INTRODUCTIONParotid gland parenchyma is subject to changes in its histological characteristics because of local or systemic conditions. Hypertriglyceridemia may be associated with fat infiltration in the parotid without inflammatory activity1. The drop in ovarian hormones after ovariectomy in rats showed fat degeneration in the parotid glands2. In Sjögren's syndrome, there is parenchyma heterogeneity because of adipose degeneration and lymphocytic infiltration3. In patients with the Human Immunodeficiency Virus (HIV), there may be parotid gland enlargement and, histologically, besides the fat infiltration, one may see lymphocytic aggregates, lymphoepithelial cysts or lymphadenopathy4. Moreover, in alcoholics and diabetics, there is a reduction in the rate of fat tissue in the stroma5. On the other hand, studies with rats have shown an increase in lipids and degeneration of secretory granules associated with an age-related decline in the secretory activities of the parotid glands6, without it representing a disease process.
In the stomatology ward of our institution, we had patients in whom we saw an increase in the volume of the parotid glands, eventually associated with complaints resembling those of a Sjögren's syndrome, but after broad diagnostic investigation, such condition was ruled out, based on current diagnostic criteria (European-American Consensus, 2002)7. By the same token, any other local or systemic conditions, such as sarcoidosis8 and lymphoma9, which would explain that situation, have just been discarded by means of pertaining propaedeutic. Nonetheless, during the diagnostic investigation process through an MRI, we noticed that a common point to them is the finding of liposubstitution of the parotid glands.
Therefore, this study aimed at informing about this pathology, which makes patients with this little-known pathology seek physicians.
METHODThis is a historical cross-sectional cohort study, carried out with the charts of 6 patients seen in the stomatology ward of our institution, between February of 2009 and January of 2012.
The inclusion criterion was patients who had clinical signs of volumetric increase of the parotid glands, without any local or systemic conditions that would justify them, after the pertaining diagnostic investigation, by means of an image exam, laboratorial and/or anatomic-pathological tests (Figure 1). In these cases, our investigation encompasses a complete blood count, antiSSB, anti-nucleus factor, rheumatoid factor, HIV, anti-HCV, Schirmer test, minor salivary gland biopsy, neck MRI, scintigraphy and, in selected cases: sialography.

Figure 1. Patient with bilateral parotid enlargement and liposubstitution seen upon MRI.
As for inclusion criterion, we defined the cases which were truly unilateral through the MRI.
Since it is a retrospective study based on information from patients' charts, without patient identification, there was no need for informed consent forms.
The project was approved by the Clinical Board and by the Ethics in Research Committee of the institution, under protocol # 49.444/12.
RESULTSWithin the time frame considered (February of 2009 through January of 2012), we admitted 483 new patients in our ward, of whom 64 (13.25%) had enlarged parotids as their main complaint, and six (1.24%) fit the inclusion criteria.
Upon MRI, the fat deposits on the parotids was seen by a T1 hypersignal; in fat suppression sequences, the suppressed sites are identified by hyposignal (T1 with contrast and T2)10 (Figures 2 and 3).

Figure 2. Axial section in T1 without contrast, showing hypersignal from the parotids.
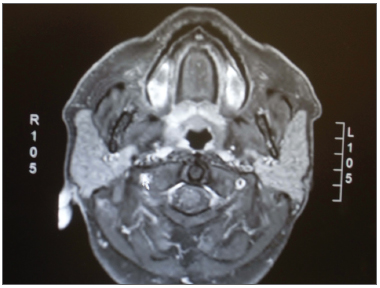
Figure 3. Axial section in T1 with contrast and fat suppression, showing hyposignal in the areas in which fat was suppressed.
The results obtained were plotted on the table below (Table 1).
The data collected point to three male patients and three females; therefore, there was no gender distinction. Age of onset varied between 33 and 68 years, with a mean age of 51 (± 12.06) years. The trait was recurrent in two patients (33.33%), being constant in the others. In all the patients, the parotid consistency was firm/fibroelastic, without irregularities or inflammatory signs, although mildly painful in one patient. We stress that xerostomy was complained by three patients (50%), confirmed upon clinical exam; notwithstanding, these patients were submitted to parotid gland scintigraphy, without any change in the tests. As far as habits are concerned, one patient (16.67%) reported being an ex-smoker and one patient (16.67%) reported mild alcohol consumption. In all the patients we found signs of liposubstitution of the parotid glands upon the MRI in both parotids, although in two cases they were unilateral.
We stress that the 64 cases of parotid enlargement in our ward had the following diagnosis: Sjögren's syndrome (15), repeating parotiditis of childhood (13), sialadenitis (7), infectious (7), tumoral (5), intraparotid cyst (4), HIV (2), lymphoma (2), alcoholic (1), sarcoidosis (1), liposubstitution (7). Of these four cases in which we found parotid liposubstitution, one case was taken off the study since the MRI showed unilateral changes.
