INTRODUCTIONThe antrochoanal polyp (ACP) is a benign lesion arising from the maxillary sinus mucosa through the ostium, that reaches the choana via the internal naris and nasopharynx, and may extend to the oropharynx.
1 It comprises 4% to 6% of nasal polyps and is usually unilateral; bilateral cases are extremely rare.
1-4 It was initially reported by Palfyn in 1753, but Killian meticulously detailed it in 1906, describing its site of origin as the maxillary sinus.
2,5 The usual clinical manifestation is nasal obstruction, and it may be associated with posterior discharge, nasal secretions, snoring, foreign body sensation, halitosis, and rarely, dysphagia or dyspnea.
1,2 Epidemiologically, it affects more men and children.
1-5 CASE PRESENTATIONCRS, a 48 years old male patient, presented with approximately 30 years of bilateral nasal obstruction that was worse on the left, in addition to rhinorrhea, hyposmia, and difficulty sleeping. He denied cacosmia, headaches, and atopic or otological complaints. He also denied smoking or alcohol consumption, allergy to non-steroidal anti-inflammatory drugs, asthma, and other comorbidities.
Nasofibroscopic assessment disclosed a polypoid mass completely occluding the nasal cavity bilaterally. Computed tomography (CT) scan of the sinuses disclosed soft-tissue masses in both nasal cavities, larger on the left side, that extended to the choanae (Fig. 1A); bilateral enlargement of the ostiomeatal complex; partial opacification of the cells of the maxillary, ethmoid, and frontal sinuses; and left sphenoid mucosal thickening.
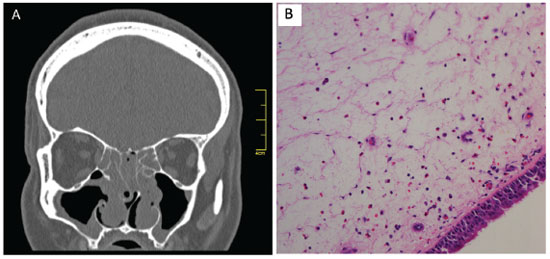
Figure 1 A, Computed tomography of the paranasal sinuses. Coronal section showing the polyps occupying the nasal cavities bilaterally, with opacification of the ethmoid sinuses due to retention of secretion and insertion of antrochoanal polyps in the medial wall of the maxillary sinuses bilaterally. B, Histological photograph at a 100 × magnification stained with hematoxylin and eosin, demonstrating antrochoanal polyp with pseudostratified cylindrical epithelium, discreet superficial inflammatory infiltrate, and occasional eosinophils.
Surgery was performed exclusively by nasal endoscopy. The intraoperative findings were limited to a single large polypoid mass in each nostril, arising from the medial wall of the maxillary sinus and extending to each choana; a right middle concha bullosa; edema, and retained secretions in the anterior and posterior ethmoid cells.
Pathological assessment showed a 5.0 × 2.0 × 1.0 cm polypoid lesion on the right and a 5.0 × 2.5 × 1.0 cm on the left, covered by respiratory epithelium without goblet cell hyperplasia or basal membrane thickening, with grade 3 edema and grade 1 fibrosis of the stroma, discrete mixed infiltrate with a neutrophile count of four per field and four to six eosinophils per field, with no signs of malignancy, consistent with the diagnostic impression of antrochoanal polyps (Fig. 1B).
The patient experienced a complete recovery with resolution of complaints and no recurrence four months postoperatively.
DISCUSSIONCases of bilateral ACP are extremely rare: only eight reports have been documented in the literature until July, 2012.
2-4 The etiology of ACP remains unclear; it has been speculated that the origination is from a maxillary cyst that enlarges near the maxillary ostium. The Bernoulli effect, caused by the respiratory airflow perpendicular to the ostium, would cause the lesion to extend into the nasal cavity.
1,2 The association between ACP and chronic rhinosinusitis has been documented, but the factors of cause and effect remain controversial.
1,5 The gold standard for ACP diagnosis is nasofibroscopy associated with CT scan documenting a polypoid mass arising from the maxillary sinus, enlargement of the ostiomeatal complex, and extension of the mass into the choana.
1-5 The posterior wall of the maxillary sinus is the most common site of origen. The lesion presents two macroscopically distinct parts: an intrasinusal cystic portion and a solid intranasal portion.
1,2,5 Microscopically, ACPs are covered with normal respiratory epithelium and exhibit stromal edema.
1,2,5,6 There are clear differences compared to inflammatory polyps: ACPs have less inflammatory infiltrate, significantly less eosinophilic infiltration, fewer submucosal glands, and a more fibrosis stroma.
1,2,5,6 These findings are consistent with the clinical, radiographic, and histopathological picture of the present patient, confirming the diagnostic impression of bilateral ACP. Endoscopic surgical removal is the preferred therapy, whether or not associated with an external surgical approach to prevent recurrence.
1-5 FINAL CONSIDERATIONSBilateral ACP is extremely rare, but it must be included in the differential diagnosis of chronic rhinosinusitis with polyps. A biopsy is mandatory in for histopathological confirmation.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.
REFERENCES1. Yaman H, Yilmaz S, Karali E, Guclu E, Ozturk O. Evaluation and management of antrochoanal polyps. Clin Exp Otorhinolaryngol. 2010;3:110-4.
2. Frosini P, Picarella G, De Campora E. Antrochoanal polyp: analysis of 200 cases. Acta Otorhinolaryngol Ital. 2009;29:21-6.
3. Sousa DW, Pinheiro SD, Silva VC, Bastos JP. Bilateral antrochoanal polyps in an adult. Braz J Otorhinolaryngol. 2011;77:539.
4. Freitas MR, Giesta RP, Pinheiro SD, Silva VC. Antrochoanal polyp: a review of sixteen cases. Braz J Otorhinolaryngol. 2006;72:831-5.
5. Maldonado M, Martínez A, Alobid I, Mullol J. The antrochoanal polyp. Rhinology. 2004;42:178-82.
6. Min YG, Chung JW, Shin JS, Chi JG. Histologic structure of antrochoanal polyps. Acta Otolaryngol. 1995;115:543-7.
1. Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo (USP), Ribeirão Preto, SP, Brazil
2. Department of Otorhinolaryngology, Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo (USP), Ribeirão Preto, SP, Brazil
3. Pathology Service, Hospital das Clínicas, Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo (USP), Ribeirão Preto, SP, Brazil
Corresponding author.
H.A.C. Sabino
E-mail:
hensabino@yahoo.com.brReceived 5 August 2012.
Accepted 6 January 2014.


