Year: 2001 Vol. 67 Ed. 1 - (7º)
Artigos Originais
Pages: 50 to 54
Nasalance Evaluation on Patients submitted to Functional Endoscopic Sinus Surgery.
Author(s):
Renata Soneghet*,
Rodrigo P. Santos**,
Mara Behlau***,
Gerhard Friedrich****,
Walter Habermann*****,
Heinz Stammenberger******.
Keywords: sinus surgery, nasality, nasalance, resonance
Abstract:
Aim: The aim of this study is to evaluate the nasalance before surgery, one day after surgery and approximately one month post-operatively, on patients with chronic sinusitis, submitted to functional endoscopic sinus surgery, by Messerklinger-Stammberger technique, using the nasometer as instrument. Material and method: Forty adult patients, German speakers with ages between 18 and 73 were evaluated at the ENT Dept. of the University of Graz, Austria. Sustained vowels "a", "i" and "u", repeated syllables with "m" and "n" followed by the same vowels and a standard nasal text, spoken at a comfortable level, constituted the voice samples. Results: The mean nasalance values of all samples, but "a" increased significantly one month after surgery. Conclusion: Nasometer was an excellent clinical tool, relative easy to use instrument, quickly administered by the speech therapist and provided reliable objective measurements of nasalance.
![]()
INTRODUCTION
Acoustic characteristics of voice are determined by two factors: sound source and vocal tract. Voice is initially produced by the vibration of the vocal folds at the passage of air. At that moment, it still has poor quality and no projection of sound into space. It is the resonance system, comprising the supraglottic area, pharynx, oral cavity, nasal cavity and paranasal sinuses that models vocal quality, acting as a resonator16. Resonance is the highlight of sound intensity of some specific frequencies of the sound spectrum and the attenuation of others². Minor alterations in configuration of these anatomical structures may produce substantial differences in vocal quality16.
In spite of the fact that the importance of certain supraglottic spaces as resonators of fundamental frequency is known, there is no consensus as to what is the real contribution of nasal cavity and paranasal sinuses in vocal quality. Proctor15 stated that one of the functions of the paranasal sinuses is to provide resonance to voice. Bunch³, however, said that "the sinus have small or no participation in vocal resonance, as perceived by the public".
Disorders of nasal resonance may be described in 2 categories: excessive nasality and insufficient nasality. In a hypernasal voice there is excessive use of nasal cavity and contamination of the oral sounds by the resonance. Air nasal escape reflects the turbulence of air that goes through the nose during articulation of consonants. It is the typical voice of lip and palate cleft and velopharyngeal inadequacy².
Hyponasality is present when there is obstruction of the nasal passage of air, hindering nose breathing. Therefore, nasal resonating system is partially or completely excluded. The loss of adequate nasal resonance takes away the brightness of the vocal quality, and vowel sounds become attenuated. However, loss of nasality is even more evident in the articulation of nasal consonants "m", "n" and "nh". In this case, the characteristic of continuity of nasal sounds is not maintained and they become similar to the corresponding plosive sounds: [p], [b] and [g], respectively. Hypertrophy of adenoids, nasal congestion and nasal polyposis, inflammation of soft tissues and septal deviations or deformities of the facial bones are common causes of hyponasality.
Nasality is an aspect of the vocal quality extremely studied by researches in the speech and articulation area. Absence, presence or degree of nasality have been perceptually evaluated by voice professionals in patients with different types of vocal disorders.
The use of instruments has become an important part of the diagnostic and treatment process of subjects with resonance disorders, because it adds objective data that are measurable during the clinical evaluation. Since the introduction of the nasometer in 19874, a number of articles were written discussing the use of the device to provide information about the different types of disorders that affect the resonance, such as the speech of patients with velopharyngeal insufficiency4, adenoid hypertrophy¹, upper airways impairment5,6, hearing, disorders and motor speech disorders, among others. In addition, nasometer has also been used in subjects with normal resonance17.
According to the literature, patients with chronic sinusitis submitted to functional endoscopic sinus surgery (FESS) reported to their physicians perceptual changes in speech. Despite these reports, there are few articles that describe the specific effects of FESS on vocal quality, and more especially, on resonance4,7,8.
