Year: 2000 Vol. 66 Ed. 6 - (7º)
Artigos Originais
Pages: 620 to 625
Vocal Rehabilitation of Laryngecomized. A new Endoscopic Technique for Secondary Restoration with Vocal Prosthesis.
Author(s):
Claudiney C. Costa*,
José F. S. Chagas**,
Pedro C. Neto****,
José L. B. Aquino***,
José G. T. Camargo***,
Maria B. N. Pascoal*,
Iára Bittante de Oliveira*****.
Keywords: laryngectomy, voice rehabilitation, prosthesis
Abstract:
Introduction: The first total laryngectomy dates of 1873 described by Billroth, and it was accompanied by the attempt of vocal rehabilitation with the Gussenbauer's external prosthesis of . In the last years the forms of vocal rehabilitation developed and the use of the tracheo esophageal fistula with a valvuled prosthesis was proposed by Blom and Singer in 198012. The placement of the prosthesis after laryngectomy is denominated secondary, and in spite of the evolutions regarding the vocal prosthesis the secondary placement using general anesthesia and rigid esophagoscopy stays as proposed by Blom and Singer in 1980, taking the complications as mediastinite, cervical cellulite, fracture of cervical vertebra, and esophageal perforation. Material and Methods: This work was accomplished in five patient submitted to total laryngectomy and rehabilitated with vocal prosthesis Blom-Singer Indwelling low pressure with secondary placement through new surgical technique by digestive endoscopy and mitigation with midazolan, in the period of June to July of 1999, releasing this way the use of general anesthesia and hospitalization. Results: All patients were rehabilitated with tracheoesophageal prosthesis, without complications related with the surgical technique. Conclusion: The advantages of this new technique in relation to the conventional are: l) releases the general anesthesia; 2) it is not necessary patient hospitalization; 3) simple material and low cost for the placement of the prosthesis; 4) smaller risks of complications, as: high digestive hemorrhage; mediastinite; fracture of cervical vertebras; esophageal perforation; 5) smaller trauma of the esophageal mucosa; 6) direct visualization of the positioning of the prosthesis in the esophagus.
![]()
INTRODUCTION
The importance of larynx as one of the key players of voice formation and breathing has been described before the Christian era. The first description of laryngeal cancer has been attributed to Arekaus, about 100 AD14.
Laryngeal cancer not only threatens life, but also brings severe consequences to patients' well being, because it is closely related with one of the essential functions of social and interpersonal relationships - the voice.
The first total laryngectomy dates back to 1873. It was conducted by Billroth and presented by his assistant Carl Gussenbauer, in the Third Congress of Surgeons in Germany, under the title "The first laryngectomy conducted in humans by Theodore Billroth- and the use of Artificial Larynx". Therefore, the first laryngectomy and the attempt of vocal rehabilitation happened simultaneously5.
Malignant laryngeal tumors have high incidences in Brazil, and it is the 6th most common site of malignant tumors in male patients (Ministerio da Saúde-1981/1984), with 2,300 deaths recorded in 1996 (INCA). In 1999, according to the American Cancer Society (INCA-2000), 10,600 new cases of laryngeal and hypopharyngeal cancer were recorded in the Unites States, with 4,200 deaths8.
Despite development of new diagnostic methods and conservative surgical techniques of partial laryngectomy, total laryngectomy is still used all over the world for advanced and early tumors, because it provides excellent survival rates. Natural sequela includes loss of voice, reduction of physical resistance, reduction of sense of olfaction and taste and loss of self-esteem, with secondary depression10.
Vocal rehabilitation until the 80's was conducted with electro-electronic devices and development of esophageal voice - techniques that are still used nowadays. Tracheoesophageal punctures, initially used in the 50's, were no longer used because of technical difficulties in making them and the high incidence of aspiration1.
