INTRODUCTIONMaxillary sinus, the largest of the paranasal sinuses, is a pneumatic space contained in the bilateral maxillary bones. Its large volume associated with capillary fragility and proximity to the apex of some upper teeth allow, in some circumstances, the creation of direct access between it and the oral cavity, which is called oroantral communication. If this accessing canal between the cavities is recovered with epithelial tissue, originated from proliferation of tissue that surrounds the communication, it receives the name of oroantral fistula (Rezende, Heitz).
As to etiological factors, the opening of the maxillary sinus is frequently conducted accidentally during dental extractions. Such perforation normally involves teeth with diverging roots close to edentulous spaces, a situation in which the maxillary sinus becomes pneumatized, weakening the alveolus and leading the dental apex closer to the sinusal cavity (Marzola; Schow).
Upon analyzing the frequency of fistulas and gender, Krause, Pruzzo, Fonseca pointed to male preference, especially during the third decades of life.
The diagnosis of oroantral fistulas involves clinical and radiological procedures. Krause, Pruzzo, Fonseca suggested the conduction of Valsalva's maneuver - in case of fistula, there is discharge of air through alveolar canal or pus through the communication, depending on the maxillary sinus status.
The patients affected by oroantral fistula manifest symptoms such as liquid leak through the nose, nasal vocal quality, swallowing disorders for liquid and solids, halitosis, coriza, affected taste, unilateral nasal obstruction, pain on the face and frontal headache (when there is acute maxillary sinusitis), unilateral nasal dripping and night cough owing to drainage of exsudate to the pharynx. The exsudate that is swallowed can produce morning anorexia, in addition to epistaxis in the affected side and inability to blow or aspirate smoke from a cigarette. In old communications, the margins of the orifice are normally smooth and sometimes we can see hyperplastic tissue, which proliferates towards the oral cavity (Rezende, Heitz8).
One of the main complications of oroantral communications is acute or chronic maxillary sinusitis, originated from the contamination of the sinus by the oral flora. The communications can be evidenced through periapical x-rays in which we can observe discontinuity of the radiopaque line that delimits the floor of the maxillary sinus. Small orifices, especially those located on the wall of the anterior sinus, can be hardly evidenced in the radiological images. Extra-buccal images (panoramic and Waters' plans) are also restricted concerning in small communications; the main importance is in the observation of the involved maxillary sinus, which can present diffuse radiopacity (sinus opacification), when compared to the sinus on the opposite side. It can be most helpful in identifying foreign bodies in the sinus, occlusal superior, posterior-inferior, frontal-nasal-plaque and face profile images.
The patients with acute maxillary sinusitis can have tumefaction and redness of the area over the molar sinus and eminence, as well as pain under the eye. Palpation over the maxillary sinus will increase pain, and the teeth with adjacent roots to the sinus will frequently present with pain or tenderness to percussion. In chronic sinusitis resulting from oroantral fistula, normally there is nasal and post-nasal coriza together with halitosis and mild sensation of pain and obstruction of the affected face side. The treatment of oro-antral communications should be performed immediately when the opening is created or later in cases of failure of primary closure (Schow9).
The purpose of the present study was to report three cases of oroantral fistula with specific treatment propositions, contributing to the information of professionals about appropriate diagnosis and surgical techniques.
CASE REPORTBefore we start to report the peculiarities of each case, it is important that we report that all three patients followed the same protocols concerning radiological images (Ortopan-tomogram, Facial PA with maxillary sinus projection, periapical and occlusal incidences), clinical examinations (intra-buccal physical examination, including Valsalva's maneuver), preoperative tests (complete blood count, complete coagulation, and glucose), preoperative treatment of sinusitis (inhalation and nasal instillation), systemic antibiotic therapy (amoxycillin + potassium clavulanate + metronidazole for 15 days), pre-medication (Paracetamol and codeine phosphate), manufacturing of an acrylic dental plate, and postoperative recommendations, differing only in flap harvesting technique, as described next.
CASE REPORT 1
Male 26-year-old patient, came to the Dental Clinic at Universidade Estadual de Feira de Santana complaining of air escape through the mouth. Intra-buccal physical examination revealed an opening in the region of the 1st upper molar tooth on the left and many absent teeth (Figure 1a). The patient reported that he had been submitted to extraction about 10 months before by an unreliable professional in the region. We conducted Valsalva's maneuver (compression of nostrils with the fingers and blowing out the air) and we detected air leak in the area. Using ortopan-tomogram as a reference, we observed loss of continuity in the radiopaque lines of the floor of the maxillary sinus on the left (Figure 1b). He also presented acute maxillary sinusitis. The treatment proposed was closure of oroantral fistula with vestibular flap. First, we made an incision around the region of the fistula to collect the flap from the first plane (Figure 1c). Next, we made a vestibular incision up to tuberosity using the mesial plan to make a second-plan flap (Figure 1d). Tuberoplasty conducted with high rotation bur to provide better mucous recovery and relaxation of the flap (Figure 1e). The patient has been followed up every 6 months and to present, he has had no signs of recurrence (Figures 1f).