The objective of the present study was to evaluate pre-operative, immediate post-operative and one month post-surgery nasalance in subjects with diagnosis of chronic sinusitis submitted to FESS using the technique of Messerklinger-Stammberger¹², and using nasometer as instrument.
MATERIAL AND METHOD
Forty adult patients participated in this study and 21 were women (52.5%) and 19 were men (47.5%), aged between 18 and 73 years, mean age of 39 years and standard deviation of 15.19, in the Department of Otorhinolaryngology at the University of Graz, Austria. The studied subjects spoke German, had never been submitted to nasal surgery, had no vocal disorder or motor speech disorder. They were all followed in the ambulatory because they had chronic sinusitis, associated or not with nasal polyposis. Patients were submitted to FESS using the technique described by Messerklinger-Stammberger18. This surgical technique was developed based on the pathophysiological theory of chronic sinusitis created by Messerklinger, in his studies conducted in the 50's and 60's¹° ¹¹ ¹². It requires opening of the prechamber of paranasal sinuses in order to restore drainage and airing. Messerklinger noted that the eradication of the primary anterior ethmoid affection by using a limited endoscopic surgical procedure resulted in recovery of the adjacent paranasal sinuses (frontal and maxillary) even without acting directly in the areas. It is a conservative technique in regards to removal procedures of nasal septum and conchae. The measure of nasalance, derived from the relation between the output of acoustic energy from the nasal and the oral cavities of the speaker was conducted using a nasometer model 6200-3 Kay Elemetrics. It consists on a system with directional microphone, positioned on both sides of a separating plaque that measures nasalance when the sign enters the system and shows the results in percentage plotted in a graph. When nasalance increases, the curve of nasalance elevates towards 100%, and when it falls, values of nasalance decrease towards the minimum point, the zero14.
Patients were asked to sustain phonation of each vowel "a", "ill and "u" for at least 5 seconds at comfortable intensity and frequency. They were also asked to produce syllables with "m" and "n" followed by the same vowels. Each syllable, was repeated 3 times. At the end, they were asked to read a standard nasal passage in German that has 33% incidence of nasal sounds normally used in clinical practice.
Vocal assessments were carried out pre-operatively as soon as patients were admitted to the hospital, in the immediate post-op, that it, one to three days after surgery, while they were in hospital and, finally, four to five weeks after surgery. Patients were asked to come to the outpatient unit for a post-op endoscopic assessment and cleaning of the nasal cavity before the last vocal assessment.
Results were submitted to statistical analysis using nonparametric tests (Wilcoxon Signed Ranks Test), with p+0.05.
RESULTS AND DISCUSSION
Based on the analysis of results, it was possible to determine a series of information about the effects of FESS on vocal quality.
There was a clear trend towards reduction of pre-op nasalance values compared to post-op ones, but only "a" and "ma" were significantly reduced.
The authors expected to find a significant reduction in all samples because of mucosa edema, possible crusts and presence of nasal packing. This expectation was not confirmed probably owing to the FESS technique proposed by Messerklinger-Stammberger, once it is a minimally invasive procedure which does not require large nasal packing and, consequently, does not block the passage of air.
Nasalance, one month post surgery, increased significantly in all samples when compared to immediate post-op results. The authors believe that as the edema reduces, crusts are eliminated and nasosinusal function is restored, resulting in elevation of nasalance values.
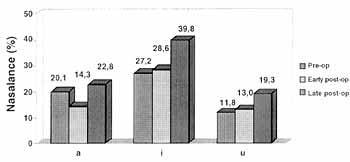
Graph 1. Mean nasalance of "a" "i" "u".
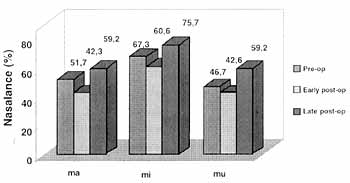
Graph 2. Mean nasalance of "ma" "mi "mu".
Comparing pre and one month post-op, our results showed that all mean values of nasalance for all samples (except "a") increased significantly.
Values of "i" went up from 27.2% pre-operatively to 39.8% post-operatively and values of "u" went from 11.8% to 19.5% (Graph 1).
