Year: 2000 Vol. 66 Ed. 5 - (16º)
Relato de Casos
Pages: 529 to 534
Carotid Body Tumor - a Case Report and Literature Review.
Author(s):
Gustavo P. Ferreira*,
Ricardo J. Gaspar**,
Henrique C. Pinto***,
Pedro P. Cintra***,
José A. Pinto****.
Keywords: paraganglia, carotid boby, paraganglioma
Abstract:
Paraganglioma are tumors that arise from paraganglia. They are rare, there is inheritability and malignancy is also rare. The most common one is carotid body paraganglioma (0,012% of all head and neck tumors). The most common feature is lateral cervical mass. Angiography is gold-standard for diagnoses. Surgical treatment is emphasised. We report the case of a 67 year-old woman with asimptomatic bilateral neck mass. Diagnostic and therapeutic approaches as outcome are described.
![]()
INTRODUCTION
Paragangliomas are tumors that surge from microscopic structures associated with the autonomic nervous system and are distributed on the para-axial regions of the brainstem, around branchiomeric arches and in the peripheral area of autonomic nervous system - the paraganglia.
Even though paragangliomas were originally named chemodectomas, the term carotid body tumors emerged as the most popular designation for those tumors located in the carotid bifurcation.
The most frequent paraganglioma is located in the carotid body (0.012% of head and neck tumors); less frequent locations are middle ear, jugular vein, vagus nerve, larynx and aortic arch.
Carotid body tumors present as lateral cervical masses of slow growth, and they may be manifested by symptoms that result from cranial nerve involvement, size of mass and endocrine activity.
Arteriography is the preferred exam for diagnosis of these tumors.
The advocated treatment is surgical. Techniques vary according to circumference extension of tumor and carotid arteries and degree of adherence of tumor to vessels. Preoperative embolization improves surgical results. Radiotherapy should be considered fot non-accessible, recurrent and partially resected tumors, as well as for patients whose surgery would be associated with high morbidity.
After an extensive review of the topic, we present the case of a 67-year-old patient with bilateral paraganglioma of carotid body operated in our service.
LITERATURE REVIEW
Carotid sinus is a structure that consists of extensible receptors located in the adventitia layer of lateral face of carotid bulb. Signs transmitted by the nerve of carotid sinus (Hering nerve) pass through glossopharyngeal towards the solitary tract of cerebral medullar area. From this area, secondary signs inhibit vasoconstrictor center of the marrow and excite the vagus. This parasympathetic response is mediated by two paths: 1) vasodilatation of veins and arterioles, and 2) bradycardia and increase of cardiac contraction force. Therefore, the final effect is decrease of blood pressure.
Carotid body is located along the medial face of carotid bifurcation, bilaterally. Its embryological origin is combined: mesoderm, from 3rd branchial arch, and ectoderm, from neural crest, from which derive the paraganglionar cells that integrate it.
The complex carotid sinus-body acts as a chemoreceptor and baroreceptor. The chemoreceptor function, especially mediated by carotid body, is sensitive to changes in partial pressure of oxygen and carbon dioxide (PaO2 and PaCO2), hydrogenionic potential (pH) and blood flow. Sensitivity of the organ is very high due to great tissue perfusion (three times more than cerebral flow)8.
In order to have constant stimuli from carotid body it is essential to regulate ventilation. If there is drop in PaO2, there is an increase in the discharge rate of carotid sinus nerve, increasing the rate of ventilation. Increase in ventilation is also observed if there is increase in PaCO2. Such is the sensitivity of the system that it enables regulation changes to take place in only one respiratory cycle.
Effects of pH and temperature changes are more indirect and may influence it through changes in partial pressure of gases. Chronic hypoxia is controlled by central mechanisms, with little participation of carotid body.
Apparently, the altitude of houses where patients live in relation to sea level plays an important role in the geneses of carotid body tumors, because prolonged hypoxia interferes not only in the function of the organ, but also in its growth.
Carotid body tumors are initially manifested as lateral cervical masses, consistent and of slow growth. Symptoms related to involvement of cranial nerves, size of mass and endocrine activity of tumor are less commons, present in only 30% of the patients.
There is predominance in female patients, but woman/ man ratio varies a lot in the literature (from 1.4:1 to 7.3:1)7,10.
