INTRODUCTIONTinnitus is a symptom defined as an auditory perception in the absence of an external source of sound1,2. According to the World Health Organization (WHO), 278 million people have tinnitus - approximately 15% of the world population. This prevalence increases to 33% among individuals with more than 60 years of age2-4. In Brazil, it is estimated that we have 28 million individuals with tinnitus, making it a public health problem5.
Jastreboff3 and Sanchez et al.6 reported that 20% of the patients with tinnitus consider it a significant nuisance with a negative impact in their lives, which may cause depression and, in extreme cases, even suicide. Hallam et al.7> stress that the lack of habituation in some patients with tinnitus may be associated with personality traits or symptoms of depression.
The diagnosis of depression implies in a clear change in mood and depression symptoms. These alterations must last for at least two weeks and have a considerable impact on the work and family affairs of the individual8.
Depression may be associated with an increase in the difficulty to adapt to the compromises brought about by a chronic disease. There are indications that depression symptoms, as well as depression itself, are associated with such increase9,10. It is highly prevalent, with estimates that it affects 3% to 5% of the general population. In clinical settings, the incidence is even higher, since depression can be found in 5% to 10% of outpatients and in 9% to 16% of hospitalized patients11.
We know that depression is frequent in almost all chronic diseases, and when present, it leads to a worsening in quality of life, worse disease progression and worse compliance to treatment12.
Depression symptoms are: sadness, melancholy, frequent sobbing, apathy, a feeling of boredom, increased irritability, a feeling of hopelessness, lack of enthusiasm, insomnia or hypersomnia, loss or increase in appetite, libido reduction, anhedonia, ideas of death, pessimism, ideas of regret and guilt, suicidal acts or ideation, attention deficit, memory deficit, difficulty making decisions, a feeling of incapacity, slow thinking, psychomotor slowing down, negativism, ideas of ruination, hypochondriac delirium, auditory or visual delusions8.
The literature has studies concerning the presence of psychopathological factors associated with tinnitus. Tinnitus has been associated with numerous psychological problems, psychosomatic and psychiatric disorders, as well, especially, mood disorders. Depression symptoms are common in individuals with tinnitus, and may worsen their suffering. The mechanisms through which depression interacts with tinnitus are not thoroughly understood, but is a strong association with depression in patients with tinnitus13.
The nuisance associated with tinnitus is subjective and variable in relation to its intensity and frequency, and it might compromise the patient's life in a global way, causing personal, professional, social and family impairments.
The goal of this study is to establish the scientific evidence of the association between depression symptoms, depression and tinnitus.
METHODWe carried out a systematic review of the papers published on tinnitus and depression indexed in the following databases: PubMed, SciELO and LILACS.
Using the keywords taken from the Medical Subject Headings (MeSH), we setup the following advanced search strategy in PubMed: "Tinnitus"[Mesh] AND "Depressive Disorder"[Mesh] AND ("humans"[MeSH Terms] AND (English[lang] OR Spanish[lang] OR Portuguese[lang]) AND "adult"[MeSH Terms]).
In the LILACS and SciELO databases, we utilized the keywords indexed in the Health and Sciences Keywords and we setup the following strategy:
Tinnitus AND Depre$. We used the basic research form with the term
AND in order to select the words (
depression and tinnitus) and the trunking sign
$ in order to search for words with the same keyword root "depression".
The inclusion criteria were studied in patients older than 18 years, published in English, Portuguese or Spanish, associating tinnitus and depression. We took off letters to the editor and case studies.
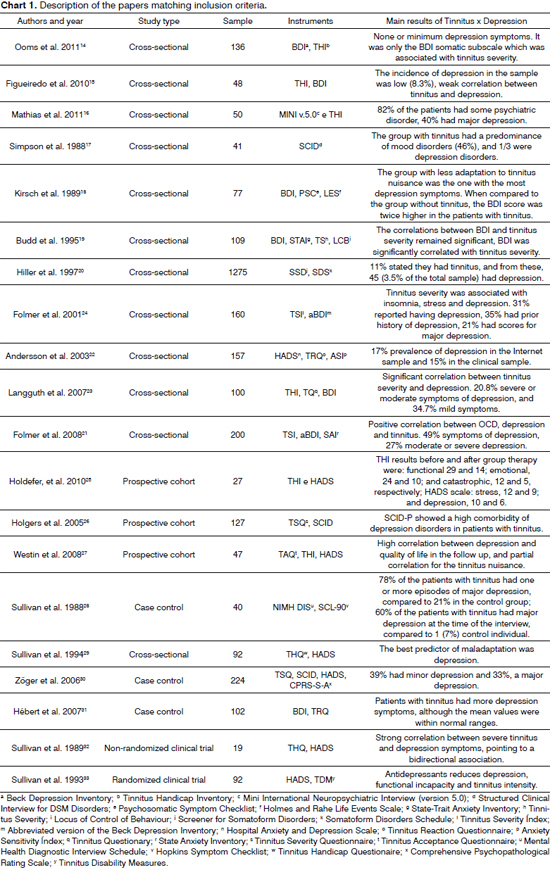
Data extraction from the selected papers was carried out by two reviewers, plotted according to the following information: authors, publishing year, sample size, study design, instruments utilized, main outcomes of the association between tinnitus and depression.
