INTRODUCTIONNeurofibromatosis type 2 (NF2) is a dominant autosomal disease which affects 1:40,000 individuals1,2. In these cases there is a two allele mutation on the chromosome 22 long arm tumor suppressor gene1,2. The patients usually develop multiple schwannomas along the spine and in the skull. Bilateral vestibular schwannoma happens in 90% of those with the gene1. These patients will invariably develop progressive sensorineural hearing loss, characterized by poor sound discrimination. Tinnitus and unbalance may also happen1.
The auditory rehabilitation of patients who evolved to a severe-profound hearing loss, until very recently was restricted to them learning lip reading. In 1979, House and Hitselberger started to change this story when they performed the first single channel auditory brainstem implant (ABI) in a NF2 deaf patient3. The implant electrode bundle has improved with the years, going from 8 to 21 electrodes4. This technological progress has benefited over 700 patients implanted with the ABI, with variable auditory responses1,2,4-8.
During the 90's, the cochlear implant (CI) also became available for the rehabilitation of deaf patients with NF2 submitted to tumor resection with cochlear nerve preservation9-15.
The auditory rehabilitation of NF2 patients may be carried out in two different ways (CI or ABI). We will, hereby, report on the auditory results from four patients with NF2 submitted to brainstem or cochlear auditory implant surgery in our clinic, and review the literature on this topic.
METHODWe prospectively assessed four NF2 patients submitted to vestibular schwannoma exeresis surgery during February of 2006 and March of 2009. The ipsilateral brainstem implant (ABI) or the cochlear implant (IC) was carried out in the same procedure, depending on cochlear nerve preservation.
Clinical and radiological data were collected before surgery, stressing auditory performance, auditory deprivation time and tumor size.
Three patients were implanted through the translabyrinthine approach with the Nucleus 24
® ABI (Cochlear Corporation) after tumor removal. In order to assess the lateral wall of the IV ventricle (Luschka's foramen). As anatomical landmarks, we used the following: the IX cranial nerve, the acoustic-facial trunk, the cerebellar flocculus and the choroid plexus. During the surgeries, the VII, IX, X and XI ipsilateral cranial nerves were continuously monitored (NIM Response-2; Medtronic Xomed).
Brainstem electrically evoked auditory potentials (electrical ABR) were used to check for proper positioning of the electrode bundle, by means of the Biologic Navigator Pro (Bio-logic Systems Corp.
®) device, coupled to the implant stimulation interface through a sync cable.
In one patient, the cochlear nerve anatomical preservation was possible during tumor exeresis through the retrolabyrinthine approach. The promontory electrical stimulation test during surgery showed a present response, although with poor morphology and dubious reproducibility. We decided to use the Nucleus Freedom Contour Advanced
® (Cochlear Corporation) simultaneous cochlear implant through the round window. In such case, intraoperative neural telemetry showed no response in the five electrodes tested. The electrode bundle positioning was checked after surgery through Stenvers and transorbital view x-rays.
Checking electrode impedances, both in ABI as well as in CI showed inadequate values.
ABI activation was done approximately 1 month after the surgery, with the patient awake in an ICU unit with cardiorespiratory monitoring. The electrodes were sequentially activated with a monopolar current, with a gradual increase for recording a comfortable auditory sensation and side effects. The speech coding strategy used in the three patients was the Spectral peak (Speak). CI activation was carried out after surgery and the speech coding strategy was the advanced combination encoders (ACE).
The auditory results after 48 months using the ABI and 12 months using the CI were expressed in: tonal thresholds in a sound field, four-choice test, vowel and phrases recognition index presented in a closed and open format, telephone use.
