IntroductionSilicosis is a nodular lung fibrosis that develops following the inhalation of crystalline silica dust (SiO2), and is the most common and severe pneumoconiosis2.
This disease is reported worldwide, particularly in people that were closely exposed to free silica whichsilica, which exists in great variety in nature. The most important source of this silica is quartz. The disease has been described since ancient times and the facts that determine its severity and outcomes are namely exposure time, individual susceptibility and environmental care for individuals under exposure. 4.
When the ore containing silica is heated to temperatures higher than 1,.000º C and sprayed to size smaller than 5 micra, it becomes more pathogenic. Particles larger that 5 micra are captured by mucociliary transport of the upper airways. Particles smaller than 0.5 micra remain in suspension and are exhaled3.
More than 80% of particles larger than 6 micra are eliminated through vibrissae of the nostrils or by the mucociliary transport of the upper airways in few hours3.
Among the activities considered risky we found: mining, tunneling, stonework, manufacturinge of ceramics and china, refractory and abrasive materials, foundry work, sand blasting . 2.
The same materials that contain small amounts of silica can be hazardous if used in environments that generate high content of dust 2. The small particles that pass the nasal cavity reach the lung alveoli and penetrate the lung interstitium are phagocytosed by the macrophages that are grouped in nodules in the lymphatic structures; free silica has a selective toxic effect on these macrophages that are lysated. Next, a series of biological reactions result in the formation of a characteristic nodule with proliferation of fibroblasts and collagen fiber. The continuous deposition of SiO2 and the destruction of the macrophages generate fibrogenesis and hyaline deposition. This hyaline substance is formed by antigen-antibody and complement 2.
The larger part tof silica that reaches the lung is removed by mucocialiary transport 1.
Macroscopically the silicotic lung nodule is better palpable than visible, and is similar to a sand grain 3.
The silicotic nodule diameter ranges from 0.3 to 1.5 mm, and presents a clear histological appearance, rounded or star-like shape, its nucleouus is formed by fiber-hyaline tissue. The peripheral region is clearly differentiated from the nucleous with the reticular fibers, macrophages, fibroblasts, lymphocytes and plasmocytes. The nodules may become confluent and form rounded masses of 1cm diameter3.
The observation of birefringent crystals of silica in the nodules is key for differential diagnosis, which is performed with polarized light microscope. 3.
The major factor of collagen fiber production remains unknown, however there is the assumption that it is the "fibroblasts stimulation factor" released by the macrophages that phagocytosed the silica. Nevertheless, immune mechanisms may act, since it is known that patients that develop silicosis normally present an increase of blood rheumatoid factor and anti-nuclear antibody3.
Patients with silicosis and frequency of with exposure frequency higher than normal present an increase of the antinuclear antibodies with increased prevalence of the association with rheumatoid arthritis, scleroderma and systemic lupus eryithrematosus 2.
Disease symptoms depend on the exposure dose and period, in addition to individual susceptibility; the symptoms may appear in some weeks in cases of long and heavy exposures, and some patients may be asymptomatic for 10 years or more.; There is not an specific therapy for silicosis, but only management of complications2.
Depending on dose and lag period since onset of exposure Silicosis forms that may occur are as follows1:
1. Chronic: most commonly found in lowight level exposure to crystalline silica, for more than 10 years.
2. Accelerated: shorter, high level eavy exposure for 5 to 10 years.
3. Acute: generally in young adults under heavy exposure of very small particles even for short time: it is believed that there is a significant immune role that leads to respiratory insufficiency in few months.
Other diseases are associated to the inhaling silica dust such as bronchitis, tuberculosis, and lung cancer. 2
Although the disease is prevalent all in over other parts of the world, the researched literature did not provide any description of nasal mucosa impairment with silica granuloma formation.
Case reportThe patient, CRG, a 46- year- old female housewife from SSão Paulo arrived at our care center in April 1996. C.R.G.
The patient began to notice a fall of the nasal dorsum three years beforeago, which evolved to the current condition, and has remained unchanged for two years. During this time there was only a mild nasal obstruction; the patient had bloody secretion when blowing cleaned her nose. She denied any other otorhinolaryngologiycal symptom or local trauma. The patient smokeds 20 cigarrettes a day and denied any infectious process or contact with risk groups or drug users. Physical examination showedreported a depression of the nasal dorsum on the upper side cartilage junction with the nasal bones; in the nasal cavity the nasal septum presented an ulcerated area with granulous bottom and lined with fibrin in areas II and III.0 (Figures 1 to 5).
With clinical hypothesis of graunummalomatous ulcer disease the patient underwent syiphifilis blood test, Montenegro test, direct test of fungi, test of bacilli resistance to alcohol/acid by the method of Ziehl-Nielsen and complete blood counttest , all within normal range.esults.
CT scan of the paranasal sinuses presented a mild hypodense area in the right frontal sinus. The conventional chest radiographs did not reported any kind of change in the pleuro-pulmonary fields.
Biopsy was performed and the material was sent to pathological anatomy examination: mucosa and upper airway with intense fibrous proliferation and collagen deposition with nodular appearance, having transparent fissures. It also had a lympho-plasmocyitariany infiltrate around the nodules with macrophages and clear cyitoplasm. The observation of this material under the polarized light revealed the presence of typical silica crystals. (Figure 6 to 8)
Diagnosis: nasal mucosa silicosis.
The patient was interviewed about the permanence in environments polluted by agents of any nature that could present a risk. Still the contact with silica containing materials was extensively investigatedresearched, butand any factor that could trigger the disease was not identified.
The patient was instructed to make the nasal lavage only with saline solution at 0.9%.
The patient presented crust formation in the described area until August 1996 when a septum perforation was observed in the ulcerated area; then a new biopsy was then performed with the same result of silicosis in respiratory mucosa. Nasal lavage with saline solution at 0.9% was prescribed to the patient (Figure 9).
From October 1996 on, the patient did not have any tissue granulation in the nasal cavity and did not report any symptoms related to septum perforation, whose that was with its rims were lined by mucosa with a normal appearance mucosa. (Figure 10)
The immune system analysis included aspects such as rheumatoid factor, presence of LE cells , and antinuclear factor for possible relation with autoimmune disease, butand nothing was reported. The patient remained asymptomatic until January 1999, and the external appearance of the nose did not change.
Due to esthetical complains related to the nose saddle, the patient underwent rhinoplasty with a auricular concha graft inserted in the conchae auricular and in the nasal dorsum; a new biopsy was carried out during the procedure and had the same results of the former examinations.
The patient remained asymptomatic until January 2000 and the nasal mucosa does not present any sign of disease activity.(Figures 11 to 14)