Singer and Blom, in 1980, presented a new vocal rehabilitation technique in patients submitted to total laryngectomy, consisting of a tracheoesophageal puncture in which a prosthesis was introduced, enabling the unidirectional passage of expired air from the trachea into cervical esophagus, barring the passage of food from the esophagus into the trachea. In this first study, they evaluated 60 patients with vocal rehabilitation index of 90%. The first prosthesis was made of silicone, was removable and had to be cleaned once a day and replaced by the patient. Initial durability of these prostheses was about 3 months5.
In recent years, modifications to these prostheses have been introduced in order to make them more resistant to infections, enhance durability, reduce the manipulation by the patient and exclude the possibility of a reaction to foreign body; however, for secondary placement, the patient still has to be submitted to general anesthesia.
We developed a technique for secondary placement vocal prosthesis using esophagogastroduodenoscopy (EGD), eliminating the need for hospitalization and the use of general anesthesia, as well as the risk of complications related with the surgical technique of secondary placement of prostheses.
In this study, the choice of Blom-Singer prosthes (Inhealth, International Healthcare Technologies, CA) w; based on some characteristics: easy manipulation by patient valve with low resistance to respiratory flow (3-5mmH20)9, providing less effortful and more fluent speech, easy substitution in the office, and low cost.
Therefore, this study aimed at describing a new method of secondary placement of vocal prostheses type Blom Sing through EGD, without general anesthesia and avoiding interference of possible post-op complications. In addition, we evaluated efficacy and rate of complications.
MATERIAL AND METHOD
This study was performed in 5 patients who had epidermoid laryngeal or hypopharyngeal cancer, submitted to tot laryngectomy or pharyngolaryngectomy, with or without neck dissection, and placement of vocal prosthesis f esophagogastrosduodenoscopy (EGD) between June and July 1999. All patients were treated at the Service of Head and Neck Surgery at Hospital a Maternidade Celso Pierro (HMCP), Pontifícia Universidade Católica de Campinas (PUCCAMP), Sao Paulo. V6 placed vocal tracheoesophageal prosthesis brand Blom-Singer® Indwelling Low Pressure Voice Prosthesis 14 mm, between June and July 1999, after presentation of advantages an disadvantages of the different rehabilitation approaches. The, patients were followed-up by the team of speech pathologies and physicians of the Service of Head and Neck Surgery; HMCP, PUCCAMP.
All patients were men, aged between 40 and 75 year mean age of 57 years and median of 54 years. In two patient radiotherapy was conducted after surgery. The surgical procedures used were: simple total laryngectomy in one patient, tots pharyngolaryngectomy with unilateral neck dissection in patients, total pharyngolaryngectomy with bilateral neck dissection in 2 patients. The prosthesis was placed in the 5 patients, after surgical treatment of primary lesion, called secondary placement, using the new technique with EGD.
In the present study, patients had low social and eccnomic backgrounds, two of them were illiterate and 3 had not finished primary school, and they had all unsuccessfully tried t learn esophageal voice.
Patients signed the informed consent after hearing all information concerning cost of prosthesis, other vocal rehabilitation techniques (esophageal voice, artificial larynx), and advantages and disadvantages of tracheoesophageal prosthesis.
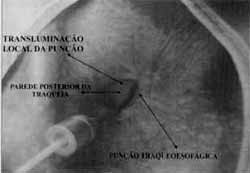
Figure 1. Place of tracheoesophageal puncture identified by transillumination (endoscope light).
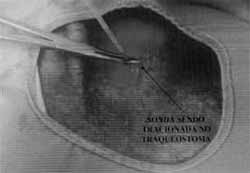
Figure 2. Needle identified in esophageal lumen, and the thread was pulled towards the oral cavity (endoscopic visualization).
The choice of vocal rehabilitation approach was made by the patient after a detailed explanation of all methods. The candidates for rehabilitation with tracheoesophageal prosthesis had to meet the following criteria: motivation; understand anatomy and functioning of prosthesis; manual dexterity to maintain the prosthesis and occlusion of tracheostome; absence of stenosis on the tracheostome; tracheostome diameter that could be occluded with the thumb; absence of pulmonary debilitating diseases; absence of mental illness and significant stenosis of hypopharynx (Foundation of Voice Restoration Following Total Laryngectomy, nor P. C. Doyle, San Diego)10. In addition, patients also had to afford the tracheoesophageal prosthesis.