Figure 1a. Clinical aspect of the fistula.

Figure 1b. Panoramic x-ray of the maxillary sinus.

Figure 1c. First plan suture of sinusal mucosa.

Figure 1d. Vestibular flap to be suture on the second plan.
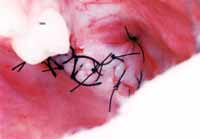
Figure 1e. Final suture of the region.

Figure 1f. One-week post-operative aspect.
CASE REPORT 2
Male 62-year-old patient, came to the Dental Clinic, Universidade Estadual de Feira de Santana, complaining of a "hole in the mouth" and when he had mouthwashes there was water coming through the nose. He had been submitted to dental extraction of unit 26 (1st upper molar on the left) 7 months before (Figure 2a). The patient presented acute maxillary sinus sinusitis and during the radiological study (ortopan-tomogram) we confirmed the lost of continuity of the floor of the left maxillary sinus (Figure 2b). We suggested closure of the fistula using a connective tissue free graft removed from the palate (opposite side). We made an incision at the level of the fistula and advanced the flap by vestibular and palatine plans, new circular incision pushing the tissue that had been cut and accommodating it in the sinusal cavity with a nylon thread (1st plan suture) (Figure 2c). Incision of the donating area and removal of connective tissue (Figure 2d). It was placed in sterile solution and later positioned on the area. Sutures of the reception and donating area of the graft (2nd plan suture). The suture was removed 15 days later. The patient was observed for 6 months after the surgery and had no signs of recurrence (Figure 2e).

Figure 2a. Clinical aspect of fistula.

Figure 2b. Panoramic x-ray of the maxillary sinus.

Figure 2c. Vestibular, palatine flap and suture on the first plan of sinusal mucosa.

Figure 2d. Connective tissue flap aspect.

Figure 2e. Postoperative aspect 21 days later.
CASE REPORT 3
Female 64-year old patient, came to the Dental Clinic, Universidade Estadual de Feira de Santana, complaining of "water going down the tooth" and that when she sneezed, she felt a foul odor. The clinical examination revealed presence of orifice in the area of extracted tooth unit 16 (1st upper molar on the right) 1 year and 3 months before (Figure 3a). Valsalva's maneuver showed drainage of purulent exsudate. The patient had total edentulous upper arch. The diagnosis of oroantral fistula was confirmed. The treatment proposed to the patient was closure of the oroantral fistula using palatine flap. We harvested a sliding palatine flap at partial thickness. We recovered the oroantral communication using the sliding flap, without suture in both plans (Figures 3b and 3c). Removal of the suture after 15 days. Postoperative investigation after 2 months. The patient has been observed every 6 months and shows no signs of recurrence (Figure 3d).

Figure 3a. Clinical aspect of the fistula.

Figure 3b. Vestibular incision and displacement of fistula.

Figure 3c. Harvesting a pediculated flap.

