INTRODUCTIONHypocalcemia is the most frequent complication in total thyroidectomy and affects 1.7% to 68% of the patients submitted to this procedure. The drop in calcium serum levels is usually transient and often asymptomatic, and correlates with permanent hypoparathyroidism in only 0% to 9% of the cases. However, the presence of symptomatic hypocalcemia may evolve to tetany, seizures, and even death unless it is diagnosed early on and treatment is offered to the patients1-9. Some authors believe the better way to prevent the risk of hypocalcemia is offering calcium oral supplementation accompanied or not by vitamin D to all patients submitted to total thyroidectomy. However, this approach could mean that 64% to 87% of the patients would be given unnecessary supplementation as they do not develop symptoms and their parathyroid hormone (PTH) levels return to normal within the week after surgery in 70% to 94% of the cases10,11. Additionally, hypercalcemia occurred in 4% of the patients given calcium supplementation and vitamin D after total thyroidectomy12-14.
Considering the drawbacks of compulsory supplementation, most services resort to clinical monitoring and serial serum calcium level testing to detect the patients with low calcium levels and symptomatic hypocalcemia who could benefit from calcium and vitamin D supplementation. Once most patients present symptoms of hypocalcemia and/or significant drops in serum calcium starting at 48 hours after surgery, with symptoms peaking in as many as four days15, they would have to be kept in the hospital for observation. Thus, patients with low risk of hypocalcemia would be prevented from leaving the hospital after the procedure and hospitalization costs would increase. Intact parathyroid hormone (i-PTH) testing done between one and 24 hours after thyroidectomy was recently found to be an effective method in the early detection of patients with symptomatic hypocalcemia requiring supplementation, thus allowing the subjects with low risk of developing this complication to be discharged earlier16,17. Despite the proven efficacy of i-PTH testing in managing total thyroidectomy patients, there is still no consensus as to the when in postoperative care i-PTH testing should be done and whether serial tests or tests associated with serum calcium levels ought to be done.
This study looked into the correlations between i-PTH serum levels measured at different times in post-thyroidectomy care and the occurrence of symptomatic hypocalcemia. The findings of this study and other publications in the literature were used to design an algorithm on the use of i-PTH tests in the clinical setting.
METHODThis longitudinal cohort study enrolled 113 consecutive patients submitted to total thyroidectomy and partial to total thyroidectomy conversion procedures in a tertiary care teaching hospital between June of 2006 and December of 2010. The study was registered at CONEP (373972) and approved by the Research Ethics Committee of the institution (CEP 10048).
All patients were tested for i-PTH under anesthetic induction four and 12 hours after surgery with immunometric assay Immulite 2000
® (normal threshold between 11 and 67 pg/mL). They were observed clinically for symptom onset (lip and finger extremity paresthesia) and signs of hypocalcemia (Chvostek and Trousseau). Only the subjects with symptomatic hypocalcemia or confirmed low calcium levels (ionic calcium under 1 mmol/L) were given oral calcium and vitamin D supplementation. The patients were informed of the risk of developing hypocalcemia symptoms after discharge and advised to seek medical help before taking the oral supplementation if the symptoms manifested.
Absolute i-PTH values are dichotomic (normal
versus below normal), and thus the probability of developing hypocalcemia was estimated based on serial testing and tests done four and 12 hours after surgery. In serial testing the lower value obtained between the two tests was considered for risk analysis. The performance of the different PTH testing times as early predictors for hypocalcemia was rated based on their sensitivity, specificity, positive predictive values, and negative predictive values using McNemar's test. Statistical data analysis was performed on software package SAS release 9.2 (SAS Institute, Inc., Cary, N.C, USA).
RESULTSThree patients were excluded from the study as they had been taking alendronate and calcium supplements before surgery. Sixteen (14.54%) of the 110 patients included in the study were males and 94 (85.46%) were females; their mean age was 48.25 years. Ninety-six patients (87.2%) underwent total thyroidectomy in one stage, while nine (8.2%) were converted from partial to total thyroidectomy and another five (4.6%) were submitted to neck dissection of the central compartment combined with total thyroidectomy. Pathology testing confirmed the presence of malignant tumors in 55 (50%) patients and benign disease in the remaining subjects. The thirty-one (28.18%) patients with symptomatic hypocalcemia were grouped together and compared to the other 79 (71.82%) patients with normal blood calcium levels. The levels of i-PTH at different points in care were highly sensitive (90.3% to 96.8%) for symptomatic hypocalcemia, while specificity ranged between 77.2% and 87.3%. No significant differences were found in the sensitivity level of the tests done four or twelve hours after surgery and in serial testing, but the specificity and positive to negative predictive value ratio of i-PTH levels measured twelve hours after surgery were significantly higher than on serial tests (
p < 0.007). Statistics are summed up in Tables 1 and 2.
