Year: 2000 Vol. 66 Ed. 4 - (9º)
Artigos Originais
Pages: 373 to 379
Mouth Breathing: Causes and Changes of the Stomatolognathic System.
Author(s):
Suely M. Motonaga*,
Larissa C. Berte**,
Wilma T. Anselmo-Lima***.
Keywords: nasal obstruction, mouth breathing, children, etiology, stomatognathic system
Abstract:
Introduction: The craniofacial growth is determined by many factors, including the genetic inheritance, and chronic oral breathing. Aim: The aim of this research was to clinically evaluate the causes of the chronic mouth breathing and to observe the possible craniodentalfacial complex alterations. Material and method: We analyzed 104 children, ages ranging between three to 10 years. All of them accomplished the otorhinolaryngologic, the stomatognathic system, audiological and roentgenography evaluation. Results: The results showed that the most frequent causes of oral breathing were: allergic rhinitis, pharynx and/or palate tonsils hypertrophy, septal deformities or habit. In our study, the main craniofacial alterations were: open mouth on rest, ogival palate, narrow face with vertical growth predominancy, jaw on lower position and dental malocclusion. Some children presented alterations on the audiological evaluation and a greater number demonstrated alterations on the mastication and swallowing. We didn't observe significant association between the cause of obstruction versus facial features intensity neither between the adenoid obstructive degree versus facial features intensity. Conclusion: These findings allow us to affirm that most of the children who Nave nasal obstruction and chronic mouth breathing present craniofacial complex alterations.
![]()
INTRODUCTION
A number of articles both in medical and odonthologic literature have described the involvement of mouth breathing and facial and structural growth alterations, especially during childhood.
The existence of any obstacle in the breathing system, especially in the nasal and/or pharyngeal regions, will result in nasal obstruction, forcing the patient to breathe through the mouth24, that is, to make use of the oral cavity as a passive conductor of breathing. Therefore, chronic mouth breathing may be defined as habitual breathing through the mouth instead of through the nose, because of high nasal resistance8. These upper airway obstacles are frequently caused by structural abnormalities, nasal-sinusal pathologies or hypertrophy of lymphatic ring of Waldeyer.
In situations in which the nasal obstruction is not solved and becomes chronic, the subject becomes a mouth breather and manifests it clinically over the various organs and systems producing signs and symptoms that are not directly related with nasal breathing itself. There are a number of studies that demonstrate the association between mouth breathing and alterations of craniofacial morphology.
Chronic mouth breathing requires posture modifications of anatomical parts, such as the mandible and the tongue, which deviate downward and backwards, and the head, which is inclined backwards. These alterations may interfere in the direction of growth of mandible and teeth1. Therefore, as a consequence, adaptation of the facial muscles takes place, causing modifications of dental arches and dental positioning, resulting in structural alterations of facial osteoskeletal parts, such as lips, tongue, palate and mandible, which are adapted to the new breathing pattern23.
The conditions that result in acute nasal obstruction are normally originated from infectious processes and introduction of foreign bodies. Among those that result in chronic nasal obstruction we include choanal atresia, adenoid hypertrophy, hypertrophied chronic tonsillitis, septal deformity, nasal fracture, allergic rhinitis, medication rhinitis, nasal polyps, nasal tumors and narrow nasal fossae.
There are a number of situations that in spite of not resulting in nasal obstruction, are responsible for mouth breathing: hypopharyngeal obstruction, macroglossia, lip insufficiency and habit.
A child who has mouth breathing may be identified by typical facial characteristics, such as open mouth, short upper lip, evert and bulky lower lip, different degrees of narrowed face, flat nose, small and underdeveloped nostrils3,4,12,23. Dentition is also affected, comprising upper incisive protrusion, narrowing of maxilla, high palate and abnormal maxilla-mandible ratio11.
The first articles that described the typical appearance of adenoid hypertrophy date back from approximately 100 years. In the last 20 years, scientists realized that breathing mode may influence facial growth. The long face syndrome, according to what is known today, includes the excessive growth of the face, lip incompetence, narrowing of nostrils, protruded upper incisive, mandible lowering and posterior cross bite. Rubin (1980)21 stated that in cases of nasal obstruction, the mandible is lowered to create a mouth-breathing path.
