INTRODUCTIONEpistaxis is a common problem that easily controlled in most of the cases. Most of the episodes of epistaxis are anterior and only occasionally they require intervention with nasal packing. In posterior epistaxis, normally more severe, it can sometimes be difficult to localize the bleeding site. The most common etiological causes are mucous dryness, digital trauma and anti-coagulants, whereas traumas associated with vascular abnormalities are responsible for severe epistaxis in less than 5% of the cases 1.
Internal carotid post-traumatic pseudoaneurysm is an uncommon cause, but it can lead to potentially fatal epistaxis. In a series of 87 patients with intracavernous aneurysm, trauma was identified as the etiological factor in 8% of the cases 2. Despite its rare occurrence, such lesions have high mortality rate. Chambers et al.(3) observed a mortality rate of 30% in a review of 100 cases of internal carotid pseudoaneurysm. The formation of the pseudoaneurysm is a consequence of hemorrhage or hematoma of the internal carotid artery, forming a fibrous tissue wall, which by continuity of the blood pulse suffers weakening and widening, which can lead to rupture 4.
Damage to the intracavernous internal carotid is detected in 1 in each 10,000 hospital admissions secondary to trauma 5. Pseudoaneurysm can present as initial manifestations massive epistaxis, whose course demonstrates a variable period of latency 3. The diagnosis of hemorrhage caused by aneurysm is frequently late owing to the time interval between trauma and epistaxis 6.
CASE REPORTWFS, Caucasian male 19-year-old patient, student, coming from Maua. He was admitted to the ER at Hospital do Servidor Público do Estado de Sao Paulo in September 2001, after head trauma in a motorcycle fall. Upon admission, he presented Glasgow score of 15, without impairment of cranial nerves. Computed tomography (CT scan) revealed the presence of frontal pneumoencephalus, fracture of the larger sphenoid ala, ethmoid bones and right orbit; presence of blood in all paranasal sinuses and cerebral edema. He remained hospitalized until stabilization of the clinical picture, presenting cerebrospinal fluid (CSF) leak on day 7, when he was submitted to lumbar puncture and complete resolution of the affection. He asked to be discharged and preferred the repair of the zygoma fracture as outpatient follow-up. He presented an episode of nasal bleeding of small amount with spontaneous resolution on day 10 after hospital discharge.
He came back to the ER in March 2002, transferred from another service, in which he received a blood transfusion and volemic reposition after abundant nasal hemorrhage from the right nasal fossa. Upon admission, he showed good general status, pallor, no nasal or oropharyngeal bleeding, and he was hospitalized with suspicion of internal carotid artery pseudoaneurysm. Flexible nasofibroscopy showed the presence of a clot in the right sphenoethmoidal recess, with no other lesions. We conducted paranasal sinuses CT scan with contrast in which we detected expansive lesion centered on the sphenoid sinus on the right, with extension to the middle fossa and ipsilateral cavernous sinus, with peripheral collection of contrast (Figure 1). We ordered magnetic resonance imaging (MRI) of the head to complement the diagnosis. The result was an image compatible with partially thrombosed giant aneurysm of the internal carotid artery on the right associated with sphenoid sinus rhinorrhea, in addition to focal images on the right carotid vascular territory compatible with ischemic lesions (Figure 2). Angiogram showed a large pseudoaneurysm originated from the anterior curvature of the intracavernous segment of the internal carotid artery on the right, occupying the sphenoid sinus (Figure 5); the test of the compression on the common carotid on the right revealed good velamentum of the right middle cerebral and right anterior cerebral arteries. Presence of symmetry in arterial capillary and venous times. Absence of avascular areas, tumor blushes with normal venous drainage. The patient was assessed by the neurosurgery that proposed a bypass between the external carotid artery and the right middle cerebral artery with ligation of the ipsilateral internal carotid artery, which was performed uneventfully. Postoperative control angiogram did not reveal filling of the right internal carotid, with exclusion of pseudoaneurysm (Figure 6).