The incidence is higher as from the fourth decade of life, and the peak is between the 5th and the 7th decades10.
They are classified as sporadic, familiar (autossomal dominant heritage) and hyperplastic (probably due to chronic hypoxia in high altitudes). Familiar tumors amount to 10% in most of the series, showing 30% of bilateral affection in these cases as opposed to 5% in sporadic cases5,4. The index of bilateral affection has reached 83%4. Familiar cases are diagnosed earlier because the family becomes aware of the likelihood of developing the disease. In the series of cases studied by Van der Mey12, familiar incidence reached 50% and multicentricity reached 55% of familiar cases.
The hypothesis that metastases were the cause of multicentric tumors was ruled out by DNA tests conducted by the author, who used flow cytometry to exclude the common cellular origin for different tumor sites.
Biological behavior of these tumors is intriguing. Although 40% of them have aneuploidia, this finding is not associated with the development of metastatic disease or aggressive growth pattern. Up to the moment, there is no known tumor marker. The incidence of malignancy varies from 5% to 10%6,8,10,12,2,9. The only malignancy criterion is process of metastatization, regardless of histological type and size of tumor.
The most common site of metastasis is the lymph node. There were also reports of pulmonary, cerebral and renal metastases6.
The incidence of cervical paraganglioma from a different origin than carotid body in association with carotid body tumor was demonstrated for the first time in the literature by Dalsing et al., in 19964, and it is explained by the common origin (neural crest) and wide distribution of these cells in the neck.
Endocrine activity characterized by secretion of catecholamines is very rare (1-3%)5, 4. The screening of active tumors includes dosage of plasma vanillylmandelic acid and urine and metanephrine analysis.
The existing relation between prevalence of these tumors in inhabitants of high altitudes and residents at sea level is 10:1 10.
The presentation of a carotid body tumor is very similar to the nodal metastasis on low digastric-jugular region. In a patient without evidence of primary site in the upper aerodigestive tract, it is necessary to carry out neck imaging tests, such as CT scan and MRI8.
Arteriography is the preferred exam for diagnosis of carotid body tumors, because it is a highly sensitive method (97%) and morbidity is nearly zero10. In addition, it provides information about size of lesion, presence of concomitant aterosclerotic lesions; degree of distortion/displacement of carotid vessels, origin of tumor arterial supply (internal or external carotid, vertebral or thyrocervical trunk) and detects contralateral tumors6,7,4,1.
The typical characteristics of paraganglioma of carotid body shown in the exam are opening of carotid bifurcation and vascular blush7,4.
Arteriography is essential for identification of large tumors that can be easily embolized. The risk of lesion during embolization is low, and it reduces blood loss and size of tumor, and facilitates the resection of large tumors, improving surgical results6,7,5. Embolization may be referred as a temporarily preoperative surgical technique, since the mass may acquire a new blood flow and continue its development if it is not resected.
Muhn et al.10 believed that diagnosis of carotid body tumor is better defined by ultrasound (USG) with Doppler. The typical finding is well-delimited hyper-vascularized mass opening carotid bifurcation.
Fine needle aspiration is not useful for diagnosis and open biopsy should be avoided, because of bleeding risk7.
Despite its need, assessment of cerebral perfusion in patients with high risk of internal carotid artery lesion is rarely performed. External compression of common carotid and electroencephalogram are unsafe methods for such purpose. Transcranial Doppler with carotid occlusion has a predictive value of 15%. Temporary occlusion with balloon and clinical or encephalographic monitoring has specificity of 75-90%. Such studies may be conducted pre and intra-operatively. However, they may be better employed before surgery because they give time for the surgeon to advise the patient and plan how to deal with the internal carotid artery during the procedure1.
In 1971, Shamblin et al. (apud 9) classified paragangliomas of carotid body in three groups, according to circumference extension of tumor in relation to internal and external carotid arteries, as well as to degree of adherence to adventitia of vessels. Group 1: relatively small tumors, with minimum adherence to carotid vessels, enabling the performance of surgical excision with little difficulty; Group 2: large tumors, moderate adherence to adventitia, enabling surgical excision through precise dissection; Group 3: larger tumors involving carotid arteries with one possibility only of en-block excision.
