Year: 2000 Vol. 66 Ed. 4 - (5º)
Artigos Originais
Pages: 343 to 346
ABR in Patients with Ischemic Heart Disease and Comparison With Normal Persons.
Author(s):
Fabiana O Pereira*,
José A. A. Oliveira**.
Keywords: ABA, heart disease, coronary disease, heart attack
Abstract:
Introduction: ABR has demonstrated to have high sensibility to show several metabolic disturbances, as diabetes, hypertension and dislipidemia. There are, although, few studies that relate abnormalities in conduction from cochlea to inferior colliculus with ischemic heart lesions or aterosclerosis. Purpose: in this study, with ABR, we intended to evaluate abnormalities in brainstem vascular microcirculation associated with heart ischemic disease. Material and method: 24 patients with ischemic heart disease were evaluated, with mean age of 56 years (varying from 38 to 76 years), being 18 males and six females. These patients were compared to 24 normal volunteers, with age varying from 45 to 76 years (mean age of 61 years), 13 males and 11 females. Latencies of waves I, III and V, interpeak latencies I-III, I-V and III-V and peak amplitudes of waves I and V were evaluated. Results: Peak amplitude of wave V was diminished in patients with ischemic heart disease if compared to volunteers. Conclusion: Ischemic heart disease could be related to abnormalities in brainstem vascular microcirculation, seen through diminution in wave V amplitude.
![]()
INTRODUCTION
ABR is a non-invasive method of neurophysiological assessment that has high sensitivity to detect cerebral electrical responses to auditory stimuli, at different click intensities3.
It is known that some metabolic diseases, such as hypertension, diabetes2, dislipidemia1, or ischemic lesions generate modifications both in speed and intensity of electrical impulses from the cochlea to the brainstem.
It has also been shown that ABR carried out at high intensities can show metabolic disorders with high sensitivity. However, there are few studies that relate cardiac or arteriosclerotic ischemic disorders and central electrical impulses, both at speed and intensity of conduction.
Karamitsos4 compared with ABR patients with and without ischemic heart disease. It was shown in this study that patients with ischemic heart disease have significant alterations of amplitude and latency of waves at brainstem level. However, no alterations were noted for latency and amplitude at the level of cochlear nerve.
Arteriosclerosis, frequently affecting patients who have ischemic heart disease, occurs in a generalized fashion. It affects the so-called target organs, such as brain, lungs, kidney and retinal. The cochlea is currently being considered a target organ. It is widely known now that affection of target organs by arteriosclerotic lesions increases considerably the risk of developing ischemic myocardial episodes.
OBJECTIVES
Using short-latency ABR, we intended to check the existence of functional impairment of cochlear nerve up to inferior colliculus in patients with ischemic myocardial disease.
We aimed at assessing with ABR latency and amplitude of electrical impulses of cochlea and inferior colliculus, comparing their results to those of healthy subjects.
MATERIAL AND METHOD
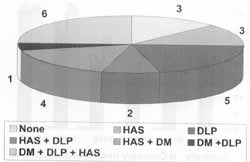
We evaluated 24 patients with ischemic heart disease 18 had suffered acute myocardial infarction and 6 had unstable angina. Patients were neurologically asymptomatic and 18 were male and 6 were female patients. Ages ranged from 38 to 76 years (mean age of 58 years). Some of them had associated pathologies, such as diabetes (DM), systemic arterial hypertension (HAS) and dislipidemia (DLP), distributed as shown in Fig. 1.
These patients were compared to 24 volunteers who were also neurologically asymptomatic and without any of the pathologies listed above, divided into 13 male and 11 female subjects. Ages ranged from 45 to 76 years (mean age of 61 years).
Figure 1. Distribution of associated pathologies, diabetes (DM), dislipidemia (DLP) and hypertension (HAS) in patients with ischemic heart disease.
All patients were audiologically assessed though otoscopy, pure tone audiometry and speech recognition index, and acoustic immitance measure. Ears with moderate disorders in any of the exams were excluded from the sample.
Patients were then submitted to ABR with clicks of alternate polarity in stimulus frequency 11.4/sec and intensity of 90dB in each ear. We assessed amplitude of waves I and V, latency of waves I, III and V and interpeak latency of waves IIII, I-V and III-V in each of the exams.
Subjects had been informed about the exams they were undertaking and agreed to do so. This study was reviewed and approved by the Commission of Medical Ethics at Hospital das Clínicas da FMRP-USP.
The results of patients with ischemic heart disease were compared to those of normal controls using Student t test for sample of different sizes.
RESULTS
Audiometry
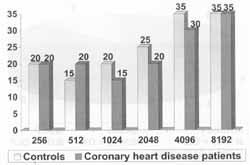
Results of audiometry, immitance measures and speech recognition index of patients with ischemic heart disease were similar to those of the controls. Two exams of ischemic heart disease patients were excluded (each ear of two different patients) because thresholds were 'below 40 dB in high frequencies (higher than 2000 Hz). Mean results of each frequency in controls and in patients are illustrated in Fig. 2.