Figure 1. Frontal view of the patient.
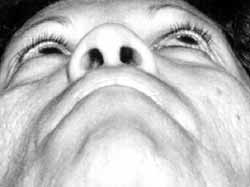
Figure 2. Inferior view of the patient.

Figure 3. Right lateral view.

Figure 4. Left lateral view.
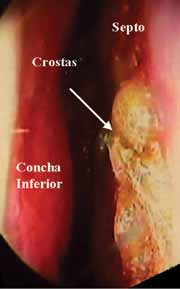
Figure 5. Aspect of the initial lesion, with ulceration area recovered by fibrin.
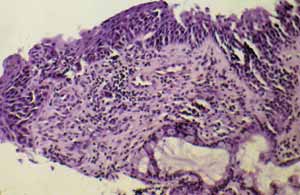
Figure 6. Section of nasal mucosa with silicotic nodule.
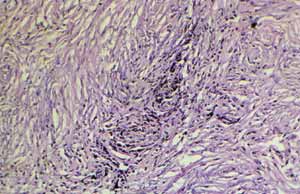
Figure 7. Section of nasal mucosa with marked fibrous proliferation amidst transparent slots.
Figure 8. Section of nasal mucosa observed under polarized light revealing the presence of silica characteristic crystals.

Figure 9. Nasal septum perforation with rims recovered by fibrin.
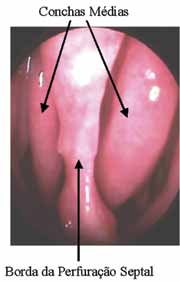
Figure 10. Nasal septum perforation with rims recovered by normal mucosa.

Figure 11.

Figure 12.

Figure 13.