The new technique consisted of secondary placement of vocal prosthesis using EGD as the visualization aid, conducted with videogastroendoscope Fujinon Eve Series 400, and monitor Sony Triniton Color. Patients were sedated with 5mg of endovenous midazolan; next, we introduced the endoscope through the esophagus until identification by transillumination of the exact point of puncture on the posterior wall of the tracheostome (Figure 1).
Using a needle of 2.1mm in diameter by 5.1 cm in length, we conducted a puncture of the posterior wall of the trachea, guided by endoscopic light, at 0.5cm from the upper border of the tracheostome, until the bevel perforated the anterior wall of the esophagus, checked by the monitor connected to the endoscope (Figure 2).
Once we identified the needle into the esophageal lumen, we passed a 1.7mm by 30.5cm long catheter through the lumen of the needle, pulling it towards the oral cavity using an endoscopic biopsy clamp and guided through the monitor (Figure 2). When the catheter was in the oral cavity, we proceeded with the fixation of the nelaton probe number 12, and on the other side, we fixed the vocal prosthesis with zero cotton thread.
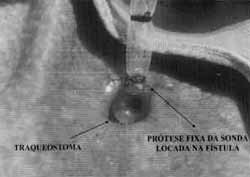
The probe was pulled from the oral cavity to the tracheostome (Figure 3), until it was properly placed in the tracheoesophageal puncture (Figures 4 and 5).
Patients were encouraged to speak in the endoscopy room, and were discharged after they had recovered from the sedation with midazolan, approximately 30 minutes later, and they were followed up by the Service of Headead and Neck Surgery at PUCCAMP one week after the placement of vocal prosthesis. In addition, patients came once a month, in the 3 first months, and later once every three months, to evaluate complications of placement and use of vocal prosthesis. Patients were instructed to seek our medical assistance if there was any event resultant from the use of the -prosthesis.
RESULTS
All patients had vocal restoration immediately after the placement of the prosthesis and we did not observe any complication regarding the used technique.
DISCUSSION
Total laryngectomy has a massive impact in the life of patients. Loss of larynx results in abrupt rupture with verbal communication and interaction with other people, resulting in significant changes in the social, economic, family and psychological life of the laryngectomee3.
Figure 3. Prosthesis fixed to nelaton probe and pulled on the posterior tracheal wall.
Esophageal voice is currently the most widely used method in the services that deal with vocal rehabilitation after total laryngectomy, either because of low cost or because it is not necessary to use prostheses or any other electronic devices. The disadvantage is that the procedure has high failure rates, varying from 10% (Hunt, 1964) to 60% or more (Martin, 1963; Robbins, 1984), and the long period it takes to learn it, which may vary from 4 months to one year11.
The introduction of valve tracheoesophageal prostheses as a method of vocal rehabilitation of laryngectomized patients promoted a drastic change in the therapeutic area of restoration of a laryngeal voice. The advantages of vocal rehabilitation using tracheoesophageal prostheses are: no compromise of oncologic surgical principles, compatibility with patients submitted to radiotherapy12, high success rates, short learning period, vocal quality superior to other forms of rehabilitation, use of lungs as the source of air for phonation, increasing maximum phonation time, making sentences longer and closer to those produced by laryngeal voice, and intensity of voice higher than with other rehabilitation methods1.
Disadvantages of vocal rehabilitation using prosthesis are: cost of prosthesis, need for follow-up with surgeon to maintain and replace the prosthesis, need to use one hand to occlude the tracheostome13.
One of the decisive factors in the choice of tracheoesophageal prosthesis was low cost of prosthesis, compared to the other types available in Brazil.
Figure 4. Prosthesis placed in tracheoesophageal puncture(external visualization).
Figure 5. Prosthesis placed in the esophagus (endoscopic visualization).