ABR
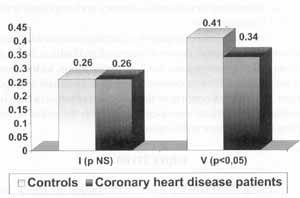
Results obtained from the comparison between is chemic heart disease patients and healthy controls showed reduction of wave V, with statistically significant difference (p<0.05). As to amplitude of wave I, there was no statistically significant difference.
Figure 2. Average of audiometric thresholds (in dB) in each frequency (in Hz).
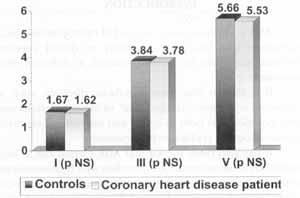
Figure 3. Comparison of latencies of waves I, III and V (in ms) between patients with ischemic heart disease and the controls.
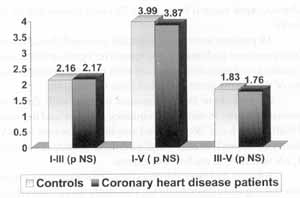
Figure 4. Comparison of interpeak latencies of waves I-III, I-V and III-V (in ms) between ischemic heart disease and controls.
Figure 5. Comparison of amplitude of waves I and V (in mV) between ischemic heart disease and controls.
There were no statistically significant differences in latencies of waves I, III and V, or in interpeak intervals of waves I-III, I-V and III-V.
Results are presented in Figures 3, 4 and 5.
DISCUSSION
Results obtained from this study showed a reduction of amplitude of wave V in ischemic heart disease patients compared to normal controls. It shows that there is an impairment in the circulation at the level of brainstem in these patients compared to normal controls, especially at the level of inferior colliculus. It is a slight difference especially because amplitude is less sensitive than latency.
In a similar a study, Karamitsos et al.5 related significant alterations of circulation at the level of brainstem in patients with ischemic heart disease, evidencing increase of latency of waves II, IV and V and reduction of amplitude of waves I and V, when compared to normal controls. These alterations were not significant in our study. The difference in results between the two studies could be explained by the duration of ischemic heart disease, what may influence cerebral circulation. Since this factor was not determined in any of the studies, their comparison becomes impossible. It is worth pointing out that the number of patients, despite significant, was not large enough to understand the reason for this difference. Another factor that was not comparable between the two studies was the presence of metabolic diseases, a fact not considered in the study of Karamitsos et al. It is widely known that metabolic alterations associated with ischemic heart disease, such as diabetes and dislipidemia, do influence ABR.
We know that some pathologies, among them diabetes2 and dislipidemia1, result in ABR alterations both at the level of cochlea and brainstem. In other animal experimental studies4, cochlea was considered an organ directly affected by blood microcirculation pathologies, as well as lungs, kidneys, eyes and heart. Cochlear function, assessed by means of amplitude and latency of wave I, was not affected in ischemic heart disease patients in our study, similar to the results of the study by Karamitsos5.
CONCLUSION
This study confirmed the hypothesis that blood microcirculation pathologies that result in ischemic heart diseases may lead to cerebral microcirculation abnormalities, despite the fact that results were not very significant, showing only reduction of wave V.
However, in our study, we did not confirm the hypothesis that cochlear microcirculation would also be affected, a hypothesis made for animal models, but which has not been confirmed in any ABR study in humans yet.
REFERENCES
1. BEM DAVID, J.; PRATT, H.; LANDMAN, L. et al. -A comparison of -auditory brainstem evoked potentials in hyperlipidemic and normolipidemic subjects. Laryngoscope 1986; 98:186-189.
2. BULLER, N.; SHVILLI, Y.; LAURIAN, N. et al. - Delayed brainstem auditory evoked responses in diabetic patients. J Laryngol Otol 1988;102:357-360.
3. CHIAPPA, K. H.; ROPPER, A. H. - Evoked potentials in clinical medicine. N. Engl J. Med 1980; 305: 1140-1147.
4. KARAMITSOS, D. G.; NICHOLAS, G. et al. - Brainstem auditory evoked potentials in patients with ischemic heart disease. Laryngoscope 1996; 106: 54-57.
5. SIDMAN, J. D.; PRAZMA, J. et al. - Cochlea and heart as end organs in small vessels disease. Am Otol Laryngol 1988; 97: 912.
* Resident Physician of the Department of Otorhinolaryngology at Hospital das Clínicas, Faculdade de Medicina de Ribeirão Preto /SP.
** Faculty Professor and Head of the Department of Otorhinolaryngology at Hospital das Clínicas, Faculdade de Medicina de Ribeirão Preto /SP.
Study presented at I Congresso Triológico de Otorrinolaringologia, in São Paulo/ SP, November 13 - 14, 1999.
Address for correspondence: Departamento de Otorrinolaringologia do Hospital das Clinicas da Faculdade de Medicina de Ribeirão Preto, da Universidade de São Paulo.
Avenida dos Bandeirantes, 3900 - 14096-900 Ribeirão Preto /SP - Tel: (55 16) 602-2863 / Fax: (55 16) 633-0186.
Article submitted on January 17, 2000. Article accepted on June 1, 2000.