Year: 2001 Vol. 67 Ed. 2 - (13º)
Artigos Originais
Pages: 229 to 232
Tonsillectomy: Dissection Versus Sluder Technique.
Author(s):
Cécil C. Ramos*,
Maria E. R. Gonçalves**,
Mendonça, R. R.***,
Gualandro, D. M.***.
Keywords: tonsillectomy, surgical technique, Sluder guilhotine
Abstract:
Introduction: Although tonsillectomy is one of the oldest surgeries and more practiced all over the world, there are few works addressed to establish the best surgical technique. We aimed at to evaluate some surgical, clinical and laboratoryal parameters in attempt of establishing advantages and disadvantages among the principal surgical techniques. Study design: Clinical prospective. Material and method: The authors carried on a prospective study in children submitted to tonsillectomy, by means of dissection technique and Sluder guilhotine technique, in fortuitous way, aiming to determine which technician, physicians or laboratoryal parameters differ significantly between them. Results: Operative time and necessity of hemostasis by suture were, on average, shorter by Sluder technique, althoughh the clinical and laboratoryal parameters showed no significant difference. Conclusion: The tonsillectomy by Sluder technique presented larger advantages when compared with the dissection technique, mainly in small children.
![]()
INTRODUCTION
The surgery of palatine tonsil removal is one of the most ancient surgeries reported in medical history and still a frequently used procedure. There are reports of tonsil extirpation that dated back from 3,000BC; currently millions of these surgeries are conducted every year around the world. If, on the one hand, these figures seem to reflect a consensus, on the other hand, the choice for technique is far from being unanimous, since Physick first used a guillotine in 18272,8. In texts about Otorhinolaryngology, such as the academic production by Paparella and Ballenger, both the dissection and the tonsil guillotine technique (Ballenger-Sluder) are presented, but providing poor information about advantages and indications of each one.
In our experience as otorhinolaryngologists, since the first years in Medical School, we met professors and professionals that had definite opinions in favor or against the techniques, normally based on subjective observations and poor scientific evidence. Therefore, the literature brings few studies .that aimed at determining advantages and disadvantages of these theories, although a preference for dissection is normally noticed3,4,5,7,9.
The purpose of the present study was to analyze surgical, clinical and lab data to determine if there was a real difference in the use of one or the other technique.
MATERIAL AND METHOD
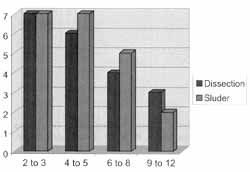
There were 41 patients who participated in the present study, ages ranging from 2 to 16 years (Figure 1), equally distribution of genders, randomly divided into two groups: those operated with the dissection technique and those operated with Sluder guillotine. In order to improve statistical treatment, patients were divided into age groups, as follows: 2 to 3 years (n=14), 4 to 5 years (n=13), 6 to 8 years (n=9) and 9 to 16 years (n=5). All patients were submitted to orotracheal intubation and were maintained under inhaling general anesthesia. The study was previously approved by the Committee of Ethics of Hospital Maternidade Cristovão da Gama.
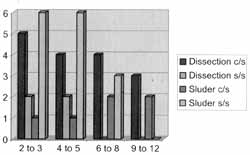
We analyzed surgical, clinical and lab parameters. At surgical time, we measured duration of surgery and need for conducting hemostasis of surgical suture (Figure 2). As to clinical assessment, we used a linear analog test adapted to our needs10,12: we asked patients to score from zero to 3 the severity of their pain (absent, mild, moderate or severe pain), pre-operatively and on the 3rd, 7th, and 14th post-op days. All surgeries were conducted by the same surgeon. Post-operative assessments were blindly performed by other member of the team, in order to follow up clinical sins, such as hyperemia on the surgical region, edema, secretions and fever. All patients were instructed to use post-op paracetamol if they experienced fever or pain. We also run complete blood test and clotting time pre-operatively and on the 3rd post-op day, as well as culture and antibiogram in case of suspected infections. Both the clinical and the post-operative measures are part of our practice routine.
Figure 1. Distribution of patients as to surgical technique used in each different age range.
Figure 2. Distribution of patients based on surgical technique and the need or not of having hemostasis of surgical stitches in each different age range (c/s with suture; s/s without suture).
RESULTS
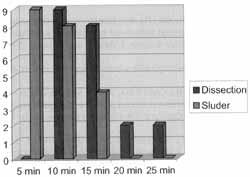
All children took paracetamol at the weight-correspondent dosage, and in no case it was necessary to complement with further medication. There were four cases with suspicion of surgical infection, which was not confirmed by culture and antibiogram; signs and symptoms resolved spontaneously and did not require antibiotics. As to surgical time, surgeries conducted with Sluder technique were made faster when compared to the group submitted to dissection, both in the global and in the age range analysis (Figure 3). The need for hemostasis of sutures was significantly smaller in the group operated by Sluder technique, although the difference tended to disappear as the age range increased (Figure 2). We did not observe statistically significant difference in any of the clinical studied parameters. Similarly, in lab parameters, we did not find significant difference between the two groups of techniques, although globally there were significant pre and post-op differences in some hematological parameters of the red series, but the significance was not maintained with the increase of age. In the analysis of clotting time, we did not find statistically significant differences both for the global analysis and the age group analysis.
