Year: 1992 Vol. 58 Ed. 3 - (5º)
Artigos Originais
Pages: 198 to 204
Efficacy of middle ear drug delivery systems: A comparative study on poly-l-lactic acid and collagen-based biodegradable membranes.
Author(s):
Marcelo M. Hueb, M.D., M.S.1,2,3,
Marcos V Goycoolea, M.D., M.S., Ph.D.1,4.5,
David Muchow1,4, e
Charles B. Ruah, M.D.1,6.
Keywords: experimental otitis media, drug delivery systems, biodegradable membranes
Abstract:
This study compared the efficacy of two different ampicillin incorporated biodegradable membranes in treating otitis media-induced cats (Eustachian tube-obstruction). When introduced in the middle ear, both devices were highly effective in preventing the chronification ar the continuam of tlte diseases when compared to the middle ears of untreated Eustachian tube-obstructed cats. The collagen-based membrane showed an increased cellular reaction and infltration by polymorphonuclears and macrophages when compared to the poly-L-Lactic acid-based membrane, which stimulated mainly tire presence of macrophages. The local use (e.q. middle ear) of slow antibiotic release systems could become an important means of delivering drugs ira adequated concentrations for prolonged period of time in otitis media and in a multitude of other otoralyngologic disorders. The results of this study and the ímportance of this new approach will be discussed
![]()
INTRODUCTION
Studies regarding the development of improved options for treating otitis media were initiated in 1980 by one of the authors (MVG). Attempts to develop modified biodegradable membranes into which drugs could be incorporated and be gradually released as the membranes degrade were accomplished1-5. Initial in vivo experiments with poly-L-Lactic acid (PLA) with ampicillin incorporated were success full in treating . Streptococcus Pneumonia-inoculated chinchillas2 and Eustachian tube-obstructed cats5. Both methods have been shown to consistently cause purulent otitis media in these experimental animals6-8. Furthermore, in vitro efficacy to release an antibiotic over time, biocompatibility, and potential cytotoxicity and ototoxicity were evaluated, demonstrating the efficacy and safety of this material2. The use of a collagen-based membrane has been shown to be effective in experimental tympanoplasty1, in treating induced media in cats when ampicillin is incorporated into it , and if further modified, to induce cholesteatoma in experimental animals9. Both membranes have a potential use in other middle ear 4and inner ear, as well as other otolaryngological disorders.
In this report we compare the results of these two membranes; collage/ampicillin and PLA/ampicillin incorporated devices, in treating purulent otitis media in Eustachian tube-obstructed cats.
MATERIAL AND METHODS
Two group of 12 adult cats each weighing 2.5 to 4 kg were used in this study. Animals underwent bilateral Eustachian tube obstruction under pentobarbital anesthesia (30 mg/kg). Sterile technique was used throughout. Through a soft palate incision fine-grade silicone sponges were introduced bilaterally in the tubal orifices to occlude them completely. At the sane procedure one group of animals received a collagen/ampicillin membrane and the other group a PLA/ampicillin membrane in their left middle ears through a posterior bulla approach. The right middle cars of each group were used as untreated controls. Cultures were obtained from nasopharynx and middle ear at the time of the procedure. Each of the two groups was then subdivided in 4 groups of 3 animals each and sacrificed under pentobarbital anesthesia (50 mg/kg) at 1, 2,4, and 12 weeks. Cultures were then obtained at the time of sacrifice from the treated (biodegradable membranes/ampicillin) and untreated (no biodegradable membranes/ampicillin) middle ears (both sides with Eustachian tube obstruction). The animals were decapitated, the temporal bones removed, fixed in 10% buffered formalin, decalcified in 5% triehloroacetic acid, dehydmied through graded series of alcohols, and processed using celloidin methods. From superior to inferior 20u sections were cut in a sliding microtome. Each tenth section was then stained with hematoxylin and eosin. Results in terms of efficacy of treatment and middle ear cultures before and after treatment were compared for both groups of animals.