Figure 14.
Although silicosis is a disease spread world wide and described since ancient times according to Rosenman et al.4, the authors did not find any reference in the extensively researched literature extensively researched of nasal mucosa impairment.
The respiratory epithelium of the nasal mucosa is identical to the bronchial epithelium, with differences occurring in the corium structure. It probably explains why the inflammatory process does not occur very often in response to silica in the nasal mucosa; it may be that the immunity of the local nasal mucosa is not stimulated to react to silica, or even crystals do not find a place to be entrapped and phagocytosed. In fact, the nose with all its structures work as a defense, filtering and conditioning the inhaled air; the nasal mucosa can not react to all antigens that come to it and its function is to eliminate them.
The diagnosis is based on a pathological anatomy study in which silica crystals identified under polarized light were found, with other elements that characterized the inflammatory process. This was exactly what was found in the patient's biopsy; the three biopsies had the same results, and the evidence of other related diseases werewas ruled out, including other granulomatous diseases or neoplasmias.
In addition to time and severity of silica exposure, the individual susceptibility is a key factor for the manifestation and development of the disease 2. The patients with silicosis presented an increase of antinuclear antibody with a higher frequency than the normal and increased association to autoimmune diseases; it would be expected that our patient, whichwho was impaired in an unusual region had a major alteration, but the investigation research did not show any anomaly. Also the patient did not have any pulmonary impairmentalteration.
According to Coutinho et al.1, silicosis is divided into three forms in terms of development: chronic, accelerated and acute. If it was possible to make the correlation between the pulmonary disease and the nasal impairment, our patient would be ranked better in the chronic step of the disease, when patients are asymptomatic for long periods and the exposure to silica is not extremely heavy.
There is not a specific treatment for silicosis 2; , the management is based on withdrawing the patient from crystal exposure site and to control likely complications, in addition to constant follow up of patients. Since the patient's first appointment, her major complaint was the esthetical deformity of the nose. Due to the lack of knowledge of the disease, our major goal was to understand it, since it was not widely known by otorhinolaryngologiysts, to manage it properly. Since there is not a specific treatment we unsuccessfully tried to find out the source of exposure, and to observe its development. The treatment was exclusively oriented to local symptoms.
We believe that the patient's silica exposure took place right before the first appointment. This is the reason why that in few months the activity of the disease that had caused septum perforation began to decrease and became quiescent. The patient remained like this for approximately 4 years after the first observation.
Since the first biopsy, the pathologic histology was identical in all samples with no changes reported for severity or type of inflammatory process.
The rhinoplasty was performed via extra mucosa, with detachment isplacement of the perichondrium, and the periosteum of the nasal dorsum, and placement of the auricular conchae autologous graft on the conchae auricular. The patient will continue to be followed up in our outpatient facility for indefinite time with the purpose ofto observinge relapse of the process activity of the process or the onset of another local or systemic disease associated to silica granuloma of the nasal mucosa.
closing remarksNasal silicosis is not a disease not described in the literature yet and as such it lacks the understanding of its physiopathophysiology and development.
This case should not be viewed only as a curiosity, but rather as a unusual impairment of an isolated disease of the nasal mucosa and whoseits pathogenic ability is not clear yet.
References1. Coutinho ZP, Castro HA, Algranti E. Pneumopatias Profissionais. In: Pneumologia, 4a Ed.; 1995. p. 729-743.
2. Mendes R, Carneiro APS. Doenças Respiratórias Ocupacionais. In: Doenças Pulmonares. Guanabara Koogan, 4a Ed.; 1997. p. 807-853.
3. Robbins SL, Cotran RS, Kumar V. EnviromentalEnvironmental Pathology. In: Pathologic Basis Ofof Diseases. WB Saunders Co., 3a Ed.; 1984. p. 767-795.
4. Rosenman KD, Reilly MJ, Kalinowski DJ, Watt FC. Silicosis In The 1990's. Chest 1997;111(3):779-786.
[1] Ph.D., Adjunct Professor, Department of Otorhinolaryngology, Santa Casa de São Paulo.
[2] Post-Graduation under course, Medical School of Santa Casa de São Paulo.
[3] Post-Graduation under course, Medical School of Santa Casa de São Paulo.
[4] Ph.D., Professor and Head of the Department of Pathology.
Affiliation: Faculdade de Ciências Médicas da Santa Casa de São Paulo
Rua Cesário Motta Jr., 112, São Paulo, SP - 01277-900
Tel. (55 11) 222-8405 - Fax (55 11)5051-2165 - E-mail: ivobf@dialdata.com.br