DISCUSSION
We frequently observe heated discussions about advantages and disadvantages of different tonsillectomy techniques, both in academic and non-academic environments. Although advocators of techniques have a number of arguments, there are few studies that aimed at determining in practice if there are significant advantages of dissection technique, the so called classic technique, over the technique with Sluder guillotine. Since not always do teaching institutions allow residents to perform both techniques, the professionals are not able to evaluate the peculiarities of each method. Even for surgeons that dominate both techniques, evaluation is normally based more on subjective concepts than scientific evidence. Therefore, we tried to include the largest number of objective variables in the present study.
Associated with variation in surgical time, the frequency of hemorrhages that do not respond to local compression with gauze is a reliable parameter to evaluate morbidity of the technique4,12, although the experience of each surgeon may bias the interpretation12. In our study, the frequency of infra-operative hemorrhage and surgical time was significantly higher for patients operated on with the classic technique, although the significance was not maintained in older age ranges. We did not find in the literature any explanation to the lower frequency of hemorrhage in Studer's technique, although it seems obvious that shorter manipulation, confirmed by the surgical time, could be one of the explanations.
Figure 3. Distribution of patients based on employed surgical technique and duration of surgery (global analysis).
Based on the adapted analog linear study1,13, we did not find a significantly different answer between the two groups concerning severity of post-op pain, although we observed a significant increase in the number of complaints in older age ranges, as reported by the literature. Similarly, the other clinical parameters such as edema, presence of secretion, hyperemia on the surgical region and fever were not significantly different between the two groups.
We did not find in the literature data about differences in lab tests comparing different tonsillectomy techniques, although it is known that young patients may experience a significant loss of volemia in such procedures5. In our assessment, we observed a significant reduction of hematological parameters, such as hematocrit and hemoglobin in the CBC on the third post-op day, when compared to the pre-op CBC in the global analysis, confirming the data provided by the literature. However, in the analysis of the groups of each surgical technique, we did not observe statistically significant difference.
CONCLUSION
Our results suggested that some benefits may be derived from the use of Sluder technique, such as shorter surgical time and need for fewer sutures, although it has been clearly observed that these benefits were no longer evident as the age of patients increased. Nevertheless, we strongly believe that regardless of the results of the present or other similar studies, the experience of the surgeon is still what counts the most when it comes to choosing the surgical technique.
REFERENCES
1. BEYER, J. E.; Mc GRATH, E J.; BERDE, C. B. - Discordance Between Self-reported Behavioral Pain Measures in Children Aged 3-7 Years After Surgery. J. Pain Symp. Manag.; 5:350-356, 1990.
2. BREDA, D. - Indicaq6es de adeno-amigdalectomia. ECMAL; 3(1): 3-6, 1985.
3. BRUNETTO, B.; CASTILHA, A. M.; SACALUGA, F. - La adenoamigdalectomia como un procedimento ambulat6rio. Revista Otorrinolaringol. Cir. Cabeza y Cuello; 52(3): 16771, 1992.
4. CALVO, I. F.; NAVARRETE, A. - Morbilidad de la adenoidectomia y de la amigdalectomia en 100 pacientes escogidos al azar. Ann. Otorrinolaringol. Mex.; 38(2): 1079, 1993.
5. FAIGEL, H. C. - Tonsillectomy: a bloody mess. Clin. Pediatr 5:.652-3, 1966.
6. GERSTEL, R.; VAIDAS, S., GAITINI, I. - Effects of Peritonsilar Infiltration on post-tonsillectomy pain. Ann. Otol. Rhynol. Laryngol., 105: 868-870, 1996.
7. LAVY, J. A. - Post-tonsillectomy pain: the difference between younger and older patients. Int. J. Pediatr. Otorhinolaryngol., 42: 11-15, 1997.
8. LOPES FILHO, O. - Amígdalas: operar ou não a porque. Rev. Bras. Otorrinolaringol; 61(6): 496, 1995.
9. LUTZELER, M. - Evaluaci6n clinica de la amigdalectomia. Prensa Md. Argent; 73(8): 363-6, 1986.
10. MURTHY, E; LAING, M. R. - Dissection tonsillectomy: Pattern of post-operative pain, medication and resumption of normal activity. J. Laryngol Otol, 112: 41-44, 1998.
11. PINTO, J. Á.; PINHEIRO, J. M.; MEKHITARIAN NETO, L.; ANDRADE, N. V - Avaliação de acetaminofem, dipirona e placebo no tratamento de dor pós-amigdalectomia. Rev. Bras. Cir. 74(4): 185-90, 1984.
12. SANCHEZ, J. O.; GONZALEZ, J. V; ARIZA, J. V; CEDILLOS, L. A. R.; MONTANO, J. M. - Hemorragia posamigdalectomía. Revista Mex. Pediatr, 55(4): 183-4, 1988.
13. SANT'ANNA, G. D.; MAURI, M.; SILVA, D. B.; JUNIOR, H. C. - Dor pós-tonsilectomia: Comparação entre pacientes com diferentes idades. Rev. Bras. Otolaringol., 66(2): 1237, 2000.
* Otorhinolaryngology at FMUSE Doctorate studies under course at Faculdade de Medicina da USE Graduated from Faculdade de Medicina de Botucatu/SP - UNESP.
** Registered Nurse, Master studies under course at Faculdade de Medicina da Fundação ABC.
*** Undergraduate School of Medicine, Fundação ABC.
Study conducted at Hospital Maternidade Crist6vao da Gama, em Santo André/SP and presented at 35° Congresso Brasileiro de Otorrinolaringologia.
Address for correspondence: Cecil Cordeiro Ramos - Rua Gamboa, 245 - 09190-670 Santo André/SP - Tel: (55 11) 9266-9950 - E-mal: cecil@canbrasnet.com.br
Article submitted on January 15, 2001. Article accepted on March 19, 2001.