RESULTSOf the 64 studies found, 53 were found in PubMed, 11 in Lilacs and nine in SciELO; of the Lilacs/SciELO papers, nine were common to the two databases, and two were found in the Lilacs only, making up a total of 64 papers. The papers found are from the last 29 years (1982-2011).
Access to papers was possible thanks to the online distribution through the CAPES website, by the researchers going to the BIREME for access to the printed journals and by response to the authors' request by e-mail or regular mail.
Of the papers found, 2014-33 met the criterion to participate in the systematic review, and were included in the study; and 44 were taken off for being case reports, letters to the editor or for not correlating depression symptoms or depression with tinnitus.
Of the 20 studies matching the inclusion criteria, 12 were cross-sectional14-24,29, three were prospective and longitudinal25-27, three were case-controlled28,30,31 and two were clinical cases32,33.
A positive correlation between tinnitus and depression was found in 18 studies16-33, that is, these studies proved that depression is somehow associated, predisposing the patient to a maladaptation to tinnitus or as a consequence of the tinnitus severity. However, two studies14,15 did not find any significant association between depression and tinnitus, these two were cross-sectional studies.
The most used scale to detect depression was the BDI (eight studies)14,15,18,19,21,23,24,31 and the one most used to detect depression symptoms was the HADS (seven studies) 22,25,27,29,30,32,33, almost always associated with a severity scale of tinnitus symptoms, and the THI (five studies)14-16,23,27 the most used instrument. The samples varied much in size, from 27 to 1275 patients, with a mean value of 167.3 (Chart 1).
Two cross-sectional studies were unable to establish a significant correlation between depression and tinnitus14,15. In a study carried out by Figueiredo et al.15, the low incidence of depression (8.3%) in the study sample, showed a weak correlation between tinnitus and depression. One explanation could be the fact that the THI score was below the expected mean value and, in the literature, depression is associated to an increase in the nuisance, high THI scores. Ooms et al.14 found none or a minimum presence of depression symptoms. However, there was a significantly positive correlation (
p< 0.01) between the presence of somatic symptoms in the depression scale and the nuisance of tinnitus by the THI, capable of indicating an association of somatic symptoms and the severity of tinnitus.
Three prospective and longitudinal studies showed a high comorbidity of depression disorders in tinnitus patients25-27. Holdefer et al. showed that the severity of tinnitus can significantly predict depression in the follow-up25. In the study carried out by Holgers et al.26, there was a high prevalence of depression disorders in patients with severe tinnitus, and the study carried out by Westin et al. showed that the symptoms of depression, was the only measure with significant results in the follow-up27.
Three case-control studies28,30,31> also showed a positive correlation between depression and tinnitus. Hébert et al.31 compared the prevalence and severity of 27 physical symptoms in 51 patients with major depression and 51 paired controls, and found that 49% of the patients with depression also complained of tinnitus, compared to 11.8% of the controls. In the study carried out by Zöger et al.30, there was a correlation between tinnitus severity and depression, 39% of the patients had depression and 33% had major depression, and they concluded that depression is the most important factor associated to suffering in patients with tinnitus and was responsible for approximately 20% of the variance observed in the association. Sullivan et al.28 reported that patients with tinnitus had a significant prevalence of major depression during life (78%
vs. 21%) and significantly higher prevalence of depression at the time of the study (60%
vs. 7%) when compared to controls.
