Year: 2000 Vol. 66 Ed. 5 - (18º)
Relato de Casos
Pages: 541 to 544
Tumefactive Fibroinflammatory Lesion of the Cervical Region in a Child - Case Report.
Author(s):
Marcus A. Lima*,
Luís C. Carmo**,
Juliana B Cunha**,
Patrícia M. Pinheiro**,
Fernando A. Pimenta***.
Keywords: tumefactive fibroinflammatory lesion, pseudoneoplasia, neck, child
Abstract:
Tumefactive fibroinflammatory lesion (TFL) is a rare idiopathic fibrosclerosing disorder, which resembles a malignant invasive process, but is histologically benign, ranging in age from 10 to 71 years. This report describes a case of TFL in cervical region in a six-year-old girl, roughly characterized by a white to graytan firm mass, with a homogenous texture simulating neoplasia. Microscopically, it was represented by a proliferating fibrous tissue with lymphocytes and polymorfonuclear leukocytes. This appearance is similar to that seen in other idiopathic fibrosing syndromes, such as Riedel's thyroiditis, sclerosing cholangitis, retroperitoneal fibrosis and orbital pseudotumor. Mostly in children, the TFL can simulate neoplasias like sarcomas. It also has diverse therapies and a high local recurrence rate, which makes the clinical management of these patients difficult. The patient of this case evolved well, without signs of recurrence.
![]()
INTRODUCTION
Although not very common, pseudo-neoplasic proliferation' of the head and neck have attracted the attention not only because of the possibility of simulating a neoplasia, but also because they have high recurrence potential and association with other diseases10. Among this kind of proliferation, we may list fibromatosis, nodular fasciitis, and proliferative myosistis10, because they are more frequent and sometimes they manifest a clinical malignant presentation, leading to confusion with sarcoma. Recently, a new entity was described and it has become a frequent topic of discussion - tumefactive fibroinflammatory lesion (TFL) of the head and neck4,5,6,8,10.
The term tumefactive fibroinflammatory lesion was used for the first time in 1983 by Wold and Welland6,8 to describe a fibrosclerosing disorder, presenting malignant clinical manifestation but histologically benign, affecting subjects between the ages of 10 and-71 years, with highest incidence between the 5th and 6th decades of life, and installing on the head and neck regions5. This lesion is part of a group of diseases that share similar histopathology, such as Riedel's thyroiditis, retroperitoneal and mediastinis fibrosis, sclerosing cholangitis, and orbit pseudotumor4,7,10. Its etiology is still obscure, generating therapeutic controversy that varies from the use of high doses of corticosteroids to surgery and radiotherapy.
We recently serviced a case of neck TFL in a 6-year-old child with clinical diagnosis of sarcoma of cervical soft parts. We decided to publish it because of its rarity and in order to attract the attention of surgeons for the possibility of a lesion that clinically simulates a malignant neoplasia.
CASE REPORT
Six-year-old girl, Caucasian, with history of a mass on the posterior triangle of left lateral region of the neck for 30 days, growing progressively, which was not painful but associated with generalized lymph node pathology and fever. Ten days before, she had had purulent tonsillitis treated with crystal penicillin, with good progression of case. At the physical exam, we observed a firm non-depressible mass, measuring 4.0 x 2.5cm, painful upon palpation, with little mobility and adhered to deeper plans. Lab tests: total blood count: leukocytosis, increase in segmented, monocytosis and high hemosedimentation rate; serology for cytomegalovirus, rubella and mononucleosis non-suggestive of acute infection; urinalysis without alterations. Chest x-ray was normal; abdominal and pelvic ultrasounds were normal, and cervical ultrasound showed enlargement of lateral left region and lymph nodes with increased volume located on inferior and superior carotid chains bilaterally, cervical posterior to the left and submandibular to the right, between 0.8 and 2.1 cm in diameter.
Anatomic pathological exam
Macroscopy
Oval-shaped nodular structure weighting 5g and measuring 3 x 2 x 2 cm, presenting external surface slightly lobulated, pink-yellowish color, of elastic consistency. The cut surface demonstrated tissue of striated aspect, white-gray bright color, soft consistency, containing an oval-shaped nodule measuring 1.1 x 0.6 x 0.6 cm, of gray color, soft consistency and lymph node aspect.
Microscopy
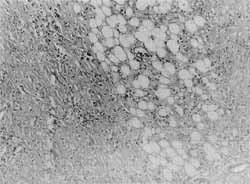
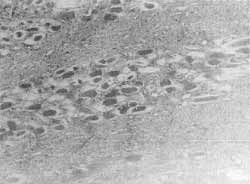
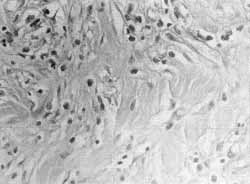
Fibromuscular tissue presenting intense inflammatory infiltrate consisting of lymphocytes, plasmacytes, and eosinophils close to the diffuse fibroblastic proliferation without atypias (Figure 1), with necrosis of fat and intense deposits of collagen that permeated and caused atrophy of muscle fibers (Figure 2). In a detailed area of the inflammatory process, inflammatory cells permeated the fibrous collagenic connective tissue (Figure 3). There were no mitosis figures. Among the process, we noticed lymph node with reactive follicular hyperplasia.
Diagnosis: Product of exeresis of "left cervical region tumor": tumefactive fibroinflammatory lesion of the neck.
After the surgery, we did not prescribe specific medication and the patient was clinically followed-up for 20 weeks without signs of recurrence, based on CT Scan. She complained about reduced sensitivity of a small portion of the earlobe of the left auricular pinna.
