Year: 2001 Vol. 67 Ed. 2 - (18º)
Relato de Casos
Pages: 261 to 263
Sinonasal T/NK Cell Lymphoma - Case Report.
Author(s):
Míriam C. M. de Castro*,
Eduardo L. Silveira**,
Maurício Figueiredo***,
Carlos A. Ribeiro****.
Keywords: paranasal, neoplasm, lymphoma, paranasal cavity
Abstract:
Sinonasal lymphoma is rare, its diagnostic is dificult and almost ever late. T/NK cell lymphoma is a new terminology used for lymphoma that destructs midline facial tissue or aerodigestive tract. Many other terms are used to name this neoplasm: lethal midline granuloma, malignant midline reticulosis, idiopathic midline destructive granuloma, polymorphic reticulosis, midfacial necrotizing lesion, midfacial destructive lesion, pseudolymphoma, nonhealing midline granuloma, midline destructive granuloma and midline granuloma syndrome. A case of a primary non-Hodgkin's sinonasal lymphoma are reported and diagnosis emphasized.
![]()
INTRODUCTION
Malignant tumors of nose and paranasal sinuses are not frequent and represent approximately 3% of all head and neck cancer cases and 0.8% of all human cancer cases.
Among all lymphomas, 0.017% is located in the nasal cavity or the paranasal sinuses, and 0.44% of all extra-nodal lymphomas shares the same location. For non-Hodgkin lymphoma, nasosinusal tract hosts 1.5% of the tumors.
Patients may present a wide range of symptoms, including nasal obstruction, purulent secretion, epistaxis, sinusitis, odontogenic pain, visual disorders, syndrome of cavernous sinus, facial pain and syndrome of insensitive mentalis.
Due to non-specific symptoms, diagnosis is normally late, resulting in worse prognosis for the patient.
T/NK cell lymphoma is the most recently used term to represent an aggressive and destructive lymphoma of aerodigestive tract or facial midline tissues; it requires a immunohistochemical diagnosis in which we define the cell immune type as T/Natural Killer.
Other terminology used to define the pathology was polymorphic reticulosis, midline malignant reticulosis, lethal midline granuloma, midline idiopathic destructive disease, midfacial necrotizing lesion, midfacial destructive lesion, midline destructive granuloma, midline granuloma syndrome, non-healing midline granuloma and pseudolymphoma. T/ NK lymphoma has also been included in the category of angiocentric immuneproliferative lesions and in the European-American classification of lymphoid neoplasia it was included as a angiocentric lymphoma, and there is evidence of its association with EBV
The incidence of this kind of tumor is higher in Peru and Asia (China), between 6.7 and 7.2% in Asiatic countries and 8% in a study of patients in Peru, comparing to 1.5 % in the United States and 0.17% in Germany.
In a US study of 120 non-Hodgkin lymphomas, 65 were type B cell phenotype and 55 were type T cells.
T/NK lymphomas may manifest at any age; in addition, they are more predominant among male patients.
Such neoplasia normally disseminates to other extra-nodal sites, such as skin, subcutaneous tissues, gastrointestinal tract and testes.
There are reports of a hemophagocytic syndrome present in some cases of this lymphoma, associated with EBV which is normally fatal.
Five-year survival was 46 to 63 % in a study, but another study revealed mean 3-year survival of only 9%.
CASE REPORT
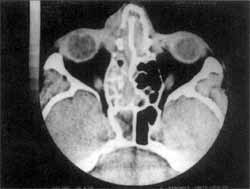
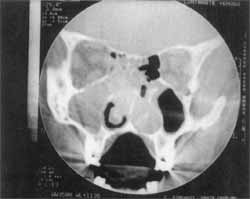
A 46-year-old patient with acute sinusopathy showed clinical improvement after the 4th cycle of antibiotics. He remained without complaints for 10 months, when he returned to the service with recurrence of acute episode and evolution to peri-orbital cellulite, despite the antibiotic therapy. Paranasal sinuses CT showed left pansinusitis with bilateral mass and septal destruction (Figures 1 and 2).
Figure 1. CT axial section of paranasal sinuses showing pansinusal impairment on the right.
Upon surgical biopsy, we noticed infiltration of septal mucosa occupying areas 3 and 4; it was irregular, pale, friable and had focal necrotic spots. We collected a biopsy of the material and sent to anatomic pathological analysis.
There was improvement of clinical condition after the surgery and the analysis presented a generalized inflammatory process, with focal necrotic spots and increased number of mitosis. We then proceeded to immunohistochemical analysis.