In 1984, Davidge-Pitts and Pantanowitz9 correlated these groups and size of tumor and concluded that tumors smaller than 6 cm corresponded to groups 1 and 2 of Shamblin; and tumors larger than 6 cm, to group 3 of Shamblin.
Therefore, tumors that should be dissected have at least 6cm in size and incomplete circumference extension, with an angle of carotid bifurcation below 90°, and those that should be rescted have more than 6crn and complete circumference extension and angle higher than 90°.
Intra-operative management of tumors in high risk patients for internal carotid damage should be based on the results of cerebral perfusion studies:
In patients passed satisfactorily through the test of temporary occlusion with balloon, the tumor is excised through peri-adventitia dissection, after placement of vascular clamps. If there is lesion of carotid vessels, it is safe to conduct systemic heparinization of patient and temporary clamping of carotid with small risks of complications. Vascular repair or reconstruction is then performed. Intra-operative shunt does not seem to be necessary in these patients.
Radiotherapy has been proposed as alternative to surgery in the treatment of carotid body tumors. It should be considered as the preferred treatment for non-accessible, recurrent and partially resected tumors, and for those patients whose surgery would be associated with high morbidity risk.
Between 1964 and 1992, the literature in English lists 31 patients with carotid body tumor treated with radiotherapy (with or without previous therapy), achieving local control in 30 of them (97%)11.
Tumor resection and the benefit of radiotherapy have been reported in cases of bone metastases. On the other hand, growth of tumor has already been described. It seems to be supported as a adjuvant therapy in malignant tumors after resection and in cases of local recurrence3.
The response of vascular tumors to radiation is limited to microvascular lesions, causing sclerosis and fibrosis. Death cell has not been demonstrated yet. Histopathological studies of Hawthorne et al.12 showed that tumor behavior after radiation is unpredictable. Eighteen irradiated tumors were investigated and 12 of them had live tissues without evidence of necrosis.
Reduction of surgical morbidity is closely related to exposure to ample surgery and careful identification of nerves before dissection.
Currently, the main cause of morbidity is damage to cranial nerves. In a review conducted by Mc Pherson et al.8 the incidence of neural lesion was of 17% to 57%, mean of 40%.
The resection of an isolate carotid body tumor is associated with a minimum risk of lesion of cranial nerve. The presence of multiple paragangliomas, however, increases dramatically this risk. The largest series reported morbidity incidence at about 24%, and 22.3% accounts for peripheral nervous paralysis.
Hypoglossus is the cranial nerve most frequently affected7.
Although the incidence of new post-operative paralysis is between 12% and 20%, natural history of the disease records the incidence of paralysis without surgery in 75%.
Analysis of 1,181 published cases of carotid body tumor revealed complications of central nervous system in 6.3% of the cases, and all these complications, except one, were present in patients who had internal carotid artery damage. Surgical general mortality was 3.2% and all deaths, except for one, took place in the group of patients who had the internal carotid artery damaged during the surgery1.
Out of 275 cases of vascular lesion involving internal carotid artery, most of them happened during dissection of tumors that were clearly adhered to the vessel wall.
In the series of 16 patients with bilateral tumors reported by Netterville8, 10 were submitted to bilateral resection. Two patients presented as if they had active pheochromocytoma. There were blood pressure and cardiac rate fluctuations. A complete assessment did not identify active tumors. Removal of baroreceptors interrupts the valuable feedback that controls acute changes in blood pressure. As a result of loss of function of baroreceptors provided by carotid sinuses, hypertensive response to stimuli is exacerbated, especially in early post-op conditions.
It is difficult to predict the post-operative progress of patients; however, patients with smaller tumors compensate them earlier.
As a result of loss of parasympathetic system feedback, sympathetic system is then responsible for most of cardiovascular morbidity observed after bilateral resection, and selective treatment should be carried out to control the excess of sympathetic stimuli.
Other complication recently described by Netterville8 and not clearly understood yet is pain in the carotid region during oral ingestion, called first-bite pain:
CASE REPORT
Female patient, aged 67 years old, smoker - 20 cigarettes a day for 40 years, complaining of "neck nodules" found during a thyroid physical exam two months before. She did not refer any other previous complaints.
ENT physical exam was normal. In the neck, there were two consistent and fixed masses, one on the left jugular-carotid region measuring 3x3cm, and the other on the right in the same area measuring approximately 1x2cm.