DISCUSSIONParathyroid function may be compromised after thyroidectomy, whether by direct trauma or gland vascular impairment, leading to reduced levels of circulating PTH and consequent drops in blood calcium18. Until recently, the detection of patients at high risk for severe hypocalcemia relied on the clinical observation of the signs and symptoms connected to the complication or on drops in blood calcium, usually seen 24-48 hours after surgery19,20. The development of specific immunometric assays to verify the level of i-PTH21,22 aided significantly to the use of parathyroid hormone as an early predictor for hypocalcemia in patients submitted to total thyroidectomy. Due to their short half-life - 3 to 5 minutes - drops in i-PTH can be observed immediately after surgery23,24. Although many studies have looked into the correlations between postoperative i-PTH levels and risk of hypocalcemia, very few tried to establish the obvious resulting clinical applications, once test results and conclusions in these studies vary significantly. Immediate i-PTH levels are generally regarded as the test results from blood collected up to six hours after surgery; late i-PTH is obtained 12 hours after surgery. This study analyzed the differences between immediate, late, and serial i-PTH testing in determining the risk of hypocalcemia. Sensitivity levels were 93.5%, 90.3% and 96.8% in 4-hour, 12-hour, and serial tests respectively.
These findings were consistent with the studies by Soon et al.25 (92.3%), Sywak et al.26 (90%), and Toniato et al.27 (95.85%); these authors found that drops in i-PTH to levels under normal in the assay were well correlated with occurrence of hypocalcemia. These levels of sensitivity are higher than those reported by Scurry et al.28 (80%), Di Fabio et al.29 (76.2%), and Khafif et al.30 (23%); these authors, by their turn, correlated drops in i-PTH greater than 75%-80% from the baseline preoperative values as a risk factor for hypocalcemia.
These findings indicate that using the lower threshold for normal i-PTH levels as a reference to determine the risk of hypocalcemia is more sensitive than calculating percentage drops as proposed by some authors, once the prevalence of severe symptomatic hypocalcemia is higher in patients with subnormal i-PTH levels31,32. No statistically significant differences were found when the sensitivity levels of 4-hour, 12-hour, and serial tests were compared, thus suggesting a strong correlation between the findings obtained from tests done at different times after surgery as shown by Vescan et al.33 and Grodski & Serpell24.
Observed specificity levels were 78.5% (4-hour PTH), 87.3% (12-hour PTH), and 77.2% (sPTH), showing that tests can be used safely to determine which patients are at a low risk of developing symptomatic hypocalcemia when their postoperative i-PTH levels are normal. The same was seen by Lam & Kerr34 in a study enrolling 40 patients, in which no cases of hypocalcemia were observed in subjects with normal postoperative i-PTH levels. The chance of finding subnormal i-PTH levels in patients with hypocalcemia was 4.2 to 7 times greater than the chance of observing altered test results in individuals with normal calcium levels.
This allows patients at a low risk for hypocalcemia to be discharged within 24 hours of surgery, resulting in significant reductions in hospitalization costs as shown by Payne et al.35, in a study that revealed a cost reduction of approximately USD 726 per total thyroidectomy patient discharged earlier based on postoperative i-PTH and calcium levels.
Specificity was greater in the i-PTH tests done 12 hours after surgery (
p = 0.007). Therefore, we would like to recommend a protocol now in use at our institution, in which one i-PTH test is done to screen patients at a low risk of developing severe symptomatic hypocalcemia after total thyroidectomy as shown in Figure 1.
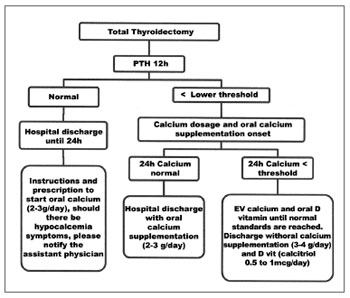
Figure 1. Single test algorithm for 12-hour i-PTH as a predictor for hypocalcemia - PTH - intact parathyroid hormone.
Intact parathyroid hormone levels are highly sensitive and specific for risk of hypocalcemia. One single test 12 hours after surgery can be used to select patients at a low risk for hypocalcemia and start early treatment for high risk patients.