DISCUSSIONThe most relevant studies found were the two clinical trials. Sullivan et al.32 carried out a non-randomized, bind, placebo-washout clinical trial using nortryptiline, with 19 patients with severe tinnitus, diagnosed with major depression and concluded that treatment with antidepressants reduces tinnitus severity, alleviating its nuisance, since it reduced the intensity of depression symptoms. And Sullivan et al.33 did a randomized, double blind, placebo-controlled clinical trial using nortriptyline with 92 chronic tinnitus patients, 38 patients diagnosed with major depression and 54 patients had depression symptoms and tinnitus nuisance. They reported an improvement in depression symptoms and of the tinnitus nuisance; however, the patients considered the side effects of the medication as harmful to their quality of life. The authors suggest a strong correlation between severe tinnitus and depression symptoms a bidirectional association. Tinnitus can cause an increase in depression symptoms - which can cause a poor adaptation to tinnitus and, consequently, increase the tinnitus severity. They concluded that the treatment with antidepressants for patients with severe chronic tinnitus may be considered useful, but we still need clinical trials involving non-pharmacological treatments for depression, correlating with the quality of life of these patients.
There are at least three possibilities of associating depression and tinnitus: depression as one of the factors which worsens tinnitus18,19,22,28,31, tinnitus as a predisposing factor to depression14-17,20,24 and tinnitus installing as a comorbidity in patients with depression18,26-28,32; in such case, depression increase the intensity, the discomfort and the intolerance to tinnitus, increasing depression.
CONCLUSIONThere is a high prevalence of depression symptoms in patients with tinnitus. Studies suggest at least three possible associations between depression and tinnitus: depression as a factor affecting tinnitus, tinnitus as a factor which may predispose individuals to depression, and tinnitus as a comorbidity in patients with depression. However, the mechanisms of interaction between depression and tinnitus are not fully understood. Future studies are necessary to help unveil the cause-and-effect association between depression and tinnitus.
REFERENCES1. Almeida TAS, Samelli AG, Mecca FDN, Martino E de, Paulino AM. Sensação subjetiva do zumbido pré e pós-intervenção nutricional em alterações metabólicas. Pró-Fono. 2009;21(4):291-6.
2. Coelho CCB, Sanchez TG, Bento RF. Tinnitus characteristics of patients attended in a tinnitus clinic. Arq Int Otorrinolaringol. 2004;8(3):284-93.
3. Jastebroff PJ. Phantom auditory perception (tinnitus): mechanisms of generation and perception. Neurosci Res. 1990;8(4):221-54.
4. Pinto PC, Sanchez TG, Tomita S. The impact of gender, age and hearing loss on tinnitus severity. Braz J Otorhinolaryngol. 2010;76(1):18-24.
5. Sanchez TG, Knobel KA, Ferrari GMS, Batezati SC, Bento RF. Grupo de Apoio a Pessoas com Zumbido (GAPZ): metodologia, resultados e propostas futuras. Arq Int Otorrinolaringol. 2002;6(4):278-84.
6. Sanchez T, Zonato A, Bittar R, Bento R. Controvérsias sobre a fisiologia do zumbido. Arq Fund Otorrinolaringol. 1997;1(1):2-8.
7. Hallam RS, Jakes SC, Chambers C, Hinchcliff R. A comparison of different methods for assessing the 'intensity' of tinnitus. Acta Otolaryngol. 1985;99(5-6):501-8.
8. Belmaker RH, Agam G. Major depressive disorder. N Engl J Med. 2008;358(1):55-68.
9. Broadhead WE, Blazer DG, George LK, Tse CK. Depression, disability days, and days lost from work in a prospective epidemiologic survey. JAMA. 1990;264(19):2524-8.
10. Johnson J, Weissman MM, Klerman GL. Service utilization and social morbidity associated with depressive symptoms in the community. JAMA. 1992;18;267(11):1478-83.
11. Katon, WJ. Clinical and health Services relationships between major depression, depressive symptoms, and general medical illness. Biol Psychiatry. 2003;54(3):216-26.
12. Teng CT, Humes EC, Demetrio FN. Depressão e comorbidades clínicas. Rev Psiquiatr Clin. 2005;32(3):149-59.
13. Attias J, Shemesh Z, Bleich A, Solomon Z, Bar-Or G, Alster J, et al. Psychological profile of help-seeking and non-help-seeking tinnitus patients. Scand Audiol. 1995;24(1):13-8.
14. Ooms E, Meganck R, Vanheule S, Vinck B, Watelet JB, Dhooge I. Tinnitus severity and the relation to depressive symptoms: a critical study. Otolaryngol Head Neck Surg. 2011;145(2):276-81.
