IntroductionSalivary glands, specifically the parotid and submandibular glands, are anatomically associated to the facial nerve and its branches. If it were not for that, surgical treatment of the affections to these glands would be technically simple. However, parotidectomy and submandibular gland resection bring a risk of neural lesion with significant esthetical-functional sequelae for the patients. Simple exposure and manipulation of the nerve may result in temporary paralysis, causing anxiety to the surgeon and patient.
We have observed a higher risk of temporary facial paralysis in parotidectomy caused by inflammatory diseases comparing to parotidectomy caused by tumors. The duration of paralysis is longer, up to 3 months after the surgery. Bates1 reported an incidence of 29% of temporary facial paralysis after parotidectomies for sialoadenitis. Such a fact is due to more careful and traumatic dissection of the motor branches of the facial nerve caused by fibrosis in the operative field. In addition, the dissected nerve is exposed to inflammatory processes of the adjacent tissues, sometimes with associated infections.
Submandibular gland is the salivary tissue most frequently affected and removed during inflammatory processes. Goh4 reported that most surgeries of submandibular glands - 60% are caused by inflammatory process. Despite the fact that unilateral removal of submandibular gland is associated with reduction in salivary flow at rest and increase of subjective xerostomia, according to Cunning2, exeresis of the gland is an effective and frequently used procedure for the treatment of chronic sialoadenitis, associated or not to sialolithiasis 3.
Traditionally, it is recommended that the mandibular branch of the facial nerve along the mandibular rim be identified before the surgical removal of the submandibular gland. Hald5 reported that neuropraxia of the mandibular branch is a frequent post-surgical finding. Ichimura6 reported an incidence of facial dysfunction of 29.8% and that paralysis was more frequent in cases in which the nerve was identified, comparing to cases in which it was not.
The monobloc removal of the gland, with fat tissue and lymph nodes from the submandibular triangle with sacrifice of facial vessels, advocated in the treatment of neoplasias, does not affect the surgery for sialoadenitis. The parenchyma of the compromised gland must be eliminated.
For these reasons, we started in our service the subcapsular resection of submandibular gland for cases of sialoadenitis associated or not to sialolithiasis. The purpose of the present study was to show the technique we used and our experience in its application.
Material and MethodWe selected patients who had chronic sialoadenitis, associated or not to sialolithiasis. We excluded cases whose preoperative fine needle aspiration biopsy suggested neoplasic process. Patients who raised neoplasic suspicion during surgery were also excluded. In such cases, we followed the traditional procedure, with identification of the mandibular branch of the facial nerve, sacrifice of the facial vessels and en bloc removal of the submandibular gland with the fat tissue and the lymph nodes of the submandibular triangle. Five adult patients underwent subcapsular resection of the submandibular gland, divided into 3 male and 2 female patients with no other significant pathology.
The procedure was conducted under general anesthesia, patient on cervical extension. We performed a 6cm-transversal incision, parallel to the mandibular rim and 4cm below it, from the level of the mandibular angle, including skin, subcutaneous and muscle platysma (Figure 1). The dissection continued to identify the lower part of the gland. At this level, the capsule was opened and the glandular parenchyma was released from it, showing its multilobular aspect (Figure 2). The facial vein was identified on the lateral side of the gland and easily preserved and put aside (Figure 3). On the facial artery, we identified deeper the vein, which had a close correlation with the glandular parenchyma. Its preservation and placement on the side requires that the branches to the submandibular be carefully ligated. The dissection on the superior portion of the gland should be conducted close to the parenchyma, without violating the capsule, but avoiding lesion to the mandibular branch of the facial nerve. The mandibular branch was not identified, protected by the capsule and the areolar tissue, reducing the likelihood of trauma by the extender. The gland was removed after the ligation and section of the Wharton's duct and branches of the lingual nerve to the submandibular. We left a suction drain and closed the planes including the platysma muscle, subcutaneous and skin layers. The drain was removed within 24 to 48 hours and the stitches, 7 days later.
ResultsThe procedure lasted in average 40 minutes and it is normally less than what is required for a conventional surgery. The difference is due to time saving in identification and protection of the submandibular branch, which is the tensest part of the conventional procedure.
No patients presented motor disorders of the facial region. One patient presented temporary reduction of ipsilateral hemitongue. He presented severe inflammatory process with fistulation on the posterior region of the floor of the mouth. It required vigorous retraction of retractors for surgical exposure and laborious dissection of the lingual nerve. Despite that, he did not have mandibular branch paresis of the facial nerve.
Pathology of all cases confirmed the chronic inflammatory condition. Postoperative evolution was satisfactory in all cases with resolution of the preoperative symptoms that forced the patient to undergo surgery.
Figure 1.
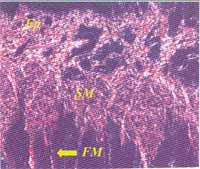
Figure 2.
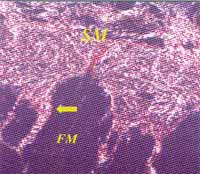
Figure 3.
Currently, in all surgical areas, there is a trend towards carrying out procedures called functional8, avoiding unnecessary trauma. The purpose is to minimize surgical morbidity without reducing cure rates.