While we waited for the result of the study, there was another exacerbation of the symptoms, which was clinically controlled.
The immunohistochemical result showed T/NK (Natural Killer) cell lymphoma, with negative CD-20, focal positive CD-43, diffuse positive LCA, negative cytokeratins AE1/AE3, positive anti-KI-67 in approximately 80% of the cells, and positive CD-56, a result confirmed by two different labs. We conducted abdominal CT scan and biopsy of iliac crest for staging and they were normal. We then started chemotherapy with CHOP scheme (ciclophosphamide, doxorrubicin, vincristin and prednisone) - one cycle and the patient presented clinical improvement and was discharged from hospital.
Within one month, he returned with recurrence and exteriorization of tumor in the nasal fossa. We conducted a new biopsy and immunohistochemical reconfirmation. He started a new chemotherapy scheme - MINE (methotrexate, ifosfamide, novantrone, etoposide and mesne). At the beginning of the third cycle, the patient presented permeability of nasal fossae, absence of secretion and occasional maxillary sinus pain on the right.
Figure 2. CT coronal section of paranasal sinuses showing tumor infiltration in both nasal fossae, septum destruction and maxillary-ethmoid involvement.
DISCUSSION
Nasosinusal neoplasia is a pathology of late diagnosis because of non-specific clinical nasosinusal manifestations, requiring a high degree of suspicion when we face nonspecific and prolonged cases.
Symptoms such as facial pain, epistaxis, sinusitis, purulent secretion, odontogenic pain, nasal obstruction, sinusal cutaneous fistula, necrosis, ulceration and septal perforation, among others, maybe present, followed in some cases by fever and weight loss.
Of all cases of lymphoma, 0.017% is nasosinusal and among non-Hodgkin lymphomas 1.5 % is in the region.
CD-56 is a specific marker of Natural Killer lymphocyte, and T/NK lymphoma is a new terminology for a series of eponyms that previously classified the pathology. Its highest incidence has been described among Chinese (most of non-Hodgkin nasosinusal lymphomas), Peruvian and Mexican people.
It is a tumor of reserved prognosis, because the statistics on survival are conflicting: from 9% in a 3-year survival rate to 46 to 63% in a 5-year survival rate. Its incidence is equally distributed among all ages, most markedly in the 51 and 61 decades of life, predominantly in men.
REFERENCES
1. MICHEL B. CAHALI, LUIZ U. SENNES, MÁRCIA S. MURAKAMI, WALMIR E. E A. D'ANTONIO, CLÁUDIO M. Y IKINO, PATRÍCIA E SANTORO, ÍTALO R. T DE MEDEIROS, OSSAMU BUTUGAN - Tumores Nasossinusais Malignos: Espectro de apresentação nos últimos 15 anos.
2. MILLS, S. E. et all - Tumors of the upper aerodigestive tract and ear, 2000, 219 - 225; Armed forces institute of pathology, Washington DC.
3. PH E LEFEBVRE, S. TOMBU AND J.-E DEMANEZ - Non-Hodgkin's lymphoma of the paranasal sinuses-Report of two cases. Acta Otorhinolaryngologica Belg., 51, 93-98, 1997.
4. RICHARD E ROG, CAPT, DC, USN, BETHESDA, MD., Beware of malignant lymphoma masquerading as facial inflammatory processes. Oral. Surg. Oral. Med. Oral. Pathol., 71:415-9, 1991.
5. WILLIAM H. WILDER, MD; STEPHEN G. HARNER, MD; PETER M. BANKS, MD,- Lymphoma of the Nose and Paranasal Sinuses. Arch. Otolaryngol. -109: 104-7, 1983.
* Assistant Professor of the Discipline of Otorhinolaryngology at Faculdade de Ciências Médicas de Minas Gerais - Service of Obrhinolaryngology at Santa Casa de Belo Horizonte.
** Resident Physician of the Service of Otorhinolaryngology at Santa Casa de Belo Horizonte.
*** Otorhinolaryngologist at Santa Casa de Belo Horizonte.
**** Assistant Professor of the Discipline of Pathological Anatomy at UFMG.
Clinic of Otorhinolaryngology at Santa Casa de Belo Horizonte.
Address for correspondence: Eduardo Lemos Silveira - Rua Cabo Verde, 175/303 - Cruzeiro - 30310-260 Belo Horizonte/MG - Tel: (55 31) 287-0996.
Article submitted on July 6, 2000. Article accepted on September 28, 2000.