 8 were female subjects, aged from 18 to 35 years (mean age of 26.5 years).
All patients submitted to the procedure had easily controlled traps-operative bleeding, using high-frequency knife cauterization. Post-op pain was the second most common complication, controlled by diclofenaco (75mg) before the procedure and after it, prescribed together with oral analgesic for 7 to 10 days.
There were two post-op bleeding episodes, one on the 4th and another on the 6th day, both minor and spontaneously resolved with no need for intervention.
All patients evolved with significant subjective improvement of halitosis and the complaint of caseous discharge.
DISCUSSION
A number of authors have described laser tonsillectomy1,6,11,12. Laser devices have a varied application in the area of otorhinolaryngology and facial plastic surgery. Since it is a high cost device, the more we use it for different procedures, the lower will be its final cost.
Soft tissues may be cut, vaporized or coagulated with laser, which is an advantage, reducing traps-operative bleeding and post-op pain6.
To use laser in the operating room we should follow a rigid protocol that requires from adaptation of the environment of the surgical room to type of endotracheal tube, because of the risk of O2 combustion.
In addition, we know that the risk of complications in such surgeries is minimal8. Therefore, we prefer to use the laser in the office, for ambulatory surgeries such as resection of nevi, blepharoplasty, wrinkle resection, LAUP and others.
Once confirmed the diagnosis of caseous chronic tonsillitis in adults and when the patients agree to the surgery, we believe that they should be informed about the possibility of performing tonsillectomy under local anesthesia with CO2 laser.
Different authors described good results with laser cryptolysis of palatine tonsils1,6,11,12. In our experience, the incidence of recurrence was significant, requiring second, third or fourth interventions to solve the problem of caseum discharge. On the other hand, dedicating some more time and effort during tonsillectomy, we managed to solve the problem for good.
Auf et al.1 stated that laser tonsillectomy is less painful and Strunk and Nichols11 said the opposite, stating that post-op pain is the same in both procedures. We agree with the former.
Undoubtedly, bleeding is reduced with laser. Bismuth subgallate, in addition to the hemostatic effect, facilitates the visualization of the major bleeding vessel, because it shows a red dot in the damaged area, which is dyed yellow because of the subgallate5,9,10,13.
CONCLUSION
This new procedure may be employed in adult cooperative patients who do not have exacerbated nausea reflex. It is an intervention that should be employed whenever possible due to its effectiveness, safety, comfort, speed and reduced bleeding. In addition, it does eliminate the risk of taking a general anesthesia and the need for hospitalization. When patients decide to undergo tonsillectomy, they should be given this therapeutic option. Despite the high cost of the laser device, the final cost of the surgery is reduced because of the simplification of the procedures. It is an interesting alternative that we should offer to our patients.
REFERENCES
1. AUF, L; OSBORNE, J. E.; SPARKES, C.; KHALIL, H. - Is the KTP laser effective in tonsillectomy? Clin. Otolaryngol., 22: 145-146, 1997.
2. CANNON, R. C. - Safety protocol for laser-assisted tonsillectomy. Laryngoscope, 108(8 Pt 1): 1249-1251, 1998. 3. ENDO, L. H. - Adenoamigdalectomia. In: PINTO, J. A. (org.). Ronco a Apneia do Sono. Rio de Janeiro: Revinter, 2000.p. 111-115.
4. HUNGRIA, H. - O problema das amígdalas a vegetações adenóides. In: Otorrinolaringologia. 8.ed. Rio de Janeiro: Guanabara Koogan, 2000. p. 167-170.
5. ISSA, A. - O use do subgalato de bismuto como agente hemostático em cirurgias de adenóides /ou de amígdalas. Ribeirão Preto, 1998 (Tese de mestrado - Faculdade de medicina de Ribeirão Preto - Universidade de São Paulo)
6. KRESPI, Y P; LING, E. H. - Laser-assisted serial tonsillectomy J. Otolaryngol., 3(5): 325-327, 1994.
7. MALECKI, J. - The antibody level in the tonsil. Parenchyma and its correlations. Arch. Otolaryngol., 67: 28-31, 1958.
8. MANIGLIA, A. J.; KUSHNER, H.; COZZI, L. Adenotonsillectomy A safe outpatient procedure. Arch. Otolaryngol. Head Neck Surg., 115(1): 92-94, 1989.
9. MOLINA, F. D.; et al. - A eficácia do subgalato de bismuto em tonsilectomias como agente hemostático. Rev. Bras. Otorrinolaringol, 66(3): 194-197, 2000.
10. NASSIF, A. C. N.; PATROCINIO, J. A. - O subgalato de bismuto nas amigdalectomias. RBM, 35(8): 505-506, 1978.
11. STRUNK, C. L.; NICHOLS, M. L. - A comparison of the KPT/532-laser tonsillectomy vs. traditional dissection/snare tonsillectomy. Otolaryngol. Head Neck Surg., 103(6): 966971, 1990.
12. SUPIYAPHUN, P; SIRICHAROENSANG, S. - Treatment of tonsillar crypt infection with CO2 laser. A preliminary report. J. Med. Assoc. Thai., 79(2): 133-136, 1996.
13. THORISDOTTIR, H.; RATNOFF, O.; MANIGLIA, A. Activation of Hageman factor (Factor XII) by bismuth subgallate, a hemostatic agent. J. Lab. Clin. Med., 112: 481-486; 1998
* Undergraduate, School of Medicine at Universidade Federal de Uberlândia - Uberlândia /MG.
** Faculty Professor and Head of the Service of Otorhinolaryngology Hospital de Clínicas, Universidade Federal de Uberlândia.
*** Otorhinolaryngologist of the Service of Otorhinolaryngology Hospital de Clínicas, Universidade Federal de Uberlândia.
**** Resident Physician of the Service of Otorhinolaryngology, Hospital de Clínicas, Universidade Federal de Uberlândia.
***** Undergraduate, School of Medicine, Pontifícia Universidade Católica de Campinas.
Service of Otorhinolaryngology at Hospital de Clínicas, Universidade Federal de Uberlândia and Department of Otorhinolaryngolog at Hospital Santa Genoveva - Uberlândia /MG.
Address correspondence to: José Antônio Patrocínio - Rua XV de Novembro, 327 / apto. 1600 - Bairro Centro - 38400-214 Uberlândia/MG. Tel/Fax: (55 34) 215-1143
E-mail: lucaspatrocinio@triang.com.br / lucaspatrocinio@doctor.com
Article submitted on September 21, 2000. Article accepted on February 9, 2001.