However, in the treatment of salivary neoplasia, even in benign ones such as pleomorphic adenoma, we should avoid conservative procedures such as enucleation. Results are compromised because of the comparison of recurrence rates with the conventional procedure10. In such pathologies, we recommend as minimum procedure superficial parotidectomy or resection of submandibular gland with peripheral areolar tissue.
In inflammatory diseases, we can try more conservative approaches. In cases of single stone on the distal portion of Stenon's duct or Wharton's duct, we can proceed to removal with orifice plasty 9. If there are chronic inflammatory processes affecting the glandular parenchyma and clinical picture of repetitive infections with no satisfactory response to clinical treatment, the surgical alternative is to remove the impaired gland.
In the case of chronic submandibular sialoadenitis, the subcapsular removal of the gland is a technically attractive option because there is no exposure of the mandibular branch of the facial nerve, preventing its manipulation. In addition, the mandibular branch is protected by a fat mass, reducing the risk of trauma by the retractors. The surgical duration is normally shorter, because some tense minutes are saved once we do not have to identify and release the mandibular branch.
Another advantage is the preservation of facial vessels. Despite the fact that the sacrifice of these vessels does not represent immediate sequela to the patient, they are the basis for various face and neck flaps7, which may be necessary for future reconstructions. They are also frequently used for anastomosis of microsurgical flaps.
Subcapsular resection also reduces the volume of the removed tissue. It minimizes cervical asymmetry, an evident esthetical advantage.
The most delicate part of the procedure is identification and ligation of the branches of the facial artery to the submandibular gland. The artery is in close contact with the gland and the branches are shorter. If there is excessive tension, they are easily ruptured causing unnecessary bleeding.
Despite the limited number of patients, the procedure proved to be advantageous, since there were no cases of postoperative facial paresis. In our experience, this result would not have been the same if we had used the conventional procedure. Even in the case that had a floor of the mouth fistula, in which we had to energetically use the retractors, the patient had no facial motor dysfunction.
Pre and trans-operative assessments proved to be very effective since there were no results of neoplasia, according to the pathology, dissected by the subcapsular technique. This fact is due to strict indications, since there were cases operated on with the conventional method whose pathology revealed inflammatory process.
ConclusionSubcapsular resection of submandibular gland proved to be technically feasible for the surgical treatment of chronic sialoadenitis. The advantages were smaller risk of temporary paresis of facial mandibular branch, shorter surgical act, preservation of facial vessels and smaller cervical postoperative asymmetry.
The indication of the technique should be carefully made pre and postoperatively in order to avoid its use in cases of neoplasia. In such situations, the use of the procedure may result in higher recurrence rate than the traditional method.
References1. BATES, D.; O'BRIEN, C.J.; TIKARAN, K.; PAINTER, D.M. - Parotid and submandibular sialadenitis treated by salivary gland excision. Aust N Z J Surg, 68(2):120-4, 1998.
2. CUNNING, D.M.; LIPKE, N.; WAX, M.K. - Significance of unilateral submandibular gland excision on salivary flow in noncancer patients. Laryngoscope, 108(6):812-5, 1998.
3. ELLIES, M.; LASKAWI, R.; ARGLEBE, C.; SCHOTT, A. - Surgical management of non-neoplastic diseases of the submandibular gland. A follow-up study. Int J oral Maxillofac Surg, 25(4):285-9, 1996.
4. GOH, Y.H.; SETHI, D.S. - Submandibular gland excision: a five-year review. J Laryngol Otol, 112(3):269-73, 1998.
5. HALD, J.; ANDREASSEN, U.K. - Submandibular gland excision: short and long-term complications. ORL J Otorhinolaryngol Relat Spec, 56(2):87-91, 1994.
6. ICHIMIURA, K.; NIBU, K.; TANAKA, T. - Nerve paralysis after surgery in the submandibular triangle: review of University of Tokyo Hospital experience. Head Neck, 19(1):48-53, 1997.
7. JACKSON, I.T. - Local flaps in head and neck reconstruction. Mosby, St. Louis, 1990.
8. MATTOX, D.E.; GOLDSMITH, M.M.; CASTELLANOS, P.F. - Minimally invasive surgery; in: CUMMINGS, C.W. (editor) Otolaryngology-Head and Neck Surgery, second edition, update I. Mosby, St. Louis, 1995.
9. RONTAL, M.; RONTAL, E. - The use of sialodochoplasty in the treatment of benign inflammatory obstructive submandibular gland disease. Laryngoscope, 87:1417-21, 1987.
10. SNYDERMAN, N.L.; SUEN, J. - Benign salivary neoplasm, in: CUMMINGS, C.W. (editor) Otolaryngology-Head and Neck Surgery. Mosby, St. Louis, 1986.
Clinic of Otorhinolaryngology, Hospital Governador Israel Pinheiro - IPSEMG, Belo Horizonte/MG.
Address correspondence to: Avenida do Contorno 9215 sala 802, Belo Horizonte/MG - 30110-130
Tel.: (55 31) 291.8288 Fax: (55 31) 3375398.
Article submitted on March 08, 2001. Article accepted on August 15, 2001.