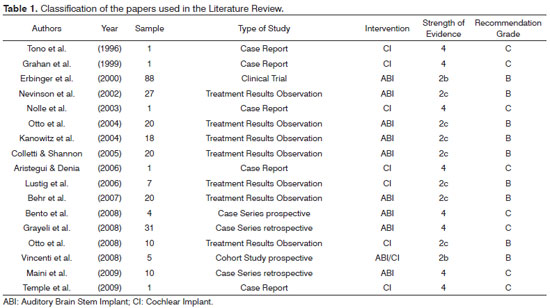
For the literature review, we used the following keywords: (cochlea or cochlear or auditory or ear) and (brain implant or brain implants), in the Medline, Lilacs and Scielo databases, with the limit of publication period up to March of 2010. We found 1118 publications. Of these, there were 17 clinical trials with NF2 patients submitted to cochlear or brainstem auditory implant, in English or Portuguese. Each study was classified according to its strength of evidence, according to the classification from the Oxford Centre for Evidence-based Medicine for studies on treatment (Table 1). Later on, these studies were also classified according to the degree of recommendation, nine publications with recommendation grade B and eight with recommendation grade C (Table 1).
This study was approved by the Ethics Committee for Research Project Analysis of our institution, under protocol number 1135/07. Extensive explanation on the risks and benefits of brainstem auditory implant surgery and the option to continue only with the lip reading training therapy were given to the patients. Signing the Informed Consent Form meant agreeing to participate in the study.
RESULTSThe three patients implanted with an ABI were males, with a mean age of 26.3 ± 1.5 years, mean deafness duration of 6.0 ± 4.0 years and mean tumor size of 3.2 ± 1.4 cm (Table 2). They all regularly used their devices for more than eight hours a day. None of them used a personal sound amplification device (PSAD) in the contralateral ear.
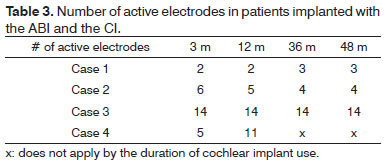
No additional postoperative complication was observed on these patients by placing the ABI. Two patients had post-operative facial paralysis, keeping a House-Brackmann score of VI. One developed a CSF fistula, treated by an external lumbar shunt and compressive brain dressing. The adverse effects seen during the ABI activation were: throat stimulation (1), torso (2), upper (2) and lower limbs (1), nausea (1) and nystagmus (1). The number of electrodes which generate hearing sensation without side effects varied between 2 and 14 (Table 3).
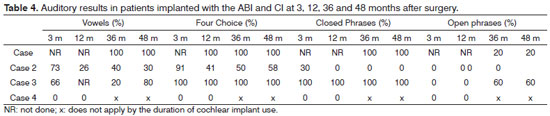
The mean value of the audiometric threshold in the free field using the device with ABI patients in the frequencies of 500; 1,000; 2,000 and 4,000 Hz was 36.7 ± 5.7 decibels (Graph 1). The tonal thresholds reached were similar among the patients and were maintained stable throughout the years. Auditory performance varied, one patient does not recognize open sentences and only 20% closed ones. The other two recognize 100% of the phrases and 10% and 20% open (Table 4). Only one of them was capable of communicating on the phone.
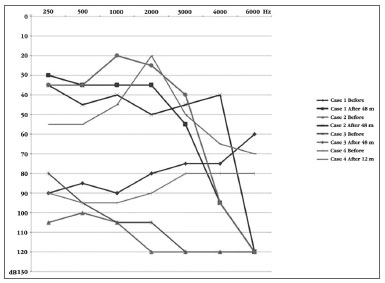
Graph 1. Free field audiometric thresholds before and after the implant.
The patient implanted with CI was 36 years old, with a 10-year history of progressive hearing loss, evolving towards a severe hearing loss for 1 year (Table 2). The tumor on the implanted side measured 1.5 cm (Table 2). She also used her implant regularly for more than 8 hours a day and used a contralateral PSAD for 7 months, with low sounds perception.
Upon activation, there were five electrodes with auditory sensation and without side effects. After 12 months of stimulation, 11 electrodes could be activated without side effects. The audiometric threshold in a free field improved after the CI, the mean values for the following frequencies: 500; 1,000; 2,000 and 4,000 Hz was 46.2 decibels (Graph 1). Despite the improvement in tonal thresholds, the patient managed to detect only the presence of sound, not discriminating phrases, words, vowels, and rhythm (Table 4).