DISCUSSIONParotid liposubstitution is a frequent radiologic finding; however, the literature does not have papers correlating idiopathic parotid bulging with its presence. It is known that this is a natural physiological process, like aging6 (we stress that the mean age of our sample was 51 years); however, subject to variations in accordance with the presence of subjacent clinical conditions1-5. In fact, the parotid liposubstitution with the Sjögren's syndrome is known, after having been demonstrated by Niemela et al.11, in a study involving 26 patients with the primary form of the disease, and changes (nodules or adipose degeneration in the parenchyma) were seen in 81% of the cases.
On the other hand, our series was made up of individuals without local or systemic diseases, exhaustively investigated, they presented parotid liposubstitution as a common denominator, which leads us to think that, in some cases, this is not a mere histological transformation as per expected with the gland aging, having a clinical and radiological manifestation of parotid enlargement. Parotid bulging was recurrent in two patients, which is not expected for a supposedly slow and gradual process. And finally, there are issues which still cannot be cleared up, especially since this is a theme with very little presence in the medical literature.
CONCLUSIONParotid liposubstitution, although a physiological process - expected with aging, may be associated with a bilateral enlargement of the glands in individuals who do not have systemic or local causes for such condition. However, some issues related to this association, remain open, and may be investigated in new studies.
REFERENCES1. Sheikh JS, Sharma M, Kunath A, Fritz DA, Glueck CJ, Hess EV. Reversible parotid enlargement and pseudo-Sjögren´s syndrome secondary to hypertriglyceridemia. J Rheumatol. 1996;23(7):1288-91.
2. Shiraishi H, Oiki H, Murata K. Fatty degeneration of the parotid gland after ovariectomy. Nihon Jibiinkoka Gakkai Kaiho. 2000;103(5):539-46.
3. Civibal C, Canpolat N, Yurt A, Kurugoglu S, Erdamar S, Bagci O, et al. A child with primary Sjögren syndrome and a review of the literature. Clin Pediatr (Phila). 2007;46(8):738-42.
4. Kabenge C, Ng S, Muyinda Z, Ameda F. Diagnostic ultrasound patterns of parotid glands in human immunodeficiency virus-positive patients in Mulago, Uganda. Dentomaxillofac Radiol. 2010;39(7):389-99.
5. Merlo C, Bohl L, Carda C, Gómez de Ferraris ME, Carranza M. Parotid sialosis: morphometrical analysis of the glandular parenchyme and stroma among diabetic and alcoholic patients. J Oral Pathol Med. 2010;39(1):10-5.
6. Kim SK. Changes in the secretory acinar cells of the rat parotid gland during aging. Anat Rec. 1984;209(3):345-54.
7. Vitali C, Bombardieri S, Jonsson R, Moutsopoulos HM, Alexander EL, Carsons SE, et al.; European Study Group on Classification Criteria for Sjögren´s Syndrome. Classification criteria for Sjögren's syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Ann Rheum Dis. 2002;61(6):554-8.
8. Sahu SK, Srivastava P, Kusum A, Kishore S, Sachan PK, Bahl DV. Parotid Sarcoidosis. Internet J Surg. 2007;9(1).
9. Dispenza F, Cicero G, Mortellaro G, Marchese D, Kulamarva G, Dispenza C. Primary Non-Hodgkins lymphoma of the parotid gland. Braz J Otorhinolaryngol. 2011;77(5):639-44.
10. Takagi Y, Sumi M, Sumi T, Ichikawa Y, Nakamura T. MR microscopy of the parotid glands in patients with Sjogren's syndrome: quantitative MR diagnostic criteria. AJNR Am J Neuroradiol. 2005;26(5):1207-14.
11. Niemelä RK, Takalo R, Pääkkö E, Suramo I, Päivänsalo M, Salo T, et al. Ultrasonography of salivary glands in primary Sjögren's syndrome. A comparison with magnetic resonance imaging and magnetic resonance sialography of parotid glands. Rheumatology (Oxford). 2004;43(7):875-9.
1. Otorhinolaryngologist (Fellow in Rhinology - Otorhinolaryngology Department - Santa Casa de São Paulo).
2. PhD in Otorhinolaryngology. Adjunct Professor and Director - Department of Otorhinolaryngology - Santa Casa de São Paulo. Otorhinolaryngology Department - Irmandade da Santa Casa de Misericórdia de São Paulo.
Send correspondence to:
Davi Sousa Garcia
Rua Dr. Cesário Motta Júnior, nº 112, Pavilhão Conde de Lara - 4º Andar. Vila Buarque
São Paulo - SP. Brazil. CEP: 01221-020
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on September 7, 2012.
Accepted on January 12, 2013. cod. 10442.