For comparison of histopathological results and efficacy, a third group of animals were used. These cats underwent Eustachian tube obstruction and received no treatment. These results have been previously reported and show the development of purulent otitis media and subsequent chronification with irreversible tissue changes7-8.
Processing of the membranes and bacterial culture methods have been reported in detail eslsewhere1-3. Details of previous experiments have been reportd for the PLA/ampicillin device in chinchillas2 and cats3, and for the collagen/ampicillin device in cats. Herein, we report only the comparative results.
RESULTS
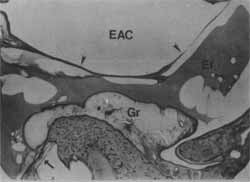
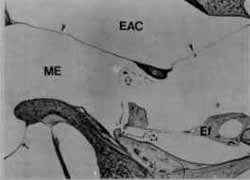
Obstructed untreated cats develop gradual middle ear changes resulting consistently in chronic irreversible otitis media 7,8 (Figures 1 and 2). In the two animal groups treated with ampicillin incorporated membranes, the left middle ears (with the device) showed milder inflammatory changes than untreated animals a early as 1 week post obstruction. By 12 weeks these middle ear cavities had a mild inflammatory reaction or were normal (Figures 3 and 4). The contralateral ears (right ears without the device) of treated animals also showed a milder reaction than the untreated group starting at 2 weeks pos obstruction.
FIGURE 1- Left middle ear of an untreated animal at 4 weeks after the procedure. EAC (external auditory canal), Ef (effusion), Gr (granulation tissue). Tympanic membrane (arrow heads), round window membrane (arrow).
FIGURE 2 - Left middle ear of an untreated animal at 12 weeks after the procedure. EAC (external auditory canal), Ef (effusion), Gr (granulation tissue). Observe numerous cholesterol clefts in effusion. Tympanic membrane (arrow heads), round window membrane (arrow).
FIGURE 3- Left middle ear (ME) with the collagen/ampicillin device (open arrow) at 4 weeks after the procedure. Observe slight inflamatory reaction with some serous effusion (Ef). EAC (external auditory canal), tympanic membrane (arrow heads).
FIGURE 4- Left ear (ME) with the PLA/ ampicillin device (open arrowes) at 12 weeks after the procedure. Observe slight inflamatory reaction. Tympanic membrane (arrow heads), round window membrane (arrow), Ef (serous effusion), EAC (external auditory canal), *(malleus).
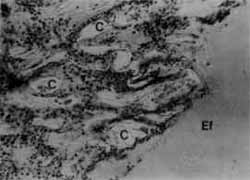
The collagen/based membrane induced a stronger cellular reaction and infiltration by polimorphonuclears and macrophages than the PLA-based membrane, which was not infiltrated and was mainly surrounded by macrophages (Figure 5 and 6). The animals that had the collagen/ampicillin membranes introduced into their middle eats also had more effusion (serous effusion) when compared to the PLA/ampicillin animals at the same stages. It should be mentioned that on top of these slight cellular responses found for both groups of treated animals, no inflamatory reaction in the mucoperiosteum seemed to be caused by the presence of the membranes.
The middle ears cultures obtained at the time of the Eustachian tube obstruction were all negative. The nasopharyngeal cultures obtained at the time of the Eustachian tube obstruction, and the middle ears cultures obtained at the time of sacrifice are shown in tables 1 and 2 for the collagen/ampicillin and PLA/ampicillin groups, respective1y. The cultures obtained at the time of sacrifice from the middle ear cavities with the membranes were negative as early as 1 week for both the PLA/ampicillin and collagen/ampicillin groups. The contralateral middle ears cultures started showing no growth at a later stages (2 weeks). These bacteriological results were similar to the histopathological) changes observed in the middle ears (with and without the membranes/ampicillin) of both groups of treated animals.
FIGURE 5- Collagen-based membrane (C) is infiltrated by numerous cells (polymorphonuclears). Ef (effusion).
FIGURE 6- Poly-L-Lactic acid membrane (P) is seen surrounded by numerous macrophages (arrow heads).
TABLE 1 - Cultures obtained from the nasopharynx at the time of obstruction and obstructed middle ears at the time of sacrifice (2 animals in each subgroup). Collagen/ ampicillin membrane. R (right), L (left).