Stomatognathic system consists of bones (mandible and maxilla), temporomandibular joint (TMJ), muscles, vascular and nervous systems and empty spaces. This system may be classified into two main groups: passive or static structures and active or dynamic structures. Static or passive structures correspond to osteodental arches, maxilla and mandible, articulated by TMJ, together with other cranial bones and hyoid bone. Dynamic or active structures are presented by the neuromuscular unit that mobilizes static parts, more susceptible to mobilization, such as the mandible or hyoid bone. Some functions carried out by this system are: breathing, mastication, swallowing and speech13,15. Any modification manifested on any of these structures may result in morphological change and functional disorder2.
The diagnosis of nasal obstruction in childhood is essentially clinical. We should combine a careful and comprehensive anamnesis, followed by detailed clinical exam, giving special attention to possible congenital morphological alterations, such as choanal atresia, septum deviation and neoplasia. They are also complemented by supplementary exams.
Some authors showed the importance of carrying out radiographic exam (cavum x-ray), to assess the size of adenoids and the degree of obstruction of nasopharynx, especially in children that do not cooperate in the physical exam6. Elwany (1987)7 showed that the relation between the measures of adenoid and the dimension of nasopharynx, described by Fujioka et al. (1979)9, expresses faithfully the size of pharyngeal tonsil and its relation with nasopharyngeal space, and that there is a correlation between clinical assessment and the weight of the adenoid removed surgically. Chami (1998)5 assessed the reliability of nasofibroscopy and cavum lateral x-ray when indicating surgery for children who had hyperplasic pharyngeal tonsil. He studied 46 patients who were aged between 1 year and 4 months and 10 years and 8 months. All subjects were submitted to anamnesis, radiological study (cavum x-ray), and nasofibroscopy. The assessment of radiological study was based on A/N ratio described by Fujioka et al. (1979)9 that define simple linear measures obtained in the lateral radiography of pharyngeal cavum. A/N ratio expresses radiologically the size of the pharyngeal tonsil and the patency of nasopharynx airways. The analysis of nasofibroscopic exams was obtained through measurement of the ratio between the area of pharyngeal tonsil (A) occupying part of the choana (C), as shown by Demain and Goetz (apud Chami, 1995)5. The author concluded that nasofibroscopy was more reliable than cavum radiography for the assessment of size and shape of pharyngeal tonsil, and that A/C ratio observed at nasofibroscopy was a more appropriate measuring instrument than the A/N ratio of radiography used to determine the degree of obstruction of pharyngeal tonsil.
In the last decade, some studies described not only craniofacial abnormalities, but also cardiorespiratory complications caused by nasopharyngeal obstructions in children10,20,25,26.
Chronic installation of mouth breathing during the period of growth of a child affects both the normal development of facial skeleton and, above all, the general health. A multidisciplinary team should work to have early diagnosis and appropriate treatment, preventing the consequent disorders of chronic mouth breathing.
This study aimed at assessing and defining the cause of mouth breathing in children, correlating orofacial morphological abnormalities and the degree of obstruction of nasopharynx using cavum x-ray and determining the occurrence of otological and hearing alterations in children with mouth breathing.
MATERIAL AND METHOD
One hundred and four children were studied - boys and girls, aged between 3 and 10 years, complaining of chronic mouth breathing, referred to the Speech and Hearing Pathology Clinic of UNESP-Campus Marília. We conducted complete ENT assessment, speech assessment (visual inspection and palpation of elements of stomatognathic system) and complementary exams, such as cavum radiography, pure tone audiometry and immitanciometry.
Data were recorded in a specific protocol, after authorization of parents or responsible accompanying person. Nasopharyngeal obstruction was determined by the measure of adenoid in radiological exams.
We assessed indirectly the size of adenoid tissue, that is, based on free nasopharyngeal air space, according to the method introduced by McNamara (1984)17, taking the measure in millimeters from the point of the anterior half of the posterior contour of soft palate to the point closet to the pharyngeal wall. According to values obtained, free nasopharyngeal air space was divided into 4 groups: the first group had nasopharyngeal space larger than 6mm; the second had values between 4.1 and 6mm, the third group, between 2.1 and 4mm, and the last group had values between 0 and 2mm.
We also measured the size of adenoid and nasopharynx (A/N ratio), based on the method described by Fujioka et al. (1979)9, consisting of first taking the measure of the adenoid (A), from the perpendicular distance between the maximum point of convexity along the inferior margin of adenoid shadow (Al) up to line B, traced on the anterior margin of basal-occipital region. The value of nasopharyngeal space (N) is obtained by the measures between 2 points C 1(posterior-superior extremity of hard palate) and D1 (anterior-inferior extremity of spheno-basal-occipital synchondrosis). Based on A/N ratios, we classified them as large, normal or small.