REFERENCES1. Al-Suliman NN, Ryttov NF, Qvist N, Blichert-Toft M, Graversen HP. Experience in a specialist thyroid surgery unit: a demographic study, surgical complications, and outcome. Eur J Surg. 1997;163(1):13-20.
2. Wilson RB, Erskine C, Crowe PJ. Hypomagnesemia and hypocalcemia after thyroidectomy: prospective study. World J Surg. 2000;24(6):722-6.
3. Bergenfelz A, Jansson S, Kristoffersson A, Martensson H, Reihnér E, Wallin G, et al. Complications to thyroid surgery: results as reported in a database from a multicenter audit comprising 3,660 patients. Langenbecks Arch Surg. 2008;393(5):667-73.
4. Glinoer D, Andry G, Chantrain G, Samil N. Clinical aspects of early and late hypocalcaemia after thyroid surgery. Eur J Surg Oncol. 2000;26(6):571-7.
5. Tovi F, Noyek AM, Chapnik JS, Freeman JL. Safety of total thyroidectomy: review of 100 consecutive cases. Laryngoscope. 1989;99(12):1233-7.
6. Jafari M, Pattou F, Soudan B, Devos M, Truant S, Mohiedine T, et al. Étude prospective des facteur prédictifs precoces de la survenue d'hipocalcémie définitive aprés thyroidectomie bilatérale. Ann Chir. 2002;127(8):612-8.
7. Proye C, Carnaille B, Maynou C, Bizard JP, Gilliot P, Lariviere J, et al. Le risque parathyroïdien en chirurgie thyroïdienne. Chirurgie. 1990;116(6-7):493-500.
8. Megherbi MT, Graba A, Abid L, Oulmane D, Saidani M, Benabadji R. Complications et séquelles de la chirurgie thyroïdienne bénigne. J Chir. 1992;129(1):41-6.
9. Khairy GA, Al-Saif A. Incidental parathyroidectomy during thyroid resection: incidence, risk factors, and outcome. Ann Saudi Med. 2011;31(3):274-8.
10. Pattou F, Combemale F, Fabre S, Carnaille B, Decoulx M, Wemeau JL, et al. Hypocalcemia following thyroid surgery: incidence and prediction of outcome. World J Surg. 1998;22(7):718-24.
11. Del Rio P, Arcuri MF, Ferreri G, Sommaruga L, Sianesi M. The utility of serum PTH assessment 24 hours after total thyroidectomy. Otolaryngol Head Neck Surg. 2005;132(4):584-6.
12. Youngwirth L, Benavidez J, Sippel R, Chen H. Parathyroid hormone deficiency after total thyroidectomy: incidence and time. J Surg Res. 2010;163(1):69-71.
13. Roh JL, Park CI. Routine oral calcium and vitamin D supplements for prevention of hypocalcemia after total thyroidectomy. Am J Surg. 2006;192(5):675-8.
14. Sabour S, Manders E, Steward DL. The role of rapid PACU parathyroid hormone in reducing post-thyroidectomy hypocalcemia. Otolaryngol Head Neck Surg. 2009;141(6):727-9.
15. Aluffi P, Aina E, Bagnati T, Toso A, Pia F. Prognostic factors for definitive hypoparathyroidism following total thyroidectomy. Acta Otorrinolaringol Esp. 2008;59(7):321-4.
16. Lindblom P, Westerdahl J, Bergenfelz A. Low parathyroid hormone levels after thyroid surgery: a feasible predictor of hypocalcemia. Surgery. 2002;131(5):515-20.
17. AES Guidelines 06/01 Group. Australian Endocrine Surgeons Guidelines AES/06/01. Postoperative parathyroid hormone measurement and early discharge after total thyroidectomy: analysis of Australian data and management recommendations. ANZ J Surg. 2007;77(4):199-202.
18. Hermann M, Ott J, Promberger R, Kober F, Karik M, Freissmuth M. Kinetics of serum parathyroid hormone during and after thyroid surgery. Br J Surg. 2008;95(12):1480-7.
19. Husein M, Hier MP, Al-Abdulhadi K, Black M. Predicting calcium status post thyroidectomy with early calcium levels. Otolaryngol Head Neck Surg. 2002;127(4):289-93.
20. Adams J, Andersen P, Everts E, Cohen J. Early postoperative calcium levels as predictors of hypocalcemia. Laryngoscope. 1998;108(12):1829-31.