Complementary exams: Imaging exams (MRI and CT scans) (Photo 1) showed the presence of solid formations on jugular-carotid space at the level of carotid bifurcation, measuring on the left (the larger one) 4.0 x 3.0 x 2.0 cm. Arteriography (Photo 2) revealed the presence of hypervascularized expansive processes supplied by external carotid arteries, intensely impregnated by contrast and conditioning separation of carotids.
Treatment: We decided to conduct surgical treatment through a cervical incision from the left mastoid apophysis, over the hyoid bone, until the median line. We carefully dissected and preserved spinal nerves accessory, hypoglossus, vagus, glossopharyngeal and superior laryngeal (Photo 3). After detaching the tumor from its nourishing vessels originated from the external carotid artery, we conducted a peri-adventitia dissection, preserving carotids and removing tumor mass (Photo 4).
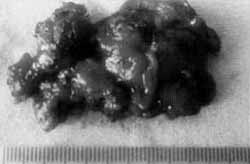
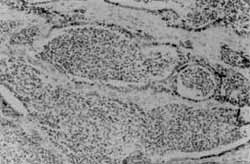
Anatomical pathological analysis: The macroscopic exam revealed a specimen of 4.5cm in diameter, brown burgundy color (Photo 5). Microscopic exam revealed cell niches (main cells) grouped in a highly vascularized connective stroma. Absence of morphological indicators of malignancy (Photo 6). Diagnosis: paraganglioma.
Post-operative progress: Patient remained in ICU for 2 days. She was discharged 6 days after the surgery. Paralysis of left hemilarynx for 2 months. Currently, 10 months after the surgery, she reported first-bite pain, presence of pharyngeal glomus; sialorrhea and low voice. Contralateral mass remains unaltered and the patient does not have complaints about it. At videolaryngoscopy, we observed intense salivary stasis, good vocal fold mobility. Videoswallowgram performed on the 12th post-operative month showed paralysis of left hemipharynx muscles.
DISCUSSION
According to the description in the literature, the carotid body tumor treated by our team presented initially as a lateral cervical mass, without any other symptomatology. Although they are not very common, complementary complaints involving endocrine activity of tumor, cranial nerve impairment and size of mass, may also be present in some cases (30%) and include cervical discomfort and pain, dysphagia, dysphonia and dyspnea, tinnitus, vertigo and headache, and symptoms of cerebral ischemia and hypertension.
Photo 1. MRI showing masses at the level of jugular-carotid region on both sides.
Photo 2. Arteriographic aspect of left mass, large opening of carotid bifurcation, showing the origin of tumor's vascularization (external carotid artery).
Photo 3. Trans-operative aspect. ACI = internal carotid artery; ACE = external carotid artery; ACC = common carotid artery.
Photo 4. Photo of post-resection of mass, preserving innervation and carotid vessels. ACI = internal carotid artery; ACE = external carotid artery; ACC = common carotid artery.
After clinical and endoscopic assessment without primitive tumor lesions, radiological study is essential to define the diagnosis.
According to radiological and clinical studies, the operated tumor was classified as group 2 of Shamblin (smaller than 6 cm).
In our procedure, we noticed the adherence of the tumor to the adventitia layer of the vessel; however, we managed to dissect it in circumference without damaging vascular walls.
Photo 5. Macroscopic aspect of surgical piece.
Photo 6. Microscopic aspect revealing niches of the main cells involved in connective stroma.
Despite careful dissection of regional nerves, the patient presented temporary sequelae of vocal fold paralysis, recovered spontaneously within 2 months, and she still has complaints compatible with cranial nerve paralysis possibly of 9th cranial nerve. First bite pain remains as a poorly understood symptom, based on the only report described in the literature.
FINAL COMMENTS
Although they are rare, carotid body tumors should be considered in differential diagnosis of cervical tumors. Diagnosis is difficult because they present clinically as lateral cervical node masses that may be mistaken by lymphnode metastases. Surgery is the gold standard treatment and the approach should be multidisciplinary, involving vascular surgeon as well, because in some cases, arterial reconstruction is also required.