Figure 1. CT axial section of the paranasal sinuses showing lesion of the sphenoid sinus on the right and peripheral capture of the contrast.

Figure 2. MRI sagittal section showing partially thrombosed giant aneurysm of the internal carotid and sphenoid sinus rhinorrhea.

Figure 3. MRI coronal section showing giant aneurysm of internal carotid artery with extension to cranial middle fossa and ipsilateral cavernous sinus.

Figure 4. MRI axial section showing sphenoid sinus lesion on the right.
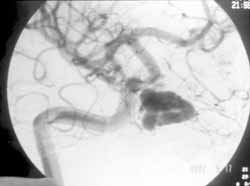
Figure 5. Arteriogram showing large pseudoaneurysm of the anterior curvature of the intracavernous segment of the right internal carotid artery.

Figure 6. Arteriogram conducted postoperatively: no filling of the right internal carotid, with exclusion of pseudoaneurysm.
Most traumatic pseudoaneurysms of the internal carotid artery that result in massive epistaxis are located in the cavernous segment and burst to the interior of the sphenoid sinus; normally, they occur in young male patients involved in car accidents 11, such as in the case reported here. The close relation of the internal carotid with the sphenoid sinus was well described in the anatomic studies with dissection of cadavers by Renn and Rhoton 7. In the study, the internal carotid had a salience to the lateral wall of the sphenoid sinus in 71% of the cases. The bone coverage of the carotid was thinner than 1mm in thickness in 66% of the specimens and 4% were recovered by dura and mucosa of the sinus with absence of bone lamina. The pseudoaneurysm of the intracavernous portion of the internal carotid is close to other cavernous structures and it can be associated with the lesion of cranial nerves 2nd, 3rd ,4th, 5th, and 6th and ophthalmic artery 1, 2. Clinically, the classical symptomatic triad of unilateral amaurosis, orbital fractures and massive epistaxis is almost pathognomonic of internal carotid pseudoaneurysm 8.
Traumatic pseudoaneurysm of the internal carotid resulting in epistaxis normally occurs within the first three months after the initial trauma (88%), however, massive hemorrhage can happen months or years later 9. In a series, 54% of the patients had the first episode of epistaxis within the first months and 87% had it within six months after the trauma 6. Our patient presented severe epistaxis after six months from the initial trauma. Chambers et al. reviewed 100 cases, up to 1981, describing epistaxis resulting from pseudoaneurysm and found 54% had epistaxis within the first month, creating a lag time of 4 months between the initial epistaxis and the diagnosis 3. Late epistaxis can be explained by the time necessary for the traumatic event to weaken the vessel wall and the pulse pressure to erode the bone of the sphenoid sinus 6. Less commonly, pseudoaneurysms can cause rupture of Eustachian tube or posterior nasopharynx 3, 10. Mortality by hemorrhage in such lesions is up to 50% 11.
Despite the fact that carotid angiogram is the ideal method to use in view of vascular damage suspicions, CT scan and MRI are commonly performed after head trauma. Some radiological findings from CT scan and MRI normally have to be further assessed, leading to performance of carotid angiogram. In the MRI, signs of hyperintense T1 /hypointense T2 in the sphenoid sinus suggest presence of blood clot and should lead to angiogram. In addition, MRI can demonstrate the presence of pseudoaneurysm. In CT scan, bone fractures involving the adjacent structures of the sphenoid sinus, sella turcica and orbital apex should make us consider the hypothesis of internal carotid pseudoaneurysm 4, such as in the case reported here, whose CT scan showed multiple fractures, including the skull base. We should bear in mind, however, that pseudoaneurysm can be present in the absence of bone defects. Moreover, a negative CT scan does not exclude the diagnosis. Carotid angiogram normally shows an output of the internal carotid, which is the wall of the pseudoaneurysm. The pseudoaneurysm lumen is normally opaque and gets filled with contrast, but angiograms in initial phase can fail to show the development of the pseudoaneurysm lumen 4.