21. Gao P, Scheibel S, D'Amour P, John MR, Rao SD, Schmidt-Gayk H, et al. Development of a novel immunoradiometric assay exclusively for biologically active whole parathyroid hormone 1-84: implications for improvement of accurate assessment of parathyroid function. J Bone Miner Res. 2001;16(4):605-14.
22. Goodman WG. The evolution of assays for parathyroid hormone. Semin Dial. 2005;18(4):296-301.
23. Noordzij JP, Lee SL, Bernet VJ, Payne RJ, Cohen SM, McLeod IK, et al. Early prediction of hypocalcemia after thyroidectomy using parathyroid hormone: an analysis of pooled individual patient data from nine observational studies. J Am Coll Surg. 2007;205(6):748-54.
24. Grodski S, Serpell J. Evidence for the role of perioperative PTH measurement after total thyroidectomy as a predictor of hypocalcemia. World J Surg. 2008;32(7):1367-73.
25. Soon PS, Magarey CJ, Campbell P, Jalaludin B. Serum intact parathyroid hormone as a predictor of hypocalcaemia after total thyroidectomy. ANZ J Surg. 2005;75(11):977-80.
26. Sywak MS, Palazzo FF, Yeh M, Wilkinson M, Snook K, Sidhu SB, et al. Parathyroid hormone assay predicts hypocalcaemia after total thyroidectomy. ANZ J Surg. 2007;77(8):667-70.
27. Toniato A, Boschin IM, Piotto A, Pelizzo M, Sartori P. Thyroidectomy and parathyroid hormone: tracing hypocalcemia-prone patients. Am J Surg. 2008;196(2):285-8.
28. Scurry WC Jr, Beus KS, Hollenbeak CS, Stack BC Jr. Perioperative parathyroid hormone assay for diagnosis and management of postthyroidectomy hypocalcemia. Laryngoscope. 2005;115(8):1362-6.
29. Di Fabio F, Casella C, Bugari G, Iacobello C, Salerni B. Identification of patients at low risk for thyroidectomy-related hypocalcemia by intraoperative quick PTH. World J Surg. 2006;30(8):1428-33.
30. Khafif A, Pivoarov A, Medina JE, Avergel A, Gil Z, Fliss DM. Parathyroid hormone: a sensitive predictor of hypocalcemia following total thyroidectomy. Otolaryngol Head Neck Surg. 2006;134(6):907-10.
31. Erbil Y, Bozbora A, Ozbey N, Issever H, Aral F, Ozarmagan S, et al. Predictive value of age and serum parathormone and vitamin d3 levels for postoperative hypocalcemia after total thyroidectomy for nontoxic multinodular goiter. Arch Surg. 2007;142(12):1182-7.
32. Wiseman JE, Mossanen M, Ituarte PH, Bath JM, Yeh MW. An algorithm informed by the parathyroid hormone level reduces hypocalcemic complications of thyroidectomy. World J Surg. 2010;34(3):532-7.
33. Vescan A, Witterick I, Freeman J. Parathyroid hormone as a predictor of hypocalcemia after thyroidectomy. Laryngoscope. 2005;115(12):2105-8.
34. Lam A, Kerr PD. Parathyroid hormone: an early predictor of postthyroidectomy hypocalcemia. Laryngoscope. 2003;113(12):2196-200.
35. Payne RJ, Tewfik MA, Hier MP, Tamilia M, Mac Namara E, Young J, et al. Benefits resulting from 1- and 6-hour parathyroid hormone and calcium levels after thyroidectomy. Otolaryngol Head Neck Surg. 2005;133(3):386-90.
1. MD, MSc. in Sciences (Head of the Otorhinolaryngology and Head and Neck Surgery Department at the São José Hospital in Joinville - SC, Brazil).
2. PhD (Professor of Otorhinolaryngology, Head and Neck at Campinas State University - UNICAMP).
3. MD (Head and Neck Surgeon and Craniomaxillofacial Surgeon at the São José Hospital in Joinville - SC, Brazil).
Hospital São José /Joinville e Disciplina de Otorrinolaringologia Cabeça e Pescoço - UNICAMP.
Send correspondence to:
Agnaldo José Graciano
Rua 3 de Maio, nº 58, sala 104, Centro
Joinville - SC. CEP: 89201-030
E-mail: agnaldograciano@yahoo.com.br
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on March 21, 2012.
Accepted on June 7, 2012. cod. 9117.


