IntroductionDocumented by Brodie in 1846, Madelung (1888) and Launois and Bensaude (1898)1, it has been addressed by different names, such as annulare colli lipoma, morbus Launois-Bensaude, horse collar and benign symmetric lipomatosis 2. In patients with masses that increase the diameter of the neck, they gradually assume the appearance of "horse collar"1.
The clinical picture is characterized by abnormal fat deposits that affect normally the neck and head region, the upper portion of the trunk and occasionally the upper limbs2. It is frequently followed by hyperurecemia, dyslipidemia, macrocystic anemia, peripheral neuropathy, glucose intolerance, renal tubular acidosis and it is normally associated to alcoholism2, 3, 4, 5, 6.
Symptomatic compression or detachment of the structures such as trachea have been described2.
The fat tissue has hard consistency, is non-painful upon palpation, diffusely distributed and without encapsulation, making it very difficult to resect it surgically2.
Literature ReviewMadelung's disease or multiple symmetric lipomatosis is not a frequent pathology in our society. There is predominance in male subjects who come from Mediterranean regions and who are alcohol abusers2, 4, 7. Cases in women and non-alcoholic subjects have also been described4. Polyneuropathy and myopathy can be severe and normally appear many years after the onset of lipomatosis 6. Neuropathy can be sensorial, motor or autonomic6. The cause of polyneuropathy is unknown. The absence of axonal acute degeneration, typical of alcoholic neuropathy supports the hypothesis that is it not due to alcohol use6. The age range is from 20 to 65 years. The etiology of the disease is unknown, some suggest that there could be a block of the lipolysis induced by lack of catecholamine, with partial or total sympathetic denervation of the fatty tissue; others believe that the cause is in the abnormalities of the autonomic nervous system4, 2. It seems to be associated to genetic abnormalities, being mitochondral dysfunction the essential biochemical defect and compatible with maternal transmission1, 2, 8.
In alcohol abusers, the biochemical abnormalities found are associated to hepatic disorders that result from alcohol intake, the direct effect of the alcohol in the mitochondral metabolism causing fatty metabolic abnormalities with abnormal fact deposit in some specific regions2.
Characteristically, the growth of the fatty tissue during the initial stage of the disease is rapidly progressive, then the course can be variable, normally it remains static, but occasionally it may progress slowly to explosive episodes5. Spontaneous regression is rare5. A single publication reported the use of oral salbutamol that led to reversion of rapidly progressive fatty masses6. Therapy with corticosteroid resulted in quick weight gain, despite some clinical improvement6.
Madelung's disease has been observed in association with diabetes, gout, alcoholism and other systemic diseases, although the concomitance of two diseases in one single patient does not define a relation between them1.
Case ReportCG, 46-year-old Black patient coming from Parana, working as bagging operator, was referred to the service of Otorhinolaryngology by the Digestive Tract Division because of tumor masses on the neck region, with 4 month evolution.
The patient reported dysphagia, dyspnea upon effort and diffuse body pain, especially on the wrists and fingers. He presented systemic hypertension, dyslipidemia and was assuming the appearance of horse collar owing to multiple neck lipomas.
For over 30 years he reported intake of one liter of alcoholic distilled and fermented drinks per day and smoking of 2 cigarette packs a day. He did not report weight loss.
Physical examination: the patient was well developed, well nourished, presenting hard consistency masses, non-painful upon palpation, and with undefined limits of the subcutaneous tissue of the neck region, being: 01 nodule of about 5 cm in the anterior neck region (sternal furcula), one 3cm nodule on the right submandibular region; one 1cm nodule on the right neck region, and another on the left neck region (Figures 1, 2 and 3). There was no morbid obesity and absence of other abnormalities on the physical examination.
Neck CT scan revealed presence of hypodense lesion, homogenous, extensive, with precise periphery and non-infiltrative lesion in the anterior neck region under the platysma and anterior to the infra-hyoid muscle (Figures 4 and 5). The pathology revealed lipoma. Complete blood count was normal. It was decided to perform surgery owing to the symptoms present and the physical deformity, though not very marked, and the surgeon would decide for conventional surgery, lipectomy or combination of both.