For statistical purposes, we employed the method of qui-square by Pearson, and for rejection of hypothesis of nullity, we defined significance level of 5%.
RESULTS
Out of 104 children, 48 (46.15%) were girls and 56 (53.85%) were boys - mean age of 6.44 years.
As to ENT anamnesis, most of the children had complaints of snoring (81.73%) and predominantly mouth breathing (97.12%). Episodes of sleep apnea were reported in 26 (25%) children. Parents also informed that 84 (80.77%) children had allergic rhinitis and 39 (37.5%) had bronchial asthma. Most common repetitive infections were tonsillitis and sinusitis followed by otitis and pneumonia.
Concerning the specific physical exam, we observed at anterior rhinoscopy the presence of 27 (25.96%) children with septal deformity, and 76 (73.08%), with coriza. As to status of turbinate, 89 (85.58%) children had hypertrophy and 77 (74.04%) had them pale. At oroscopy, we observed high palate in 91(87.50%) children and hypertrophied gums in 20 (19.23%).
Causes of mouth breathing were determined by anamnesis and physical exam and complemented by cavum radiography. We diagnosed allergic rhinitis (RA) in 34 (32.69%) children; adenoid hypertrophy (HVA) in 12 (11.54%); tonsil hypertrophy (HA), in 4 (3.85%); adenoid and tonsil hypertrophy (HAVA), in 7 (6.73%); habit in 8 (7.69%); and associated pathologies (more than one of the above-mentioned) in 39 (37.5%) cases assessed (Table 1).
According to data collected from speech anamnesis, we noticed that 10 (9.62%) children had not been breastfed, whereas 53 (50.96%) had been breastfed until the age of 6 months; and 41(39.42%), after 6 months of age. As to bottle-feeding, only 13 (12.50%) children did not use it; 11(10.58%), used it up to the age of two, and the majority, 80 (76.92%), after the age of 2 years. As to pacifier, 31(29.81%) children did not use it; 16 (15.38%), up to the age of 2 years, and 57 (54.81%), after the age of 2 years. Most of the children did not use to suck the thumb, and only 10 (9.62%) did it after the age of 2 years (Table 2). As to alterations of stomatognathic system, assessed by means of visual inspection and palpation, we observed indicative characteristics of normocephalus in 30 (28.85%) children; dolichocephalus in 67 (64.42%); and brachycephalus in 7 (6.73%) of the children assessed. We also detected dark circles around the eyes in 99 (95.19%) children; lowered mandible in 88 (84.62%) children; open mouth in 92 (88.46%); morphological alterations of upper and/or lower lips and dental alterations in 98 (94.23%) mouth breathers (Table 3). Only 2 children had mastication and swallowing patterns within the ranges of normality, except for those below the age of 4 years (three cases).TABLE 1 - Causes of mouth breathing.
After this step, children were divided into 2 groups, A and B, according to the number of orofacial modifications (facial characteristic suggestive of dolichocephalus, open mouth, impaired upper and/or lower lip, high palate, lowered mandible and dental malocclusion). Children in group A had from 1 to 3 of those characteristics, and in group B they had between 4 and 6 orofacial characteristics. We associated then the size of adenoid (Fujioka et al. method and McNamara method) and orofacial characteristics (Tables 4 and 5). The statistical analysis employed did not show statistically significant difference as to size of adenoid in both methods when compared to orofacial characteristics.
In addition, we analyzed the association of pathologies and orofacial characteristics, size of adenoids (Fujioka et al. method) and dental malocclusion: posterior cross bite and/or open bite. Statistical analysis used did not produce statistically significant differences.
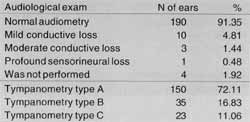
As to audiometry, two children (4 ears) were not submitted to it. We found normal audiometry in 190 (91.35%) ears, mild conductive hearing loss in 10 (4.81%), moderate conductive loss in 3 (1.44%) and sensorineural loss in one single ear. In tympanometry, we observed type A curves in 150 (72.11%) ears, type B curve in 35 (16.83%) ears and type C, in 23 (11.06%) ears (Table 6).
DISCUSSION
Chronic nasal obstruction, especially in childhood, may cause morphological changes of craniodentofacial complex. This statement has been considered for many years by innumerous researchers.TABLE 2 - Speech pathology anamnesis.