Initially, tracheoesophageal prostheses were in secondarily to laryngectomy in patients who did not esophageal voice. Thanks to the high success rates with secondary placement of prostheses, and various series that showed rehabilitation of 80 to 90% of the cases12, many modifications in the placement techniques were developed. One of them is the placement of the prosthesis together laryngectomy, the so-called primary placement, conducted for the first time in 1982 by Maves and Lingeman9. The authors reported 11 cases of patients submitted to total laryngectomy and placement of Blom-Singer or Panje prostheses in the operation, called primary puncture, and they obtain rehabilitation in 10 patients: The advantages of primary puncture are: 1) respect oncologic principles, because it enables resection of tumor with safety margins; 2) appropriate closure of pharynx, preventing aspiration; 3) elimination of the use of postoperative nasogastric tube; 4) there is no need for a second surgical intervention; 5) positive psychological effect, because vocal rehabilitation starts early4.
Hilgers and Schouwenburg7, in 1990, studied 79 patients submitted to placement of a new prosthesis developed by them, the Provox®, which did not require removal and presented low in vitro pressure, about 3 to 5mmH20, similar to the values of low pressure prostheses of Blom-Singer. The authors reached success rates of 91% (66 patients). However, the technique of secondary placement was maintained, because the patients had to undergo general anesthesia.
Since 1982, many modifications concerning prostheses and their accessories were made; however, none of them affected secondary placement, which, regardless of type, always required general anesthesia.
In primary placement of vocal prosthesis, it is positioned in the tracheoesophageal puncture concomitantly with the procedure of laryngectomy. Secondary placement consists in the introduction of the vocal prosthesis at a second surgical act, that is to say, after laryngectomy:
Gluckman, Silver and Donegan (1985)6 studied the complications of tracheoesophageal puncture in 47 patients. They found a rate of complications of 15%, including: mediastinitis in 3 patients, cervical cellulite in 3, and cervical vertebra fracture in one case. The authors concluded that simplicity and effectiveness of secondary puncture were superior to other surgeries directed to vocal rehabilitation, although similarly to all surgical procedures, the technique is associated with a significant number of complications.
In our Service, secondary placement was conducted under general anesthesia and rigid esophagoscope, according to the principles dictated by Blom and Singer in 1980. Patients underwent pre-op assessment and were hospitalized 24 hours before the procedure, followed by 8-hour fast. After the surgery, they were discharged 72 hours later, if the surgical procedure had been uneventful. Complications such as infection of puncture site and high digestive hemorrhage because of rupture of esophageal varices during insertion of rigid endoscope have already been reported.
In our series, we did not observe any complication related to the technique of secondary placement by EGD, and all patients had immediate restoration of voice.
The placement of vocal prosthesis using EGD proved to be feasible and the mean duration of placement was 15 minutes. As a result of the advantages noted, this new technique is a procedure that promotes more comfort to patients and more safety to surgeon.
CONCLUSION
This technique for secondary placement of vocal prosthesis proved to be feasible and there were no complications resultant from its performance.
The advantages as compared to conventional secondary placement are:
1. Does not require general anesthesia.
2. The patient is not hospitalized.
3. Simple and low cost material is used to place the prosthesis.
4. Lower risk of complications, such as high digestive hemorrhage, mediastinitis; cervical vertebra fracture, esophageal perforation.
5. Less trauma of oropharyngeal and esophageal mucosa.
6. Direct visualization of positioning of prosthesis in the esophagus.
REFERENCES
1. BLOM, E. D. -In BLOM, E. D.; SINGER, M. I.; HAMAKER, R. C. -Tracheoesophageal Voice Restoration Following Total Laryngectomy, San Diego, Singular Publishing Group, 1998, 0108.
2. BUSSCHER, H. J.; MEI, H. C. In BLOM; E. D.; SINGER, M. I.; HAMAKER, R. C. -Tracheoesophageal Voice Restoration Following Total Laryngectomy, San Diego, Singular Publishing Group, 1998, 89-102.