TABLE 2- Cultures obtained from the nasopharynx at the time of obstruction and obstructed middle ears at the time of sacrifice (2 animals in each subgroup). Poly-L-Lactic acid/ampicillin membrane. R (right) L (left).
DISCUSSION
Eustachian tube obstruction has been shown to consistently cause purulent otitis media in cats, which follows the continuum and progresses toward chronification with irreversible changes in the middle ear cavity7,8. Our results showed that the use of both membranes/ampicillin in Eustachian tube obstructed ears compared extremely favorably to these previously reported animals as early as l week after the procedures. Furthermore, the contralateral ears in the two groups of animals with the antibiotic devices started to compare favorably to these previously reported animals as early as 2 weeks. These results are suggestive that, with the ampicillin incorporated, the PLA-based and collagen-based membranes are able to deliver constant, and suffïcient levels of antibiotic for at least 12 weeks. It is also suggestive that these extended middle ear drug delivery systems are efficient in preventing the chronification of the otitis media in Eustachian tube-obstructed cats. The results obtained for the middle ear cultures at the time of sacrifice corroborate the histopathological fìndings and add evidence for the efficacy of these slow antibiotic release systems.
The use of reconstituted membranes has been recently described as an efficicnt and safe method for delivering sufficient and prolonged concentration of drugs in the middle ear otitis media-induced animals and preventing the chronification of the disease process 2,3,5 Furthermore, these materials have been shown to be biocompatible, biodegradable and not to cause middle ear or inner ear inflamatory reaction 1,3,5. Poly-L-Lactic acid is an organic homopolymer currently used as absorbable sutures in many surgical procedures. Our fïndings are suggestive the cellular reaction involving these membranes is probably responsible for their degradation and the slow release of the antimicrobial. The systemic levels achieved in the two groups of animals were sufficient to avoid chronification of the process even in the contralateral untreated ears. This last observation is by no means applicable as a general rule of what could be achieved in humans. However, the findings observed for the treated ears are by all means extremely suggestive that similar results could possibly be demonstrated in other animals and even in humans. Efficacy of the PLA/amplicillin membrane has been shown to be effective in treating bacterial-induced purulent otitis media in chinchillas2. In this study it was also demonstrated to be more efficient than topical or systemic use of antibiotics in repeated challenges and prophylaxis of otitis media.
The universal use of antibiotics for the treatment of infections has proved effective in numerous occasions worldwide. The overuse and highly empirical dosing considerations of these drugs has prompted the development of some resistant bacteria strains and subsequent inefficacy of the treatment. Controversy still exists over drug selection, dosage, and treatment duration10. In treating otitis media we have to consider not only the acute process but also its tendency for chronification, complications and sequelae. Occasionally, systemic or topical use of drugs do not achieve sufficient concentrations in the middle ear and therefore facilitate the continuum of the disease seen in many cases. Furthermore, topical applications of ear drops or their solvents has been shown to produce severe inflammtory reaction in the middle ear of experimental animals 11,12 and even cholesteatoma formation13-17. Therefore, a safe, practical, and efficient method for delivering antimicrobials and treating otitis media was needed.
The use of antibiotics linked to polystyrene microspheres could be another effective method for safely treating middle ear disorders without the risks of ototoxicity and citotoxicity observe in these experiments. Light and electron microscopy19 studies on the dynamics microspheres in the middle ear mucosa of cats and chinchillas have been performed. Initial results established that the microspheres are inert, and permeability of the middle ear mucosa (including the round window membrane) is selective for size and electric charge20,21. These promising studies suggest that different drugs linked to different sized and charged microspheres could be used selectively to treat middle ear or inner ear disorders.
Both membranes used in this study can incorporate other antimicrobials or drugs and treat a multitude of other pathologies in otolaryngology. Due to smaller and somewhat different cellular reaction, the PLA-based membrane has a wider use in treating inflammatory and infectious processes 2,3. The collagen-based membrane has been shown to stimulate cellular migration and therefore has a wider use in implants and surgical aspects of otology .