SYSTEMATIC REVIEW OF THE LITERATURE AND DISCUSSIONThe auditory rehabilitation of NF2 patients, who develop deafness, may be carried out in two ways: auditory cochlear or brainstem implants2,3. The choice of implant type to the utilized will depend on the anatomical and functional preservation of the cochlear nerve during the tumor resection surgery2,3. In these regards, electrophysiological tests have a crucial role in the identification of cochlear nerve responses.
This can be done during the procedure, studying the cochlear nerve action potential2. If this potential is present, the cochlear implant can be placed simultaneously with the tumor resection. Should this potential be absent or not reproducible, one should perform the promontory electrical stimulation test 6 to 8 weeks after the procedure2. In the immediate post-op, the electrical stimulation test on the promontory may be negative because of cochlear nerve neuropraxia, caused by surgical manipulation2. Such test is based on the introduction of a transtympanic needle, under local anesthesia, which will contact the promontory. The electrical stimulus is provided to the promontory in five different frequencies (50, 100, 200, 400 and 800 Hz) and the current level, initially of 0 µAmps, is progressively increased until the patient hears of perceives the stimulus2. The test is deemed positive when there is mild perception of a tone and differentiation between the different pitches. The test is deemed negative when the patient feels only a discomfort caused by the electrical stimulus2.
The literature has data on eight patients with anatomical preservation of the cochlear nerve, submitted to CI surgery, but without functional proof by an electrophysiological test, with results which were lower than those from a group of patients with cochlear nerve functional confirmation15,16 (Table 5). Only three of the eight cases had phrases discrimination15,16 (Table 5). The data from the other group with six patients with anatomical and functional preservation of the cochlear nerve, proven by electrophysiological tests, showed phrase discrimination in all the cases, with a mean value of 74.5 ± 18.8% (50-100)2,16,17 (Table 5).
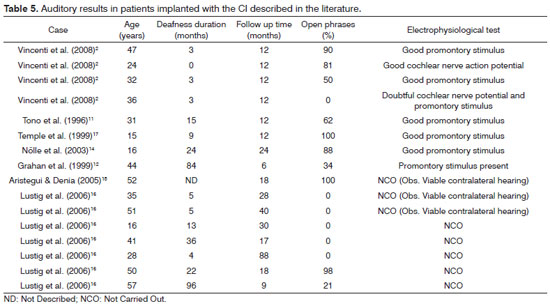
However, in one case of promontory stimulation, with a long time between the tumor resection surgery and the cochlear implant, the discrimination of open phrases was worse12 (Table 5). In this case, the cochlear basal turn was found to be ossified during surgery, suggesting that the insertion of the electrode bundle in the cochlea, when not together with the tumor removal, must be carried out in the shortest possible time in order to avoid cochlear ossification consequent to surgical manipulation12. In one case with cochlear nerve anatomical preservation, but with questionable response upon the promontory electrical stimulation test as to the nerve's action potential, speech discrimination was not achieved2 (Table 5). We found the same thing in our CI patient; despite cochlear nerve anatomical preservation, the promontory electrical stimulation test yielded poor responses and the patient did not discriminate the sounds; thus, the importance of functional proof of the nerve in order to obtain a good audiological result.
When it was not possible to spare the cochlear nerve during the vestibular schwannoma resection surgery or when its anatomical sparing did not generate electrophysiological responses, the only feasible option for the auditory rehabilitation is the brainstem auditory implant1,2,4-6,16,18-21.
Studies have shown that the ABI (Auditory Brainstem Implant) has variable audiological responses. Nonetheless, it is a consensus that the ABI enables the perception of alert environmental sounds between 85% 7 to 96.2%5 of the patients after one year of surgery, besides enhancing lip reading5,18,20.
Patients with auditory perception recognize the difference between the human speech sound and environmental sound and 64% recognize the difference between the voices from female/male and adult/children5. The mean open phrase recognition after one year using the ABI varies among the studies from 5% to 48%, together with lip reading, the values vary between 25 and 79% 20. In general, the ABI provides an additional gain between 30% and 40% compared to lip reading only1,2,5,18-20. Using a telephone is not an expected result, being the exception to the rule2,5.
