Year: 2000 Vol. 66 Ed. 5 - (19º)
Relato de Casos
Pages: 547 to 550
Lateral Canthotomy: Simple Treatment for a Serious Complication of Micro-Endoscopic Sinus Surgery.
Author(s):
Roberto E. S. Guimarães*,
Celso G. Becker*,
Helena M. G. Becker**,
Cleiton D. L. Silva***,
Daniel V. Abreu***,
Cícero A. F. Júnior***.
Keywords: functional endoscopic sinus surgery; orbital complications; orbital decompression; lateral canthotomy
Abstract:
Micro-endoscopic sinus surgery can result in both minor and major complications. Orbital complications - including orbital hematoma and orbital enphysema - are, among these, the most feared. A case of orbital enphysema successfully treated by lateral canthotomy is presented. The pathogenesis-of these potencially serious complications are discussed. A sequencial treatment algorithm is presented. This case demonstrate that lateral canthotomy constitutes a safe and fast surgical procedure to decrease intra-orbital pressure.
![]()
INTRODUCTION
Micro-endoscopic surgery of paranasal sinuses has become very important for surgical treatment of chronic sinus pathologies. Its acceptance is a result of the pioneer work conducted by Professors Messerklinger, from Austria, and Wigand, from Germany. Endoscopic access was later popularized by Stamberger, in Europe and Kennedy, in the United States. The success of the technique encouraged its use by less experienced surgeons. Some of them had to face very high complication rates.
Among complications, orbital ones are extremely severe and they may include damage to extra-ocular muscles, orbital emphysema, orbital hemorrhage, damage to nasal-lachrymal duct, and direct damage of optic nerve.
In the present article we discuss a safe, easy and efficient technique to decompress the orbit: lateral canthotomy. We also present a treatment algorithm to orbital hematoma, as well as report the efficiency of the employed technique in a case of orbital emphysema.
CASE REPORT
MEM, 24-year-old male patient, melanodermic, with extensive nasal sinusal polyposis. He was admitted in hospital to undergo nasal sinusal micro-endoscopic surgery. We conducted bilateral maxillary antrostomy, bilateral sphenoid sinusotomy and bilateral partial ethmoidectomy. During right anterior ethmoidectomy, there was an accidental rupture of papyrace, lamina, exposing orbital fat. We conducted anterior packing, with glove finger and gauze.
One hour after the surgery, it quickly progressed to right proptosis and limitation of ocular mobility; the patient was then submitted immediately to lateral canthotomy under sedation and local anesthesia with Xylocaine 2% and vasoconstrictor. After the procedure, there was a major release of air from the orbit, with regression of proptosis.
Two hours after lateral canthotomy, the patient was submitted to orbit CT Scan that showed a small quantity of air medially and laterally to the ocular globe. However, there were no signs of impairment of retrobulbar fat or optic nerve, without signs of hematoma. There was no impairment of visual acuity and ocular mobility. At immediate post-operative period, the patient presented conjunctive ecchymosis and palpebral edema.
Three months after the procedure, the patient has no sinusal or orbital symptoms, and no functional sequelae.
Figure 1. CT scan of orbit at axial section conducted 2 hours after lateral canthotomy, showing residual orbital emphysema.
DISCUSSION
Orbital anatomy has areas potentially dangerous forsurgeons. The risk is even greater if factors such as hypertension, dehiscence of lamina papyracea, extensive polyposis, previous surgery, inability to visualize maxillary ostium and chronic use of steroids are present. Risk structures include lamilta papyracea, nasal-lachrymal duct, anterior and posterior ethmoid arteries, orbital fat, medial rectus and superior oblique muscles and optic nerve1,3,4.
Literature review from 1980 to 1999 revealed few reports about orbital complications secondary to micro-endoscopic sinus surgery3,4,6. The largest series (8,000 patients) reported by Stammberger and Hawke did not observe orbital complications. However, higher incidences were reported in smaller series: among them, Stankiewicz (1989) observed 5 orbital hemorrhages in 300 patients. Levine (1990), in turn, described 3 orbital hemorrhages among 250 patients. Vleming et al. (1992), in 592 patients, found 2 orbital hemorrhages and one lesion of nasal-lachrymal duct.
Among orbital complications, hemorrhage is the most frequently observed affection6,5. It may be determined by accidental damage to anterior and posterior ethmoid arteries, with retraction to the interior of orbit, lesion of papyracea lamina with high-pressure blood inflow coming from the nasal fossa.
Clinical signs of orbital hemorrhage/hematoma are: proptosis, chemosis, edema, limitation of ocular mobility and mydriasis. These signs may surge abruptly, in the peri-operative situation, or slowly, within 48 hours1,3,2. There may be reduction of visual acuity, followed by loss of pupilar reactivity and consensual pupilar reflex3. Such an event occurs because orbital cavity has rigid limits and increase of contents (hemorrhage) causes compression of orbital structures and consequently, proptosis.
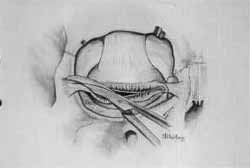
Figures 2 and 3. Orbital anatomy showing lateral canthal ligament and lateral canthotomy technique.