CONCLUSIONIn any patient that presents posterior epistaxis with previous history of cranial trauma, regardless of how remote the trauma was, we should consider the hypothesis of internal carotid pseudoaneurysm. Moreover, a pattern of recurrent or significant epistaxis with failure to respond to nasal packing should be quickly assessed with carotid angiogram. Other findings such as traumatic amaurosis, cranial nerve deficits and orbital or skull base fracture increase the suspicion of internal carotid pseudoaneurysm. During the confirmation of the diagnosis with angiogram, the internal carotid occlusion test should be performed to assess whether there is the appropriate collateral flow. Diagnosis and early management of pseudoaneurysm are essential to minimize morbidity and mortality of bleeding.
REFERENCES 1. Hoger J. Epistaxis: a clinical study of 1724 patients. J Laryngol Otol 1974, 88:317-27.
2. Higashida RT, Halbach VV, Dowd D, et al. Endovascular detachable ballon embolization therapy of cavernous carotid artery aneurysms: results in 87 cases. J Neurosurg 1990; 72:857-63.
3. Chambers EF, Rosenblum AE, Norman D, et al. Traumatic aneurysms of cavernous internal carotid artery with ssecundary epistaxis. Am J Neuroradiol 1981; 2:405-9.
4. Chen D, Concus AP, Halbach VV, Cheung SW. Epistaxis originating from traumatic pseudoaneurysm of the internal carotid artery: diagnosis and endovascular therapy. Laryngoscope 1998; 108 (3):326-31.
5. Sbeih IA, O'Laiore AS. Traumatic carotid-cavernous fistula due to transection of the intracavernous carotid artery. Case Report. J Neurosurg 1984; 60:1080-4.
6. Han MH, Sung MW et al. Traumatic pseudoaneurysm of the intracavernous ICA presenting with massive epistaxis:imaging diagnosis and endovascular treatment. Laryngoscope 1994; 104:370-7.
7. Renn WH, Rhoton AL. Microsurgical anatomy of the sellar region. J Neurosurg 1975; 66:288-98.
8. Maurer JJ, Mills M, German WJ. Triad of unilateral blindness, orbital fractures, and massive epistaxis after head injury. J Neurosurg 1961; 18:837-40.
9. Hern JD, Coley SC et al. Delayed massive epistaxis due to traumatic intracavernous carotid artery pseudoaneurysm. J Laryngol Otol 1998; 112:396-8.
10. Simpson RK Jr, Harper RL, Bryan RN. Emergency ballon occlusion for massive epistaxis due to traumatic carotid-cavernous aneurysm. J Neurosurg 1988; 68:142-4.
11. Wang AN, Winfield JA, Gunduz G. Traumatic internal carotid artery aneurysm with rupture into the sphenoid sinus. Surg Neurol 1986; 25:77-81.
12. Millman B, Giddings NA. Traumatic carotid-cavernous sinus fistula with delayed epistaxis. Ear Nose Thoat J 1994; 73:408-11.
1 Resident Physician, Service of Otorhinolaryngology/Head and Neck Surgery, Hospital do Servidor Público do Estado de Sao Paulo.
2 Ph.D. in Otorhinolaryngology and Head and Neck Surgery, Federal University of Sao Paulo - Escola Paulista de Medicina
Affiliation - Service of Otorhinolaryngology/Head and Neck Surgery, Hospital do Servidor Público do Estado de Sao Paulo.
Address correspondence to: Rua das Biobedas nº 39 apt. 43 Saúde/ São Paulo CEP 04302-010
Tel (55 11) 5587-4638 / 9670-8206 - Email: macmachado@hotmail.com
Study presented at 36º Congresso Brasileiro de Otorrinolaringologia, held in Florianópolis/SC in November 2002.
Article submitted on February 18, 2003. Article accepted on March 20, 2003.