The benefit provided by the ABI does not discard training in lip reading and multidisciplinary rehabilitation is very important for patient improvement1. Even after one year using the ABI, improvements continue to be seen4. In our series, one of the patients had a worsening in his auditory perception along the years, despite the fact that his tonal thresholds had improved. Of the six working electrodes he had, only four remained. We do not know, for sure how to explain such worsening, but since this is the patient with the largest tumor, we speculate that there could have been a progressive damage to the cochlear core, corroborated by the progressive electrode deactivation time. The electrodes are deactivated when the stimuli do not generate significant auditory input or causes extra-auditory inputs (side effects by stimulation from adjacent cores). In this patient, as time passed, it was necessary to increase the electrical charge in order to generate an auditory input, which caused greater stimulation scatter and more pronounced side effects.
Comparing the literature results obtained from NF2 patients with cochlear nerve function and anatomical preservation, submitted to CI with those submitted to ABI, there were no great differences in relation to the recognition of vowels and consonants2. The recognition of dissyllable words and phrases was higher with the cochlear implant2. Moreover, most of the patients implanted with a CI are able to use the telephone.
CONCLUSIONPatients with neurofibromatosis type 2 have now the technological resources which help in the auditory rehabilitation, providing an additional gain upon lip reading training. Although our experience has shown the opposite, literature shows that when possible to anatomically and functionally spare the cochlear nerve, the cochlear implant yields better auditory and language results. When cochlear nerve sparing is not possible, the brainstem auditory implant may be used for the same end.
REFERENCES1. Kanowitz SJ, Shapiro WH, Golfinos JG, Cohen NL, Roland JT Jr. Auditory brainstem implantation in patients with neurofibromatosis type 2. Laryngoscope. 2004;114(12):2135-46.
2. Vincenti V, Pasanisi E, Guida M, Di Trapani G, Sanna M. Hearing rehabilitation in neurofibromatosis type 2 patients: cochlear versus auditory brainstem implantation. Audiol Neurootol. 2008;13(4):273-80.
3. Hitselberger WE, House WF, Edgerton BJ, Whitaker S. Cochlear nucleus implants. Otolaryngol Head Neck Surg. 1984;92(1):52-4.
4. Maini S, Cohen MA, Hollow R, Briggs R. Update on long-term results with auditory brainstem implants in NF2 patients. Cochlear Implants Int. 2009;10 Suppl 1:33-7.
5. Nevison B, Laszig R, Sollmann WP, Lenarz T, Sterkers O, Ramsden R, et al. Results from a European clinical investigation of the Nucleus multichannel auditory brainstem implant. Ear Hear. 2002;23(3):170-83.
6. Colletti V, Shannon RV. Open set speech perception with auditory brainstem implant? Laryngoscope. 2005;115(11):1974-8.
7. Ebinger K, Otto S, Arcaroli J, Staller S, Arndt P. Multichannel auditory brainstem implant: US clinical trial results. J. Laryngol Otol Suppl. 2000;(27):50-3.
8. Bento RF, Brito Neto RV, Tsuji RK, Gomes MQ, Goffi-Gomez MV. Auditory Brainstem Implant: surgical technique and early audiological results in patients with neurofibromatosis type 2. Braz. J Otorhinolaryngol. 2008;74(5):647-51.
9. Cueva RA, Thedinger BA, Harris JP, Glasscock ME 3rd. Electrical promontory stimulation in patients with intact cochlear nerve and anacusis following acoustic neuroma surgery. Laryngoscope. 1992;102(11):1220-4.
10. Hulka GF, Bernard EJ, Pillsbury HC. Cochlear implantation in a patient after removal of an acoustic neuroma: the implications of magnetic resonance imaging with gadolinium on patient management. Arch Otolaryngol Head Neck Surg. 1995;121(4):465-8.