He pathophysiological mechanism that determines visual loss is not fully understood yet, but it is probably due to direct pressure over the optic nerve by the hematoma, supplementing arterial pressure for perfusion of soft tissues, such as optic nerve and retina3. Since they do not tolerate ischemia for more than 2-3 hours, diagnosis and treatment should be quick3,2. Therefore, the problem results from increase of contents (blood or air) inside a fixed cavity (the orbit), leading to increase of intra-orbital pressure. As a consequence, treatment should focus on draining the hematoma or expanding orbital volume.
Lateral canthotomy and inferior cantholysis are advocated as the fastest and safest ways of performing anterior expansion of orbital globe of 4-5mm, reducing intra-orbital pressure3,2,7.
Technique: canthotomy is conducted by introducing one the blades of a pair of scissors on the lateral extremity of the orbit, sectioning the lateral canthal ligament and the underlying skin. If it is not enough, we may perform an inferior cantholysis, which is the inferior extension of the incision sectioning the insertion of lateral canthal ligament3,2,6,7.
This simple procedure is frequently the only one necessary to reduce intra-orbital pressure; however, if it does not suffice, we mayconduct an orbital decompression via external or endonasal ethmoidectomy1,3.
In case of orbital hemorrhage, some authors suggested that as an initial measure we could use manitol, acetazolamide and dexametasone in high doses. After that, visual acuity, mobility and ocular tension are observed for a period of 90 minutes, and then, if they fail, surgical treatment will be conducted3. However, these measures do not treat the primary physiological mechanism - the increased intra-orbital pressure because of hemorrhage. Therefore, in our opinion, lateral canthotomy should be the initial step for orbital decompression once proptosis is recognized, because we might waste time performing clinical measures.
The following algorithm is suggested for management of intra-orbital hemorrhage:
1. Observe closely the eyes during surgical procedure, detecting signs such as proptosis, ecchymosis, mydriasis, and increase of ocular tension;
2. Avoid nasal packing after exposure of orbital fat (what may precipitate orbital hematoma - we should try local measures to control bleeding, such as use of vasoconstrictors, cautery and local hemostatic agents, gelfoam, for example);
3. Once proptosis is recognized:
o Remove packing;
o Conduct lateral canthotomy / inferior cantholysis
Once the visual acuity is stable, proptosis is reduced and mobility is preserved: ? CT scan / MRI + careful observation.
If there is persistence or increase of proptosis and /or visual deterioration ? orbital decompression.
Post-operatively, the support of an ophthalmologist is essential in order to reduce post-surgical morbidity.
CONCLUSION
Orbital hemorrhages or emphysemas are rare but severe complications of micro-endoscopic sinus surgery. Knowledge of anatomy and physiology of the process enables the surgeon to recognize complications. Lateral canthotomy is a quick, safe and simple way of providing orbital decompression, in order to minimize permanent sequelae.
REFERENCES
1. COREY, J. P. - Orbital complications in functional endoscopic sinus surgery. Otolaryngol Head Neck Surg., 109: 814-20, 1993.
2. PELAUSA, E. O. - Orbital complications of functional sinus surgery. J. Otolaryngol., 24: 154-59, 1995
3. SAUSSEZ, S. - Lateral canthotomy: a simple and safe procedure for orbital haemorrhage secondary to endoscopic sinus surgery. Rhinology, 36: 37-39, 1998
4. STAMMBERGER, H. (1991) - Special endoscopic anatomy of the lateral nasal wall and ethmoidal tissues. In: H Stammberger (Ed). Functional endoscopic sinus surgery. The Messerklinger technique. B.C. Decker, Philadelphia pp. 49-88
5. STAMMBERGER, H. (1993) - Postoperative problems and complications. In: H. Stammberger, M. Hawke (Eds.) Essentials of endoscopic sinus surgery. Mosby Year Books, St Louis pp. 199-208
6. THOMPSON, R. F. - Orbital haemorrhage during ethmoid sinus surgery. Otolaryngol. Head Neck Surg., 102: 45-50, 1990.
7. YUNG, C. - Efficacy of lateral canthotomy and cantholysis in orbital haemorrhage. Ophthalmic. Plast. Reconstr. Surg., 10: 137-41, 1994.
* Assistant Professor of the Department of Otorhinolaryngology at Hospital das Clínicas da FM-UFMG.
** Teaching Auxiliary Professor of the Department of Otorhinolaryngology at Hospital das Clínicas da FM-UFMG.
*** Resident Physician of the Service of Otorhinolaryngology at Hospital das Clínicas da FM-UFMG.
Study conducted by the Service of Otorhinolaryngology at Hospital das Clínicas da FM-UFMG.
Study presented at 1° Congresso Triológico de Otorrinolaringologia, held on November 13 - 18, 1999, in São Paulo/ SP.
Address for correspondence: Dr. Roberto E. S. Guimarães - Rua Levindo Lopes, 191 - Savassi - 30140-170 Belo Horizonte/ MG - Tel/Fax: (55 31) 281-4604
Article submitted on November 12, 1999. Article accepted on December 16, 1999.