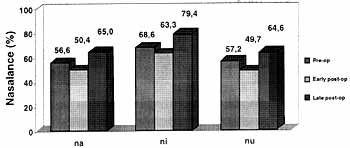
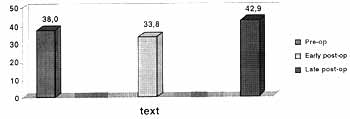
The same happened for "ma", "mi ",mu", in which nasalance values went from 51.7%, 60.6% and 46.6% in the pre-op to 59.2, 75.7% and 59.2%, respectively (Graph 2). Mean values of nasalance for "na", "ni" and "nu, as well as those of the standard passage, increased significantly from the pre-op to late post-op (Graphs 3 and 4).
Mackay and Kummer9 reported normal values of nasalance for "ma", "mi "na", "ni" in English speaking children. The corresponding nasalance means are 58.4, 78.7, 59.3 and 79.1, respectively. Nasal sounds "m" and "n" followed by the vowel "u" were not evaluated in their study.
Despite the fact that they are different languages and. populations, there is similarity between the mean values of normal English speakers and those found in German speaking people after one month post-surgery.
Graph 3. Mean nasalance of "na" "ni" "nu".
Graph 4. Mean nasalance of standard nasal passage.
Unfortunately, there are no further studies in the literature that share the same characteristics of this study, that is, patients submitted to FESS and analysis of nasalance of vowels, repetitive syllables with nasal consonants and standard passage, in order to compare the results.
However, it is possible to correlate the study by Hong et al.7, in which nasalance was evaluated in subjects who had nasal polyposis, before and after endoscopic surgery, using nasometer and a sentence that consisted of 34% nasal consonants. Nasal vowels were not evaluated since they are not available in the Korean language. The author found nasalance values of 45.7% before surgery that increased to 57.8% three weeks after it. In our study, the mean of nasalance of the standard passage in the initial assessment was 38% and it increased to 43.2% one month after (Graph 4).
Despite the fact that absolute nasalance values differ in both groups, there was a significant increase in nasalance after the surgery in both groups.
Müller¹³ determined normal values of nasalance for adult subjects speakers of German and found 33.2% as the mean nasalance for the nasal standard passage (Kindergeburstag).
The higher values of nasalance in our population may be related to differences in accent between speakers from Germany and Austria. Seaver et al.17 found variable nasalance because of the differences in dialects in four distinct geographical regions in Canada and the Unites States.
Results also showed a higher level of statistical significance for vowel "i" (P+0.001), when comparing pre-op values and those from 1-month post-op.
Analyzing the results of the questionnaire, 10% of the patients referred subjective changes in vocal quality after the surgery. This fact confirms the findings of Hosemann8, who found a subjective sensation of changed nasal resonance after surgery in 10% of the patients of his study.
CONCLUSION
Analysis of nasalance in this group of patients submitted to FESS let us concluded that despite the fact that the procedure is minimally invasive, it may produce significant changes in nasality.
The authors believe that it is essential to inform patients, especially professional voice users, about the possible effects of functional endoscopic sinusal surgery on vocal quality.
REFERENCES
1. ANDREASSEN, M. L.; LEEPER, H. A.; MACRAE, D. L. Changes in vocal resonance and nasalization following adenoidectomy in normal children: preliminary findings. Apresentado para a Sociedade Canadense de Otorrinolaringologistas a Cirurgiões de Cabeça a Pescoço, Montreal, 1990.
2. BEHLAU, M. S.; PONTES, P. - A Avaliação da Voz. In: Behlau, M. S.; Pontes P. Avaliação a Tratamento das Disfonias, São Paulo, Ed. Lovise, 1995, 56-141.
3. BUNCH, M, A. - Dynamics of the Singing Voice, Vienna, Springer-Verlag, 1992.
4. CHEN, M.Y. - Metson R. Effects of Sinus Surgery on Speech. Arch. Otolaryngol. Head Neck Surg., 123: 845 -52, 1997.
5. DALSTON, R. M.; WARREN, D. W.; DALSTON, E. T. - A preliminary investigation concerning the use of nasometry in identifying patients with hyponasality and/or nasal airway impairment. J. Speech Hear Res., 34: 11-8, 1991.