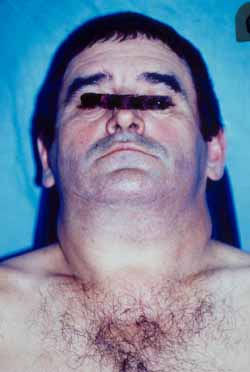
Fig.1

Fig.2
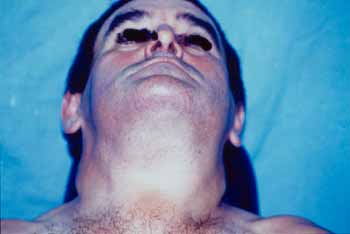
Fig.3
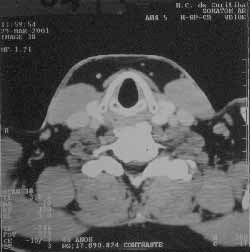
Fig.4

Fig.5
The diagnosis is made by the recognition of a unique clinical appearance, but in atypical cases it may be necessary to differentiate it from lymphoproliferative diseases5. It should be differentiated from morbid obesity, pseudolipomatous states resultant from abnormalities of the lymphatic system and congenital accumulation of fatty tissue observed in some subjects of specific African tribes2.
Masses normally do not respect cleavage plans and penetrate in all levels, making exeresis more difficult2. Surgical excision is difficult owing to the hardened consistency and the extremely vascularized tumor mass, that is why rigorous hemostasis and use of drains are necessary to prevent seroma or formation of hematoma 2, 1. The preferential access route should be direct over the masses, trying to avoid major displacements2. Owing to failure in cleavage plan between the tumor tissue and subcutaneous tissue, the surgery becomes time consuming and dangerous, especially in the regions in which there are key structures2.
Unfortunately, the removal of multiple symmetric lipomatosis has cosmetic and practical benefits that are only temporary7. Thus, frequent surgeries are the treatment of choice7. Although with limited experience in the literature, liposuction seems to come close to ideal to reduce the cosmetic scar normally seen after conventional surgery7.
After surgical removal of tumors, it is common to experience recurrence because they are not well encapsulated4. Weight loss and alcohol abuse interruption do not seem to affect the progression of the disease5, although abstinence seem to help reduce the recurrence rate4.
It is believed by some that liposuction is the easier path to remove the recurrent lipomatous deposits of multiple symmetric lipomatosis 7.
Solitary neck lipomas do not require surgery, except if they cause deformities or mechanical difficulties.
Closing RemarksMadelung's disease is extremely rare and the literature has described only about 200 cases since its first description in 18366.
The diagnosis is based on history, physical examination of masses, lab tests, biopsy and anatomic limits studied by CT scan and treatment is surgical, which can employ lipectomy, liposuction or both, with tendency of disease recurrence.
References 1. Keller SM, Waxman JS, Kim US. Benign Symmetrical Lipomatosis. Southern Medical Journal. 1986 Nov;79(11):1428-9.
2. Gemperli R, Pigossi Jr O., Ferreira MC, Lodovici O. Tratamento cirúrgico da lipomatose simétrica múltipla (doença de Madelung). Revista Paulista de Medicina, 1988 Nov-Dec;106(6): 313-316.
3. Amicucci G, Sozio ML, Rizzo FM, Sozio A. Malattia di Madelung. Minerva Chirurgica. 1998;53:655-7.
4. Gabriel YA, Chew DK, Wedderburn RV. Multiple symmetrical lipomatosis (Madelung's disease). Surgery Jan 2001;129(1):117-8.
5. Wood R. Benign symmetrical lipomatosis - a complication of excessive alcohol consumption. A case report. S Afr Med J. 1990 Apr 7;77(7):369-70.
6. Teplitsky V, Huminer D, Dux S, Learman Y, Zoldan J, Ptlik SD. Multiple symmetric Lipomatosis presenting with polyneuropathy. Isr J Med Sci. 1995. Nov;31(11):693-5.
7. Basse P, Lohmann M, Hovgard C, Alsbjorn B. Multiple symmetric lipomatosis: combined surgical treatment and liposuction. Case report. Scand J Plast Reconstr Hand Surg. 1992;26(1):111-2.
8. Berkovic SF, Andermann F, Shoubridge EA, Carpenter S, Robitaille Y, Andermann E, Melmed C, Karpati G. Mitochondrial Dysfunction in Multiple Symmetrical Lipomatosis. Annals of Neurology. May 1991;29(5):566-9.
[1] Head and Neck Surgeon, Physician of the Service of Otorhinolaryngology, Federal University of Parana.
[2] Resident Physician of the Department of Otorhinolaryngology, Federal University of Parana.
[3] Physician graduated from the Federal University of Parana.
Affiliation: Department of Ophthalmology and Otorhinolaryngology, Hospital das Clinicas, Federal University of Parana.
Address correspondence to: Edeli S. Pepe - Rua Engenheiro Benedicto Sadock de Sá, 310 Bl 05/14 Santa Cândida
Curitiba - PR - 82630-280
Tel: (55 41)256-5738/323-8039/9982-9119 Fax: (55 41) 323-7932 - E-mail: edeli@prpr.mpf.gov.br


