INTRODUCTIONHemangioma is the most common of all vascular tumors, histologically benign and normally diagnosed during childhood 4. In the head, its preferred location is the face, oral mucosa, lips and tongue and it rarely affects the uvula 2. Its location can make it vulnerable to bleeding by local trauma 6. Oral cavity and oropharynx hemangioma can also present peculiar difficulties for surgical approach, when indicated, especially owing to the limited surgical access and risk of bleeding 6.
The purpose of the present study was to report a case of obstructive uvula hemangioma in a young adult effectively treated with surgical resection en bloc with radiofrequency knife and to review the characteristics related to hemangiomas and vascular malformations.
CASE REPORTMale, Afro-descendent patient, student and aged 21 years, reported sensation of foreign body in the throat for 2 years, with progressive worsening, especially for the past months, which led to oropharyngeal dysphagia. He did not report bleeding, pain or fever. No significant past medical history. Criteria for inclusion in the risk group for sexually transmitted diseases were absent.
The oropharyngeal examination revealed large volume uvula with irregular surface, presenting an angiomatous lesion, dark violet, that affected the whole extension, with soft consistency and non-painful upon palpation (Figure 1). Upon inspecting it with posterior rhinoscopy and careful palpation of the soft palate and the tumor, it was suggested that the diagnosis would be cavernous hemangioma limited to the uvula. The physical examination including cervical and facial areas did not show any abnormalities. A computed tomography study (CT scan) with and without contrast was ordered and it did not modify the initial impression. HIV serology was negative.
The patient was submitted to surgery under general anesthesia with nasotracheal intubation. We proceeded with en bloc resection of the uvula using radiofrequency knife with minimum intraoperative bleeding. The patient had good postoperative progression. Outpatient follow-up revealed good surgical results (Figure 2). Histopathology analysis revealed the diagnosis of cavernous hemangioma (Figure 3).

Figure 1. Oropharyngoscopy revealed impairment of the uvula all over the lesion of vascular nature, with bag-of-worms aspect, suggestive of cavernous hemangioma.

Figure 2. At postoperative oropharyngoscopy, there was absence of vascular lesion and complete scarring of the surgical wound.
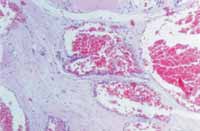
Figure 3. Histopathology shows ectasic vessels, thin vascular wall, intertwined with fibrous tissue.
HEMANGIOMA AND VASCULAR MALFORMATION
Hemangioma is the most common of all vascular tumors 4. It is the most frequent tumor in childhood with about 73% of the cases diagnosed within the first year of life 7. It is estimated that it affects 1% of Caucasian children 1, being more frequent in Caucasian that in Afro-descendents 4, with 3 times greater prevalence in female patients. Hemangiomas are more common in the head and neck 1, even though they can affect any other body segment.
Initially, the hemangioma appears as a macular circumscribed area or telangiectasia located on the skin and/or mucosa in children, especially during the first six weeks of life. It can also have deeper origin, sub-tegumentary or involve internal organs. The lesion can present quick post-natal growth, histologically designated as proliferative phase 4, 7, characterized by marked endothelial hyperplasia, frequently developing throughout some months, which is followed by a slow period of remission, named involutive phase, which normally comprises five to eight years 4 and involves progressive deposition of fibrous-fatty stroma on the vessels with better-defined endothelial wall and lumen. This biphasic pattern represents an important parameter in the nosological differentiation between hemangioma and vascular malformation per se 4. The latter is present at birth and develops according to the child's growth rate, even though it can abnormally increase after local trauma, infection, iatrogenesis or hormone affections. The Port White-type cutaneous mucosa lesion observed in Sturge-Osler-Weber syndrome is an example of vascular malformation, as provided by the biological classification of vascular anomalies proposed by Mulliken and Glowacki5.
Even though there is controversy, another important classification divides hemangiomas into capillary, cavernous and mixed 1, 7. The first group is characterized by small capillary vessels with thin vascular wall, limited normally by a single endothelial layer. Clinically, they can prove to be superficial lesions, shallow and pinky-reddish, of firm consistency, frequently presenting some degree of lobulation, which is associated with marked red color, which led some authors to described it as raspberry hemangioma. As a result of the involution, they develop a darkened aspect and later they become gray and pale, associated with progressive tissue fibrosis. In turn, cavernous hemangiomas comprise thick wall vessels of larger caliper, irregular and with tendency to locate deeply relative to the cutaneous mucous tegumentum; they can affect internal organs and the central nervous system. Upon physical examination, the limits are less defined and the consistency is soft upon palpation, but the tumors get pale upon touch. They may expand with maneuvers that promote greater venous filling, such as Valsalva's maneuver. It has been described by some authors as a bag of worms 1. Finally, the hemangioma classified as mixed, which has common characteristics of both described forms.
Currently, especially after the study by Mulliken, some authors believe that the terms deep and superficial hemangioma replace the classical classifications of cavernous or capillary, respectively, because according to them, the individual characteristics of the hemangiomas described by the classical classification would be less accurate in clinical practice. When the lesion involves concomitantly superficial and deep layers of the skin and mucosa it would be classified as being mixed or capillary-cavernous.
Most of the hemangiomas can be diagnosed with clinical examination. Similarly, clinical history and physical examination are enough to differentiate a hemangioma from vascular malformations in about 95% of the cases 4. Other vascular tumors, such as Kaposi's sarcoma, can be included in the differential diagnosis, especially in risk group patients.