Figure 3d. Postoperative aspect 4 weeks later.
Concerning the most common location for oroantral communication, we could observe that the topic has been widely debated by the authors. To Krause, Pruzzo, Fonseca, oroantral fistulas are primarily related with 2nd upper molar extractions, followed by 1st molars. The fistulas generated by extraction of the 3rd molars are not frequent and those caused by 2nd pre-molar extractions are very rare. Graziani, conversely, defended that the most frequent accidents occur with the 2nd pre-molars and 1st molars, but it can happen also with other teeth that are connected with the sinus, especially the first pre-molars or 2nd molars. The clinical cases reported here presented preference for the 1st molar region, in agreement with Graziani; Rezende, Heitz.
As to etiological factors, most authors (Car, Juretic; Marzola; Rezende, Heitz; Schow) are unanimous to state that oroantral fistula frequently occurs after extraction of teeth whose roots are in close contact with the sinusal wall, a fact that was found in the reported cases, which presented oroantral communications caused by the same etiological factor reported by them.
Schow pointed some preference to edentulous regions in which there was extensive pneumatization of the maxillary sinus. This situation was detected in the three studied cases in which the oroantral fistula was complicated by maxillary sinusitis and affected edentulous regions, with history of a single tooth that was later indicated from extraction.
As to management of oroantral fistulas and agreeing with Howe, we made acrylic dental plates and a total prosthesis to the edentulous patient (case 3) in the preoperative period, in order to support cleaning of the sinus and prevent food and liquids to go into the area during the meals, and postoperatively to protect the surgical wound from local traumas. Such procedure allows quick granulation and re-epithelialization of the area reducing local pain and fixation of surgical cement, preventing sudden pressures that could lead to dehiscence of postoperative suture.
Authors such as Marzola; Rezende, Heitz agreed that surgical correction of oroantral fistula should wait until the antral infection has been cured.
According to them, the communication will never close unless the antrum is not infected. Cure of sinusitis should preferably be made with clinical methods. Radical surgical approach of maxillary sinusitis should only be used if clinical treatment fails (Graziani; Krause, Pruzzo, Fonseca). Car, Juretic1 emphasized that among the surgical techniques to cure maxillary sinusitis associated with oroantral fistula, Caldwell-Luc access is already dated and we should prefer endoscopic techniques. In the cases reported here we used antibiotics - amoxycillin and potassium clavulanate, as proposed by Schow, together with metronidazole for maxillary sinusitis treatment. The antibiotics were used for 15 days as advocated by Krause, Pruzzo, Fonseca, who recommend proposed treatment with the antibiotics for at least one week. We also used inhalation with eucalyptus, as proposed by Howe, to relieve symptoms. As reported by Rezende, Heitz, we also used daily irrigations of the sinus through the fistula using sterile solution, so as to solve the infection.
The surgical techniques used to close the fistulae are still under dispute in the literature. Some authors advocate the use of rotation of palatine flaps (Rezende, Heitz; Graziani; Martinez, Velásquez), stating that this is the type of flap that is thick and has good blood supply (greater palatine), increasing the chances of success with no risk of tissue necrosis. They do not recommend vestibular flaps because they take to considerable loss of the vestibule fundus, requiring a second surgical intervention; they need wider pedicles since they are irrigated by small blood vessels and frequently the patient is subject to presence of hematomas and infections. In addition, there is the possibility of having facial nerve and parotid damage. Other authors prefer sliding vestibular flap (Howe; Güven) and they ensure that this type of flap does not modify facial contours; the lost vestibule area can be recovered within 8 eights after surgery, and since they are consistent they mean successful approach. The authors contraindicated the use of palatine flaps since they tend to contract when raised from the bone, but consistency and thickness make the position more difficult than with buccal flaps and they also require scarring by second intention of the donating area. A third option is the closure of fistula as advocated by Williams, who uses transplant of connective tissue obtained from the palate of the opposite side of the fistula.