TABLE 3 - Alterations of stomatognathic system.
TABLE 4 - Size of adenoid (method of Fujioka et al.) and orofacial characteristics.
x² = 5.06; g.l. = 2; p = 0.079
TABLE 5 - Size of adenoid (method of McNamara) and orofacial characteristics.
x² = 3.82; g.l. =2; p = 0.148
Among the causes of nasal obstruction, allergic rhinitis and hypertrophy of lymphatic ring of Waldeyer are the most frequent in children5,18. The majority of the studies focused on affections such as adenoid and tonsil hypertrophy and allergic rhinitis. There are other pathologies that are rare and not part of the daily practice of otorhinolaryngologists.
In our study, among the main causes of mouth breathing we detected the presence of allergic rhinitis (32.69%), adenoid and/or tonsil hypertrophy (22.12%), habit (7.69%) and also association of obstructive pathologies (37.50%). We noticed that 54.81% of the assessed cases - approximately half of the studied population, had as cause allergic rhinitis and adenoid and/or pharyngeal tonsil hypertrophy.
Weckx and Weckx (1995)24 reported the presence of mouth breathing because of habit, that is, the maintenance of mouth breathing after the institution of any kind of treatment for permeability of upper airways. Our results showed the presence of approximately 7% of the population with mouth breathing because of habit. However, this cause should be highlighted, because many children maintain mouth breathing after the treatment, what reinforces deformities. In this case, speech assessment and therapy are required in order to try to adapt the elements of stomatognathic system according to each individual's needs, as reported by Marchesan a Krakauer (1995)14.
We also observed a large proportion of associated pathologies, that is, the occurrence of more than one cause of obstruction in the same child. The most common combinations were: allergic rhinitis and hypertrophy of palatine or pharyngeal tonsil, allergic rhinitis and septal deviation, or septal deformity with hypertrophy of palatine or pharyngeal tonsil. For more than half of the studied population the main causes of obstruction were allergic rhinitis and hypertrophy of palatine or pharyngeal tonsil.
A mouth breather is identified by means of history and visual inpection4, 12. Smith (1989)22, however, said that the identification of the patient with mouth breathing should not be based only on isolated clinical impressions, but rather that it should be followed by objective exams. Several studies suggested the existence of craniofacial abnormalities resultant from mouth breathing, such as Marks and Beach (1965)16 who described dental malocclusion and high palate in children with allergic rhinitis.
The denominations "adenoid face" or "long face syndrome" have been used to describe the typical characteristics of subjects with mouth breathing. Deformities of dental arches and palate and retro-positioning of the mandible are constant findings in the population of mouth breathers. According to Marchesan (1994)15, it is known that mouth breathing is more frequently seen in dolichocephalic subjects because the third inferior of the face is longer, making lip closure and tongue position more difficult for them.TABLE 6 - Results of audiological exam (N=208 ears).
Our results concerning stomatognathic system were: characteristics suggestive of normocephalus in 28.8% of children, suggestive of dolichocephalus, 64.42%, and brachycephalus, 6.73%. Other findings collected for this population were: dark circles around the eyes in 95.19%, lowered mandible in 84.62%, open lips in 88.46%, and morphological alterations of upper and lower lips in 94.23% of the children. By means of visualization, we observed that children had faces tending to dolichocephalic pattern, associated with narrowing of upper jaw and a trend of anterior open bite. The results obtained were similar to the ones reported by different authors in the literature.
Therefore, children with mouth breathing tend to present narrow and elongated growth of the face, marked with dark circles around the eyes and modifications of lower and upper lips. These changes are not exclusive to children with nasal obstruction and we should take into account the influence of genetics and the facial characteristics of parents.
Clinical assessment to visualize indirectly adenoid tissue in children is not easy to be carried out and sometimes it is even impossible. Therefore, radiographic image of nasopharynx in profile allows objective, precise and easy measurements. It is paramount that the patient is positioned correctly when performing the radiography; patients should not cry or swallow, because they cause an elevation of soft palate, giving the impression of obstruction. Several methods were described but not one has been largely applied. Methods that demonstrate more reliable data are those related to size of adenoid and nasopharynx, and not isolated measures, because lymphoid tissue is localized in the nasal-pharyngeal space. It is believed that diagnostic imaging techniques alone do not provide enough information and that they should be associated with anamnesis and physical exam19. Adenoid palpation is not a reliable method of measurement, and it is very traumatic for children. Radiological imaging provides more information when compared to palpation. Currently, we have been using the method of visualization of adenoid tissue through endoscopic exams. This exam provides direct and tridimensional image of nasopharynx and its structures.