3. DEDIVITIS, R. A.; GUIMARAES, A. V.; HUSHI, G. D.; FUZA, K. R. - Qualidade de vida do paciente laringectomizado. Rev. Bras. de Otorrinolaringol., 66(1): 14-17, 2000.
4. FUKUTAKE, T.; YAMASHITA, T. - Speech rehabilitation and complications of primary tracheoesophageal puncture. Acta Otolaryngol (Stockh), Suppl. 500: 117-120, 1993.
5. GLUCKMAN. J. L.; FARREL M. L.; KELLY D. H. -IN CUMMINGS C. W.; FREDRICKSON, J. M.; HARKER, L. A.; KRAUSE; C. J.; RICHARDSON, M. A.; SCHULLER, D. E. Otolaryngology Head & Neck Surgery, third edition, St. Louis, Mosby, 1998, 2285-2298.
6. GLUCKMAN, J. F.; SILVER, F. M.; DONEGAN, J. O. - Operative complications of tracheoesophageal puncture. Laryngoscope, 95: 1360-1362, 1985.
7. HILGERS, F. J. M.; SCHOUWENBURG, P. F. - A new low-resistance, self-retaining prosthesis (Provox TM) for voice rehabilitation after totallaryngectomy. Laryngoscope, 100.12021207, 1990.
8. INCa - Instituto Nacional de Cancer; Ministerio da Saude - DATASUS;ACS - American Cancer Society. "Incidência e Mortalidade por Câncer Brasil EUA-Hospital do Câncer - AC Camargo.htm." 2000.
9. MAVES, M. D. & LINGEMAN, R. E. - Primary vocal rehabilitation using the Blom-Singer and Panje voice prostheses. Ann. Otol. Rhinol. Laryngol., 91: 458-460, 1982.
10. PERRY, A. -In BLOM, E. D.; SINGER, M. I.; HAMAKER, R. C. - Tracheoesophageal Voice Restoration Following Total Laryngectomy, San Diego, Singular Publishing Group, 1998, 09-18.
11. SIMPSON, C. B.; POSTMA, G. N.; STONE, R. E.; OSSOF, R. H. - Speech outcomes after laryngeal cancer management. Otolaryngol. Clin. North Am., 30(2): 189-205, 1997.
12. SINGER, M. I. & BLOM, E. D. - New endoscopic technique for restoration of voice after laryngectomy. Ann. Otol., 89. 529-533, 1980.
13. STAFFIERE, M.; STAFFIERI, A. - A new voice b post-total laryngectomy speech rehabilitation. Laryr 98: 1027-1029, 1988.
14. THAWLEY, S. E. -THAWLEY, S. E.; PANJE, W. R.; B. J. H.; LINDBERG, R. D. - Comprehensive managemey and neck tumors, second edition, Philadelphia, W.B.; Company, 1999, 979-1005.
* Otorhinolaryngologist and Intern of the Service of Head and Neck Surgery at Pontifícia Universidade Católica de Campinas - PUC - Campinas /SP.
** Head of the Service of Head and Neck Surgery at Pontifícia Universidade Católica de Campinas - PUC - Campinas /SP.
*** Assistant Physician of the Service of Head and Neck Surgery at Pontifícia Universidade Cat6lica de Campinas - PUC - Campinas /SP.
**** Assistant Physician of the Service of Endoscopy at Pontifícia Universidade Católica de Campinas - PUC - Campinas /SP.
***** Speech and Hearing Pathologist at PUC - Campinas /SP.
Affiliation: Service of Head and Neck Surgery of Hospital a Maternidade Celso Pierro da Pontifícia Universidade Católica de Campinas.
Address for correspondence: Claudiney Candido Costa - Rua Ant6nio Rodrigues Moreira Neto, 106, Apto i l - Jardim Pauliceia - 13060-063 Campinas /SP.
Tel: (5519) 227-5377 - E-mail: claudineyorl@ig.com.br
Article submitted on July 28, 2000. Article accepted on September 28, 2000.