Our results showed that both membranes are biocompatible and biodegradable, are able to release antibiotic over time, and are highly effective in treating and preventing the chronification of purulent otitis media. Future experimental use of the PLA-based membrane will include evaluation in different animals, challenge with different antimicrobials and drugs (e.g. steroids and non-steroid ante-inflammatory drugs), antibodies and antigens, and prospective clinical trials in different forms of otitis media and otolaryngological disorders (e.g. chronic sinusites). Future experimental use of the collagen-based membrane will include evaluation of its effectiveness as middle ear prosthesis incorporating antimicrobials and clinical trials of tympanoplasties in humans.
ACKNOWLEDGEMENTS
The authors would like to thank Ms. Noriko Morizono and Sherry Lamey for processing the temporal bones, and, Ms. Carolyn Sheridan for photography and technical support. The support of the FUNEPU, Uberaba, Brasil is also acknowledged.
REFERENCES
1. GOYCOOLEA, M.V.; MUCHOW, D.C.; SCHOLZ, M.T.; SIRVIO, LM.; STYPULKOWSKI, P.H.: In Search of Missing Links in Otology. I. Development of a Collagen-Based Biomaterial. Laryngoscope 101(7):717-726, 1991a.
2. GOYCOOLEA, M.V.; MUCHOW, D.C.; SIRVIO, LM.; WINANDY, RM.: In Search of Missing Links in Otology. II. Development of an Implantable Middle Ear Drug Delivery System: Initial Studies of Sustained Ampicillin Release for the Treatment of Otites Media. Laryngoscope 101(7):727-732,1991b.
3. GOYCOOLEA, M.V.; MUCHOW, D.C.; HUEB, M.M.; RUAH, C.B.: Sustained release of Ampicillin in the middle earusing a reconstituted collagen membrane: An experimental study in the cat. Present at the Fifth International Symposium on Recent Advances in Otites Media. Ft. Lauderdale, May 20-24, 1991 c. In press, proceedings.
4. GOYCOOLEA, M.M.; MUCHOW, D.C.; GOYCOOLEA, H.G.: Otitis Media, 16 Years of Pathogenesis Approach. Otolaryngol Clin North Am 24(4):967-980,1991 d.
5. GOYCOOLEA, M.V.; MUCHOW, D.C.; SIRVIO, LM.; WINANDY, R.M.; CANAFAX, D.; HUEB, M.M.: Extended middle ear drug delivery. A new concept; a new device. In press, Acta Otolaryngol (Stockh), 1991 e.
6. CANAFAX, D.M.; NONOMURA, N.; ERDMANN, G.R; LE, C.T.; JUHN, S.K.; GIEBINK, G.S.: Experimental Animals Models for Studying Antimicrobial Pharmacokinetics in Otites Media. Pharm Research 6(4):279-285, 1989.
7. GOYCOOLEA, M.V.; PAPARELLA, M.M.; CARPENTER, A.M.; JUHN, S.K.: A Longitudinal Study of Cellular Changes in Experimental Otitis Media. Otolaryngol Head Neck Surg 87: 685-700, 1979.
8. GOYCOOLEA, M.V.; PAPARELLA, M.M.; JUHN, S.K.; CARPENTER, A.M.: The cells involved in the middle ear defense system. Ann Otol Rhinol Laryngol 89 (supplem 68):121-128, 1980.
9. HUEB, M.M.; GOYCOOLEA, M.V.; MUCHOW, D.C.; DUVALL, A.J.; PAPARELLA, M.M.; SHERIDAN, C.: In Search of Missing Links in Otology. III. On the Pathogenesis of Acquired Cholesteatoma: Development of a New Animal Model. In press, Laryngoscope.
10. GIEBINK, G.S.; CANAFAX, D.M.: In SC Aronoff, WT Hughes, S Kohl, NT Speck, and ER Wald (eds), Advances in Pediatric Infectious Diseases, Year Book Med Publ Inc, Chicago, Vol. 3: 47-63,1988.