Hemangiomas can present complications such as ulceration, hemorrhage, infection, thrombocytopenia, promote states of high cardiovascular output, esthetic deformities and functional impairment of the airways, digestive tract and phonation system. Location, size of lesion, histology characteristics and cytodynamic behavior are some of the facts that can influence the onset of such morbidities.
DISCUSSIONConsidering the studied literature, it was concluded that the case reported here is atypical. Hemangiomas are rarely observed exclusively in the uvula region. Some demographic characteristics of the patients include race, age range and gender, which are not frequently observed in cases of hemangioma.
Pathological angiomatous growth of the uvula, starting in adult life, within a relatively short period, could result from previous vascular venous malformation, with quick expansion caused by local trauma, infection or hormone abnormalities, as described before, or hemangioma with clinical repercussion in an young adult. The present case clinical examination was strongly suggestive of cavernous hemangioma of the uvula.
Even though Kaposi's sarcoma is part of the differential diagnosis of vascular lesions of the oral cavity or oropharynx in risk group adults, the personal history and physical examination of the patient did not suggest this diagnosis, which was later confirmed by HIV negative serology.
Therefore, the patient studied here presented a vascular lesion in an uncommon location, with progressive development and complicated by functional impairment of swallowing associated with foreign body sensation in the throat.
Complementary tests in hemangioma assessment may include imaging studies with CT scan, MRI , angioresonance or arteriogram. Ultrasound with doppler intravascular flow can also be indicated in some cases and provides useful information about the limits of the lesion and intra-tumor venous flow, when executed by experienced hands. CT scan can be especially useful in assessing the intra-bone lesions. In the case studied here, the clinical examination did not require comprehensive further exams, which were limited to CT scan. Conventional arteriogram exposes in detail the vascular bed and can be therapeutically used for selective embolization. However, MRI presents high accuracy in assessing vascular lesions, delimiting them and providing further information about vascular flow 5.
In turn, the treatment of hemangioma is variable and can be customized. The therapeutic options are watch and see management, surgery, definite or preoperative embolization, laser, cryotherapy, radiotherapy or sclerotherapy, in addition to drug treatment with corticoids or fibrinolytic agents 1, 6, 7.
In our case, total uvulectomy with radiofrequency knife was safely performed thanks to the circumscribed aspect of the tumor, with minimum bleeding, resulting in immediate and complete remission of symptoms. The clinical pathology confirmed the diagnostic suspicion of cavernous hemangioma.
CLOSING REMARKSEven though rare, uvula hemangioma whose differential diagnosis is with vascular malformation and other angiogenic tumors, in addition to the potential difficulties of the surgical approach, can determine obstructive oropharyngeal symptoms and represent an imminent risk of bleeding, especially if extensive and not limited to the organ. In a circumscribed impairment of the uvula, surgical resection of the hemangioma using radiofrequency proved to be a safe and effective therapeutic alternative.
ACKNOWLEDGMENTWe would like to thank Dr Paulo Athanázio and Daniel Athanázio, with the Service of Clinical Pathology, Hospital das Clínicas, Federal University of Bahia, for their valuable contribution in preparing the photos and selecting the slides.
REFERENCES 1. McGill TJI, Forsen JW, Mulliken JB. Hemangiomas and vascular anomalies of the head and neck. In: Cummings CW, Fredricson JM, Harker LA, Kauser CJ, Richardson MA, Schuller DE. Otolaryngology-Head & Neck Surgery (Pediatric). 3rd edition. St. Louis: Mosby; 1998. p. 66-80.
2. Carmi G. Clinical and histopatological considerations on an unusual case of hemangioendotelioma of uvula. Otorinolaringol Ital 1967;36(4):319-32.
3. Murphy JB. The management of a large hemangioma of oral cavity with cryoterapy. J Oral Med 1976;33(3):104-6.
4. Waner M, Suen JY, Dinehart S. Treatment of hemangiomas of head and neck. Laryngoscope 1992;102:1123-32.
5. Bartlett JA, Riding KH, Salkeld LJ. Management of hemangiomas of the head and neck in children. J Otolaryngol 1988;17(2):111-20.
6. Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: a classification based endothelial characteristics. Plast Reconstr Surg 1982;69: 412-18.
7. Hassard AD, Byrne BD. Arteriovenous malformations and vascular anatomy of the upper lip and soft palate. Laryngoscope 1985;95:829-32.
1Collaborating physician, Service of Otorhinolaryngology, Hospital das Clínicas - Federal University of Bahia.
2Collaborating physician, Service of Otorhinolaryngology, Hospital das Clínicas - Federal University of Bahia.
3Coordinator, Division of Head and Neck Surgery, Service of Otorhinolaryngology, Hospital das Clínicas - Federal University of Bahia.
4Ph.D., Professor, Discipline of Otorhinolaryngology, Medical School, Federal University of Bahia and Head of the Service of Otorhinolaryngology, Hospital das Clínicas, Federal University of Bahia.
Study conducted at the Service of Otorhinolaryngology, Hospital das Clínicas - Federal University of Bahia.
Address correspondence to: Fernando P. G. Sobrinho, Cd. Rec dos Pássaros, R3, B29-A, Ap.301, Cabula, CEP: 41150-050 - Salvador.
Tel (55 71): 257-0226 - E-mail: fpgsobrinho@bol.com.br
Article submitted on September 25, 2002. Article accepted on November 07, 2002.