We noticed in our study that there was no correlation between size of adenoid (method of Fujioka et al. and method of McNamara) and the frequency of craniofacial alterations. However, children with mouth breathing showed the following orofacial abnormalities at the physical exam: elongated and narrowed face, open mouth, impaired upper and lower lips, high palate, low mandible and dental malocclusion (posterior cross bite and/or open bite). We may infer that craniofacial skeletal changes are not influenced only by nasal obstruction, because there is also the involvement of genetic characteristics and possibly also the influence of negative habits (bottle feeding, pacifier and digital suction).
Based on audiometry, we also detected that 8.65% of the children studied had some type of hearing loss, and the most common type was mild to moderate conductive hearing loss. Type A curves of tympanometry were found in 72.11%, and curves type B and C amounted to 16.83% and 11.06%, respectively. We observed that most of the patients had normal middle ear pressure. However, some children showed alterations of middle ear pressure, what could be possibly explained by partial or total block of Eustachian tube opening by adenoid tissue.
The relation between nasal obstruction and craniofacial morphology is a problem that requires multidisciplinary care, involving at least otorhinolaryngologist, orthodontist and speech and hearing pathologist. These professionals should cooperate in the diagnosis so that proper intervention may be defined, minimizing the consequences caused by chronic mouth breathing.
CONCLUSION
Based on the results, we concluded that:
1. the main causes of mouth breathing in children were: allergic rhinitis, adenoid and/or tonsil hypertrophy, habit and associated obstructive pathologies;
2. the most common morphological abnormalities of stomatognathic system were: suggestive dolichocephalic face, dark circles around the eyes, lowered mandible, open lips, impaired upper aid lower lips, and dental abnormalities. We also observed alteration of mastication and swallowing patterns;
3. there was no association between size of adenoid tissue and frequency of orofacial alteration;
4. there was no association between cause of obstruction and frequency of orofacial alteration;
5. a minority of children had auditory problems, all of conductive nature.
REFERENCES
1. ADAMIDIS, I. P.; SPYROPOULOS, M. N. - The effects of lymphadenoid hypertrophy on the position of the tongue, the mandible and the hyoid bone. European Journal of Orthodontics, Oxford, 5: 287-294, 1983.
2. ALTMANN, E: B. C. - Deglutição atípica. In: Kudo, M. (Coord.) Fisioterapia, Fonoaudiologia a Terapia Ocupacional em Pediatria. São Paulo: Sarvier, 1990: 116-131. (Monografias Médicas: Serie Pediatria, 22)
3. ARAGAO, W. - Respirador bucal. Jornal de Pediatria, Rio de Janeiro, 64(8): 349-352, 1988.
4. BRESOLIN, D. et al. - Facial characteristics of children who breathe through the mouth. Pediatrics, Springfield, 73(5): 622-625, 1984.
5. CHAMI, F. A. I. - Avaliação nasofibroscópica a radiológica de pacientes com hiperplasia da amígdala faríngea. Revista Brasileira de Atualização em Otorrinolaringologia, São Paulo, 5(4): 118-125, 1998.
6. COHEN, L. M.; KOLTAI, P. J.; SCOTT, J. R. - Lateral cervical radiographs and adenoid size: do they correlate? ENT Journal, 71 (12): 638-642, 1992.
7. ELWANY, S. - The adenoidal-nasopharyngeal ratio (NA ratio): its validity in selecting children for adenoidectomy. The Journal of Laryngology and Otology, Ash ford, 101: 569-573, 1987.
8. EMSLIE, R. D.; MASSLER, M.; ZWEMER. J. D. - Mouth breathing I: etiology and effects (a review). The Journal of the American Dental Association, Chicago, 44: 506-521, 1952.
9. FUJIOKA, M.; YOUNG, L. W.; GIRDANY, B. R.-Radiographic evaluation of adenoidal size in children: adenoidal-nasopharyngeal ratio. American Journal of Roentgenology, Baltimore, 133: 401-404, 1979.
10. KONNO, A.; HOSHINO, T.; TOGAWA, K. - Influence of upper airway obstruction by enlarged tonsils and adenoids upon recurrent infection of the lower airway in childhood. Laryngoscope, St, Louis, 90: 1709-1716, 1980.