11. PARKER, F.L.; JAMES, G.W.L.: The effects of various antibiotics and antibacterial agents on the middle and inner ear of the guinea pig. J Pharm Pharmacol 30: 236-239, 1978.
12. MORIZONO, T.; PAPARELLA, M.M.; JUHN, S.L.: Ototoxicity of propylene glycol in experimental animals. Am J Otolaryngol 1: 393399, 1980.
13. WRIGHT, C.G.; MEYERHOFF, W.L; BURNS, D.K.: Middle Ear Cholesteattoma: An Animal Model. Am J Otolaryngol 6: 327-341, 1985.
14. HUANG, C.C.; SHI, G.S; YI, Z.X.: Experimental Induction of Middle Ear Cholesteatoma in Rats. Am J Otolaryngol 9:165-172,1988.
15. VASSALI, L.; RARRIS, D.M.; GRADINI, R; APPLEBAUM, E. L.: Propylene Glycol-Induced Cholesteatoma in Chinchilla Middle Ears. Am J Otolaryngol9:180-188,1988.
16. MASAKI, M.; WRIGHT, C.G.; LEE, D.H.; MEYERHOFF, W.L: Experimental Cholesteatoma. Epidermal Ingrowth trought Tympanic Membrane folowing Middle Ear Apllication of Propylene Glycoi. Acta Otolaryngol (Stockh) 108:113-121. 1989.
17. WRIGHT, C.G.; BIRD, LL.; MEYERHOFF, W.L.: Tympanic Membrane Microstructure in Experimental Cholesteatoma. Acta Otolaryngol (Stockh) 111: 101-111, 1991.
18. HUEB, M.M.; GOYCOOLEA, M.V.; RUAH, CR; MUCHOW, D.C.: Dynamics of microspheres in the inflamed middle ear mucosa of the car. Presented an the Fifth International Symposium on Recent Advances in Otites Media. Ft. Lauderdale, Florida, May 20-24, 1991. In press, proceedings.
19. GOYCOOLEA, M.V.; MUCHOW, D.C.; HUEB, M.M.; RUAH, CS.: In Search of Missing Links in Otology. IV. Permeability of the Round Window membrane to Microsphere. An Electron Microscopy Study in Chinchillas. In press, Laryngoscope.
20. GOYCOOLE, M.V.; MUCHOW, D.; SCRACHERN, P.: Experimental Studies on Round Window Structure: Function and Permeability. Laryngoscope, 98(supllem.44):1-20,1988a.
2l. GOYCOOLEA, M.V.; MUCHOW, D.; MARTINEZ, G.C.; AGUILLA, P.B.; GOYCOOLEA, H.G.; GOYCOOLEA, C.V.; SCHACHERN, P.; KNIGHT, W.: Permeability of the Human Round-Window Membrane to Cationic Ferritin. Arch Otol Rhinol Laryngol 114: 12471251,19886.
1 Departamento de Otolaringologia da Universidade de Minnesota, Minneapolis, MN, Estados Unidos.
2 Departamento de Otorrinolaringologia da Faculdade de Medicina do Triângulo Mineiro, Uberaba- MG, Brasil
3 Hospital Santa Lúcia, Uberaba- MG, Brasil
4 Audia Chile
5 Clínica Las Condes, Santiago, Chile
6 Clínica Drs. Ruah, Lisboa, Portugal
O Dr. Hueb é Professor Assistente da FMTM, e staff; Hospital Santa Lúcia, Uberaba-MG; Mestre em Otorrinolaringologia e Pós-Graduando (doutoramento), FMRP-USP, SP; e "Instructor" no Departamento de Otorrinolaringologiada Universidade de Minnestosa, Minneapolis, MN, Estados Unidos.
Este estudo foi apoiado em parte pela 3M Minnestosa, pela verba 8P50-DC-00133 "National Institute Of Deafness and Other Conemunicative Disorders", Estados Unidos, e Audia Chile, Santiago, Chile.
Endereço para Correspondência: Dr. Marcelo M. Hueb, Hospital Santa Lúcia Av. Santos Dumont, 409 - 38010- Uberaba- MG, Brasil