REFERENCES
1. ANAND, V. K.; ALEMAR, G. O; SANDERS, T. S. - Management of the Internal Carotid Artery During Carotid BodyTumor Surgery. Laryngoscope, 105: 231-234, 1995.
2. COTTRELL, E. D.; SMITH, L. L.- Management of Uncommon Lesions Affecting' Extracranial Vessels. In: Rutherford, R. B. Vascular Surgery, Philadelphia, W. B. Saunders Company, 1995, 1622-1626.
3. FRUHWIRTH, J.; KOCH, G.; HAUSER, H.; GUTSCHI, S.; BEHAM, A; KAINZ, J.- Paragangliomas of the Carotid Bifurcation: Oncological Aspects of Vascular Surgery. Eur J. Surg. Oncol., 22: 88-92, 1996.
4. GARDNER, P.: DALSING. M.; WEISBERGER E.: SAWCHUK A; MIYAMOTO, R.- Carotid Body Tumors, Inheritance and a High Incidence of Associated Cervical Paragangliomas. Am J Surg., 172: 196-199, 1996.
5. LIAPIS, C.; GOUGOULAK1S, A; KARYDAKIS, V.; VERIKOKOS, C.; DOUSSAITOU, B.; SKANDALAKIS, P.; GOGAS, J.; SECHAS, M.- Changing Trends in Management of Carotid Body Tumors. Am. Surg., 61: 989-993, 1995.
6. Mitchell, R. O; Richardson, J. D.; Lambert, G: E.-Characteristics, Surgical Management and Outcome in 17 Carotid Body Tumors. Am. Surg., 62: 1034-1037, 1996.
7. MUHM, M.; POUTERAUER. P.; GSTOTTNER, W.; TEMMEL, A; RICHLING, B.; UNDT, G.; NIERDELE, B.; STAUDACHER, M.; EHRINGER, H.- Diagnostic and Therapeutic Approaches to Carotid Body Tumors. Arch. Surg., 132: 279-283, 1997.
8. NETTERVILLE, J.L.; REILLY, K.M.; ROBERTSON, D.; RELBER, M. E.; ARMSTRONG, W. B.; CHILDS, P.- Carotid Body Tumors. Laryngoscope, 105: 115-125, 1995.
9. PANTANOWITZ, D.; DAVIDGE-PITTS, K; DEMETRIADES, D. - The Significance of the Bifurcation Angle in Carotid Body Tumors. S. Afr. Med. J., 80: 318- 321, 1991.
10. PATINO, F. T.; ACOSTA, F. G.; PATRACA, C.G.; PARADA, J.M.; ALMEDARO, S.L. - Tumor de Cuerpo Carotideo. Analisis de 96 casos. Rev. Invest. Clin., 43: 119-123, 1991.
11. SCHILD, S. E.; FOOTE, R. L.; BUSKIRKE, S. J.; ROBINOW, J. S.; BOCK, F. F.; CUPPS, R. E.; EARLE, J. D.- Results of Radiotherapy for Chemodectomas. Mayo Clin. Proc., 67: 537-540,1992.
12. VAN DER MEY, A G. L.; FRIJNS, J. H. M.; DULKEN, H. V.; CORNELISSE, C. J.; TERPSTRA, H..L.; BRONS, E. N.; SCHMIDT, P. H.- Does Intervention Improve the Natural Course of Glomus Tumors?, 101: 635-641_ 1992.
* Resident Physician with Núcleo de Otorrinolaringologia a Cirurgia de Cabeça a Pescoço de São Paulo.
** Head of the Service of Vascular Surgery at Hospital São Camilo.
*** Physicians with Núcleo de Otorrinolaringologia a Cirurgia de Cabeça a Pescoço de São Paulo and Service of Otorhinolaryngology of Hospital São Camilo.
**** Director of Núcleo de Otorrinolaringologia a Cirurgia de Cabeça a Pescoço de São Paulo and Head of the Service of Otorhinolaryngology of Hospital São Camilo.
Study conducted at the Services of Vascular Surgery and Otorhinolaryngology of Hospital São Camilo.
Address for correspondence: Alameda dos Nhambiquaras, 159 - Moema - 04090-010 São Paulo/ SP - Tel: (55 11) 573-1970 - E-Mail: japorl@cepa.com.br
Article submitted on September 15, 1999. Article accepted on July 27, 2000.