In our cases, we used three types of flaps since the donor site selection is directly related to amount of mucosa necessary to correct the defect without adding tension and ischemia to the harvested flap and without impairment of irrigation. As to use of sliding vestibular flap in case 1, there was no significant loss of the vestibule region. To harvest the palatine flap in clinical case 3, we made relaxation at the base of the flap to easily place it on the desired site, without tensioning it; we succeeded, since we did not observe postoperative tissue necrosis. Using the contralateral connective tissue graft we could observe good first intention scarring both of the donating and the receptive areas.
CLOSING REMARKS1. The most common site of oroantral fistulas is the region of the 1st molar after tooth extractions.
2. Professionals should try to close the oroantral communication as early as possible, since absent of closure of a recent communication may lead to sinus infection, leading to maxillary sinusitis, which can aggravate the clinical picture of oroantral fistula.
3. Valsalva's maneuver is an important part of the clinical examination for the diagnosis of oroantral communications and it should be used whenever indicated by dentists.
4. Surgical correction of the oroantral fistula should wait until complete remission of the antrum infection.
5. All surgical techniques (rotation of palatine flap, sliding vestibular flap, connective tissue free graft, bone grafts, etc.) to close oroantral communications have limitations. The dentist should assess and decide what is the best technique to be employed.
6. One of the main reasons for failure of oroantral fistulae closure is fail to promote a scarring surface in the flap receiving area. Professionals should be aware of that during the surgical act.
REFERENCES 1. Car M, Juretic M. Treatment of oroantral communications after tooth extraction. Is drainage into the nose necessary or not? Acta otorrinolaringol 1998;118(6):844-6.
2. Graziani M. Cirurgia do seio maxilar. In:__. Cirurgia buco-maxilo-facial. 8ª ed. Rio Janeiro: Guanabara Koogan; 1995. p.479-502.
3. Güven O. A clinical study on oroantral fistula. J Craniomaxillofac Surg 1998;26(4):267-71.
4. Howe GL. Extrações e antro maxilar. In:__. Cirurgia oral menor. 3ª ed. São Paulo: Santos; 1990. p.207-23.
5. Krause CF, Pruzzo CE, Fonseca AX. Manejo quirúrgico de la fístula oroantral. Rev otorrinolaringo Cir cabeza cuello 1999;59(2):101-7.
6. Martínez FH, Velásquez JOR. Comunicación oroantral por extracción dental: presentación de un caso. Rev Sanit Mil Méx 1995;49(3):51-4.
7. Marzola C. Acidentes e complicações da eodontia - profilaxia e tratamento. In:__. Técnica exodôntica. 2ª ed. São Paulo: Pancast; 1994. p.284-9.
9. Rezende RA, Heitz C. Comunicação buco-sinusal e buconasal. In: Zanini SA. Cirurgia e traumatologia bucomaxilofacial. Rio de Janeiro: Revinter; 1990.p. 431-48.
9. Schow SR. Doenças odontogênicas do seio maxilar. In: Peterson LJ et al. Cirurgia oral e maxilofacial contemporânea. 2ª ed. Rio Janeiro: Guanabara Koogan; 1997. p.465-77.
10. Williams PE. Doenças dos seios maxilares de origem odontogênica. In: Krueger GO et al. Cirurgia bucal e maxilo-facial. 5ª ed. Rio de Janeiro: Guanabara Koogan; 1984. p.194-204.
1 Dentist, graduated at Universidade Estadual de Feira de Santana. Master studies on Oral Pathology
under course, Federal University of Rio Grande do Norte (UFRN).
2 Assistant Professor, Discipline of Clinical Dentistry V (bucco-maxillo-facial surgery and traumatology); Master degree in bucco-maxillo-facial
surgery and traumatology, FOP/UPE; Ph.D. studies Stomatology under course (UFPB).
3 Assistant Professor, Discipline of Clinical Dentistry V (bucco-maxillo-facial surgery and traumatology); Specialist in Dental Implants, ABO/BA.
4 Dentist, graduated at Universidade Estadual de Feira de Santana.
Address correspondence to: Jardim Concórdia nº 89 Brotas 40255-070
Tel (55 71) 244-2772/9925-6349 - E-mail: avarelac1@hotmail.com
Article submitted on November 29, 2002. Article accepted on May 15, 2003.