DISCUSSION
This was the report of a case of TFL affecting a 6-yearold child. The diagnosis was based on clinical findings and results of histopathological analysis conducted on the material collected from open excision biopsy3. Macroscopically, TFL are firm, white-gray masses, of homogenous texture, and histoiogically they present fibrous connective tissue permeated with fibroblastic proliferation, lymphocytes and polymorphonuclear10, compatible with the presentation observed in the present case and shown in Figures 1, 2 -and 3. Sinusal tract is the most frequently affected region by TFL, followed by cervical lesion, topography of our case, and parotid glands5. The less frequent affected regions are mandible, tongue and face. There are very rare reports of lesions that affected areas not on the head and neck.
The age of presentation of the 23 cases reported in the literature ranged from 10 to 71 years, and in most of the patients the lesion was diagnosed during the 5th and 6th decades of life5. The present case report presents a younger patient, a 6-year old girl, the youngest patient of TFL ever reported, because the literature presents 3 cases of subjects younger than 16 years but older than 10 years of age1,3,8.
Figure 1. Intense inflammatory infiltrate close to the diffuse fibroblastic proliferation involving fatty tissue (HE, 100x).
Figure 2. Fibrous collagenic connective tissue permeating and causing atrophy of skeletal muscle fibers (HE, 100x).
Figure 3. Detail of fibroinflammatory process showing fibrous collagenic connective tissue, permeated by lymphocytes, plasmacytes, and eosinophils (HE, 400x).
Despite the fact of being histologically benign, TFL may have a malignant clinical presentation, with fast growth, invasion of adjacent structures, and sometimes non-respondent to medication and/or surgical treatment4,6,8,9,10. However, if affecting younger subjects, especially children, they may simulate clinically important neoplasias that have very negative prognosis, such as high degree lymphoma, rhabdomyosarcoma, Ewing sarcoma, neuroblastoma, osteogenic sarcoma, synovial sarcoma, and hemangiopericytoma, among others2,11. For this reason, surgeohs must be aware and consider the hypothesis of tumefactive fibroinflammatory lesion before submitting young patients to radical treatments. In many occasions, excision surgery3,5,9, associated or not with continuous use of 10 to 20mg prednisone per day for a long period of time 4, may solve most of the cases of TFL, avoiding the use of more aggressive therapies and providing the patient and the family with a more comfortable situation.
REFERENCES
1. HUSBAND, P. & KNUDSEN, A. - Idiopathic cervical and retroperitoneal fibrosis: Report of a case treated with steroids. Postgrad Med. J., 52: 788-793, 1976.
2. JAFFE, B. F. & JAFFE, N. - Head and neck tumors in children. Pediatrics, 51:731-740, 1973.
3. LAURENZO, J. F. & GRAHAM, S. M. - Tumefactive fibroinflammatory lesion of the head and neck: a management strategy. ENTJ, 74: 87-94, 1995.
4. OLSEN, K. D.; DESANTO, L. W.; WOLD, L. E., et. al. Tumefactive fibroinflammatory lesions of the, head and neck. Laryngoscope, 96: 940-944, 1986.
5. PATEL, P. C.; PELLITTERI, P. K.; VRABEC, D. P., et al. - Tumefactive fibroinflammatory lesion of the head and neck originating in the infratemporal fossa. Am. J. Otolaryngol., 19: 216-219, 1998.
6. PRICHARD, A. J. N.; COLLOBY, P.; BARTON, R. P. E., et al. - Tumefactive fibroinflammatorylesions of the head and neck. J. laryngol. Otol., 104: 797-800, 1990.
7. RICE, D. H.; BATSAKIS, J. G.; COULTHARD, S. W., et al. Sclerosing cervicitis: Homologue of sclerosing retroperitonitis and mediastinis. Arch. Surg., 110: 120-122, 1975.
8. SAID, H.; RAZI-HADI, A.; NOOR-AKMAL, S., et al. Tumefactive fibroinflammatory lesion of the head and neck. J. Laryngol. Otol., 102: 1064-1067, 1988.
9. SAVAGE, P. D.; WICK, M. R.; THOMPSON, R. C., et al. Tumefactive fibroinflammatorv lesion of the extremity: Report of a case and review of the literature. Arch. Pathol. Lab. Med., 115: 230-232, 1991.
10. WOLD, L. E. & WEILAND, L. H. - Tumefactive fibroinflammatory lesions of the head and neck. Am. J. Surg. Pathol., 7: 477-482, 1983.
11. YOUNG JR, J. L. & MILLER, R. W. - Incidence of malignant tumors in US children. J. Pediatr., 86: 254-258, 1975.
* Pathologist Physician of Associação de Combate ao Câncer do Brasil Central and Joint Professor of Endocrinoloy at Faculdade de Medicina do Triângulo Mineiro (FMTM)
** Undergraduate of School of Medicine at FMTM.
*** Surgeon and Assistant Professor of the Discipline of Pediatric Surgery at FMTM.
Address for correspondence: Dr. Marcus Aurelho de Lima - Disciplina de Endocrinologia do Hospital Escola - Faculdade de Medicina do Triângulo Mineiro - Rua Getúlio Guaritá, 130 - Abadia - 38025-440 Uberaba/ MG - Brazil - Tel: (55 34) 318-5292 / 5258 - Fax: (55 34) 312-6640 - E-mail: lima@mednet.com.br
Article submitted on October 4, 1999. Article accepted on May 30, 2000.