6. HARDIN, M. A.; VAN, DEMARK. D. R.; MORRIS, H. L.; PAYNE, M. M. - Correspondence between nasalance scores and listener judgements of hypernasality and hyponasality. Cleft Palate Craniof J., 29 (4): 346-51, 1992.
7. HONG, K. H.; KWON, S. H.; JUNG, S. S. -The assessment of nasality with a nasometer and sound spectrography in patients with nasal polyposis. Otolaryngol. Head Neck Surg., 117- 343-8, 1997.
8. HOSEMANN, W.; GÖDE, U.; DUNKER, J. E.; EYSHOLDT,U. - Influence of endoscopic sinus surgery on voice quality. Eur Arch. Otorhinolaryngol., 255: 499-505, 1998.
9. MacKAY, I. R. A.; KUMMER, A. W. - Nasometric evaluation of velopharyngeal function in non-literate subjects. 125th Meeting of Acoustical Society of America, May 17-21, 1993, Ottawa, Canada.
10. MESSERKLINGER, W. - Die normalen Sekretwege in der Nase des Menschen. Arch. Klin. Fxp. Ohr. Nas. Kehlkopfhedk, 195: 138, 1969.
11. MESSERKLINGER, W. - Endoscopy of the nose. Baltimore: Urban & Schwarzenberg, 1978.
12. MESSERKLINGER, W. - Die Rolle der lateralen Nasenwand in der Pathogenese, Diagnose and Therapie der rezidivierenden chronischen Rhinosinusitis. Laryngol. Rhinol. Otol., 66:- 293, 1987.
13. MULLER, R.; BELEITES, T. H.; KUHN, M.; HLOUCAL, U. Objektive Messung der normalen Nasalanz im sachischen Sprachraum. In: Aktuelle phoniatrisch - paedaudiologische Aspekte 1999/2000, Bd. 7, Manfred Gross (ed.). Heidelberg: Median-Verlag; 2000: 167-171. 14. Nasometer Model 6200-3 IBM PC Version Instructional Manual, 1987.
15. PROCTOR, D. F. - Breathing, Speech and Song, Vienna. Springer-Verlag, 1980.
16. SATALOFF, R. T. - Clinical Anatomy and Physiology of the Voice. In: Sataloff RT. Professional Voice: the Science and Art of Clinical Care, New York, Raven Press, 1991, 7-18.
17. SEAVER, E. J.; DALSTON, R. M.; LEEPER, H. A.; ADAMS, L. E. - A study of nasometric values for normal nasal resonance. J. Speech Hear Res., 34: 715-21, 1991.
18. STAMMBERGER, H. - Functional endoscopic sinus surgery. Philadelphia: BC Decker. 1991.
*Speech and Hearing Pathologist, Specialist in Voice at Centro de Estudos da Voz and in Head and Neck Cancer Rehabilitation at Santa Casa de São Paulo. Former Fellow of the Department of Phoniatrics at the University of Graz, Austria.
** Master degree in Otorhinolaryngology under course at Universidade Federal de São Paulo - EPM, Former Fellow of the Department of Otorhinolaryngology at the University of Graz, Austria.
*** Ph.D. in Human Communication Disorders - UNIFESP-EPM.
**** Head of the Department of Phoniatrics and Logopedics at University of Graz, Austria.
***** Assistant Physician of the Department of Phoniatrics at University of Graz, Austria.
****** Head of the Department of Otorhinolaryngology at University of Graz, Austria.
Study conducted in the Clinic of Otorhinolaryngology at University of Graz, Austria.
Study presented at 35° Congresso Brasileiro de Otorrinolaringologia, which was awarded a special citation. Study presented at The Voice Foundation's 29th Annual Symposium, on July 2, 2000, in Philadelphia, USA. Supported by ÖAD (Österreichischer Akademischer Austauschdienst), Austria.
Address for correspondence: Dr. Rodrigo de Paula Santos - Rua Botucatu, 740 - 30 Andar, Sala 23 - Vila Clementino - 04023-900 São Paulo /SP.
Article submitted on August 15, 2000. Article accepted on October 20, 2000