15. Figueiredo RR, Rates MA, Azevedo AA, Oliveira PM, Navarro PB. Correlation analysis of hearing thresholds, validated questionnaires and psychoacoustic measurements in tinnitus patients. Braz J Otorhinolaryngol. 2010;76(4):522-6.
16. Mathias KV, Mezzasalma MA, Nardi AE. Prevalência de transtorno de pânico em pacientes com zumbidos. Rev Psiquiatr Clín. 2011;38(4):139-42.
17. Simpson RB, Nedzelski JM, Barber HO, Thomas MR. Psychiatric diagnoses in patients with psychogenic dizziness or severe tinnitus. J Otolaryngol. 1988;17(6):325-30.
18. Kirsch CA, Blanchard EB, Parnes SM. Psychological characteristics of individuals high and low in their ability to cope with tinnitus. Psychosom Med. 1989;51(2):209-17.
19. Budd RJ, Pugh R. The relationship between locus of control, tinnitus severity, and emotional distress in a group of tinnitus sufferers. J Psychosom Res. 1995;39(8):1015-8.
20. Hiller W, Janca A, Burke KC. Association between tinnitus and somatoform disorders. J Psychosom Res. 1997;43(6):613-24.
21. Folmer RL, Griest SE, Martin WH. Obsessive-compulsiveness in a population of tinnitus patients. Int Tinnitus J. 2008;14(2):127-30.
22. Andersson G, Kaldo-Sandström V, Ström L, Strömgren T. Internet administration of the Hospital Anxiety and Depression Scale in a sample of tinnitus patients. J Psychosom Res. 2003;55(3):259-62.
23. Langguth B, Kleinjung T, Fischer B, Hajak G, Eichhammer P, Sand PG. Tinnitus severity, depression, and the big five personality traits. Prog Brain Res. 2007;166:221-5.
24. Folmer RL, Griest SE, Martin WH. Chronic tinnitus as phantom auditory pain. Otolaryngol Head Neck Surg. 2001;124(4):394-400.
25. Holdefer L, Oliveira CACP, Venosa AR. Group Therapy for Patients with Tinnitus at the University of Brasilia Medical School. Braz J Otorhinolaryngol. 2010;76(1):102-6.
26. Holgers KM, Zöger S, Svedlund K. Predictive factors for development of severe tinnitus suffering-further characterisation. Int J Audiol. 2005;44(10):584-92.
27. Westin V, Hayes SC, Andersson G. Is it the sound or your relationship to it? The role of acceptance in predicting tinnitus impact. Behav Res Ther. 2008;46(12):1259-65.
28. Sullivan MD, Katon W, Dobie R, Sakai C, Russo J, Harrop-Griffiths J. Disabling tinnitus. Association with affective disorder. Gen Hosp Psychiatry. 1988;10(4):285-91.
29. Sullivan M, Katon W, Russo J, Dobie R, Sakai C. Coping and marital support as correlates of tinnitus disability. Gen Hosp Psychiatry. 1994;16(4):259-66.
30. Zöger S, Svedlund J, Holgers KM. Relationship between tinnitus severity and psychiatric disorders. Psychosomatics. 2006;47(4):282-8.
31. Hébert S, Carrier J. Sleep complaints in elderly tinnitus patients: a controlled study. Ear Hear. 2007;28(5):649-55.
32. Sullivan MD, Dobie RA, Sakai CS, Katon WJ. Treatment of depressed tinnitus patients with nortriptyline. Ann Otol Rhinol Laryngol. 1989;98(11):867-72.
33. Sullivan M, Katon W, Russo J, Dobie R, Sakai C. A randomized trial of nortriptyline for severe chronic tinnitus. Effects on depression, disability, and tinnitus symptoms. Arch Intern Med. 1993;153(19):2251-9.
1. MSc; PhD student. Psychologist - Medical School of the Federal University of São Paulo -UNIFESP-EPM.
2. PhD. Post-Doctoral program. DDS - UNIFESP-EPM.
3. PhD. Associate Professor of Psychiatry - UNIFESP-EPM.
4. Post-Doctoral Degree - Adjunct Professor of Otorhinolaryngology - UNIFESP-EPM.
Department of Otorhinolaryngology and Head and Neck Surgery, Federal University of São Paulo - UNIFESP-EPM.
Send correspondence to:
Luciana Geocze
Rua dos Otonis, nº 700, 1º andar. Vila Clementino
São Paulo - SP. Brazil. CEP: 04025-002
Tel: (11)5575-2552.
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on August 10, 2012.
Accepted on October 25, 2012. cod. 10003.