11. LINDER-ARONSON, S. -Adenoids: their effect on mode of breathing and nasal airflow and their relationship to characteristics of the facial skeleton and the dentition. Acta Oto-Laryngológica, Stockholm, 265: 5-132, 1970. Supplement.
12. LOPEZ-MARURE, E. N.; AGUDELO - VEJA, B. L; ECHEVERRI, J. D. - Medición de tejido adenoideo en placa lateral de nasofaringe: correlación clínico radiológica. Boletín Medico del Hospital Infantil, Mexico, 46(6): 409-413, 1989.
13. MARCHESAN, I. Q. - O trabalho fonoaudiológico nas alterações do sistema estomatognático. In:_______ (Org.). Tópicos em Fonoaudiologia. São Paulo: Lovise, 1994: 83-96.
14. MARCHESAN, I. Q.; KRAKAUER, L. H. - A importância do trabalho respiratório na terapia miofuncional. In: Marchesan, I. Q. (Org.). Tópicos em Fonoaudiologia. São Paulo: Lovise,1995: 155-160.
15. MARCHESAN, I. Q. - Avaliando a tratando o sistema estomatognático. In: Lopes Filho, O. (Ed.). Tratado de Fonoaudiologia. São Paulo: Roca, 1997: 763-780.
16. MARKS, M. B.; BEACH, M. -Allergy in relation to orofacial dental deformities in children: a review. Journal of Allergy, St. Louis, 36(3): 293-302, 1965.
17. McNAMARA Jr.. J. A. -A method of cephalometric evaluation. American Journal of Orthodontics, St. Louis, 86(6).449-469, 1984.
18. MOCELLIN, M.; PASINATO, R.; FARIA. J. L. - Obstrução nasal. In: Ramos, B. D. (Coord.) Manual de Otorrinolaringologia, Rio de Janeiro: Sociedade Brasileira de Pediatria,1994: 79-84.
19. OULIS, C. J. et al. - The effect of hypertrophic adenoids and tonsils on the development of posterior crossbite and oral habits. The Journal of Clinical Pediatric Dentistry, Sapporo, 18(3): 197-201, 1994.
20. Potsic, W. P. -Sleep apnea in children. Otolaryngologic Clinics of North America, Philadelphia, 22(3): 537-544, 1989.
21. RUBIN, R. M. - Mode of respiration and facial growth. American Journal of Orthodontics, St. Louis, 78 (5): 504-510, 1980.
22. SMITH, R. M. -The relationship between nasal obstruction and craniofacial growth. Pediatric Clinics of North America, Philadelphia, 36(6): 1423-1434, 1989.
23. SUBTELNY. J. D. -Effect of diseases of tonsils and adenoids on dentofacial morphology. Annals of0tology, Rhinologyand Laryngology, St. Louis, 84: 50-54, 1975.
24. WECKX, L. L. M.; WECKX, L. Y. - Respirador bucal: causas e conseqüências. In: Jornada Internacional de Otorrinolaringologia, 1., Jornada Internacional de Fonoaudiologia, 2. Ribeirão Preto: Centro de Estudos Otorrinolaringológico "Ricardo Marseillan", 1998: 45-55. (Collectanea Symposium. Serie Medicina & Saúde)
25. WHITE, P.; FORTE, V. -Surgical management of nasal airway obstruction in children. TheJournal of otolaryngology, Toronto, 18(4): 155-157, 1989.
26. YONKERS, A. J.; SPAUR; R. C. - Upper airway obstruction and the pharyngeal lymphoid tissue. The Otolaryngologic Clinics of North America, Philadelphia, 20(2): 235-239, 1987.
* Master degree in Otorhinolaryngology, Faculdade de Medicina de Ribeirão Preto - USP, Assistant Professor of the Course of Speech and Hearing Pathology at UNESP - Marília /SP.
** Speech Pathologist and Master degree in Education under course at UNESP - Campus Marília.
*** Ph.D. and Assistant Professor of the Department of Ophthalmology and Otorhinolaryngology at Faculdade de Medicina de Ribeirão Preto - USP /SP.
Dissertation Thesis, Master Degree in Otorhinolaryngology, Faculdade de Medicina de Ribeirão Preto /SP.
Address for correspondence: Faculdade de Filosofia a Ciências-Depto. de Fonoaudiologia - Avenida Higino Muzzi Filho, 737 - Campus Universitário.
17525-900 Marília /SP - Tel: (55 14) 421-1224 - Fax (55 14) 422-4797.
Article submitted on March 8, 2000. Article accepted on March 30, 2000.