11. Tono T, Ushisako Y, Morimitsu T. Cochlear implantation in an intralabyrinthine acoustic neuroma patient after resection of an intracanalicular tumour. J Laryngol Otol. 1996;110(6):570-3.
12. Graham J, Lynch C, Weber B, Stollwerck L, Wei J, Brookes G. The magnetless Clarion cochlear implant in a patient with neurofibromatosis 2. J Laryngol Otol. 1999;113(5):458-63.
13. Ahsan S, Telischi F, Hodges A, Balkany T. Cochlear implantation concurrent with translabyrinthine acoustic neuroma resection. Laryngoscope. 2003;113(3):472-4.
14. Nölle C, Todt I, Basta D, Unterberg A, Mautner VF, Ernst A. Cochlear implantation after tumour resection in neurofibromatosis type 2: impact of infra- and postoperative neural response telemetry monitoring. ORL J Otorhinolaryngol Relat Spec. 2003;65(4):230-4.
15. Aristegui M, Denia A. Simultaneous cochlear implantation and translabyrinthine removal of vestibular schwannoma in an only hearing ear: report of two cases (neurofibromatosis type 2 and unilateral vestibular schwannoma). Otol Neurotol. 2005;26(2):205-10.
16. Lustig LR, Yeagle J, Driscoll CL, Blevins N, Francis H, Niparko JK. Cochlear implantation in patients with neurofibromatosis type 2 and bilateral vestibular schwannoma. Otol Neurotol. 2006;27(4):512-8.
17. Temple RH, Axon PR, Ramsden RT, Keles N, Deger K, Yücel E. Auditory rehabilitation in neurofibromatosis type 2: a case for cochlear implantation. J Laryngol Otol. 1999;113(2):161-3.
18. Otto SR, Shannon RV, Wilkinson EP, Hitselberger WE, McCreery DB, Moore JK, et al. Audiologic outcomes with the penetrating electrode auditory brainstem implant. Otol Neurotol. 2008;29(8):1147-54.
19. Behr R, Müller J, Shehata-Dieler W, Schlake HP, Helms J, Roosen K, et al. The High Rate CIS Auditory Brainstem Implant for Restoration of Hearing in NF-2 Patients. Skull Base. 2007;17(2):91-107.
20. Otto SR, Brackmann DE, Hitselberger W. Auditory brainstem implantation in 12- to 18-year-olds. Arch Otolaryngol Head Neck Surg. 2004;130(5):656-9.
21. Grayeli AB, Kalamarides M, Bouccara D, Ambert-Dahan E, Sterkers O. Auditory brainstem implant in neurofibromatosis type 2 and non-neurofibromatosis type 2 patients. Otol Neurotol. 2008;29(8):1140-6.
1. ENT Physician; Ear Surgery and Lateral Skull Base Surgery Fellow - Department of Otorhinolaryngology - Medical School of the University of São Paulo - HCFMUSP.
2. PhD; Speech and Hearing Therapist - Department of Otorhinolaryngology - HCFMUSP.
3. PhD. Assistant Physician - Department of Otorhinolaryngology - Medical School of the University of São Paulo - HCFMUSP.
4. Neurosurgeon; Assistant Physician - Department of Neurosurgery - HCFMUSP.
5. Senior Associate Professor - Department of Otorhinolaryngology - Medical School of the University of São Paulo - HCFMUSP.
6. Full Professor - Department of Otorhinolaryngology - Medical School of the University of São Paulo - HCFMUSP.
Departamento de Otorrinolaringologia e Neurocirurgia do Hospital das Clinicas da Faculdade de Medicina da Universidade de São Paulo.
Send correspondence to:
Tatiana Alves Monteiro
Faculdade de Medicina da Universidade de São Paulo
Av. Doutor Eneas de Carvalho Aguiar nº 155, 6º andar, sala 6167
São Paulo - SP. Brazil
Tel: (11) 81537487. Fax: (11) 30697833
E-mail: vitatimonteiro@ig.com.br
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on June 27, 2011.
Accepted on April 13, 2012. cod.8656.


