INTRODUCTIONThe inflammatory myofibroblastic tumor (IMT) is a benign pseudoneoplastic proliferation, of unknown origin, which involves mainly the gastrointestinal tract, liver and lungs. There are just a handful of cases reported in the literature concerning their involvement of the temporal bone, which is the second one with brain invasion.
CASE PRESENTATIONThis study reports on the case of a 59-year old woman complaining of vertigo and sudden hearing loss on her left side lasting for one month. Upon the physical exam, she had an intact tympanic membrane, though hyperemic.
We ordered an audiogram, which showed severe mixed hearing loss on the left side. In the left-side temporal bone CT scan we found a soft tissue mass occupying the epitympanic and the mastoid antrum regions, sparing the ossicular chain and the scutum; though eroding the lateral semicircular canal (Figure 1A).
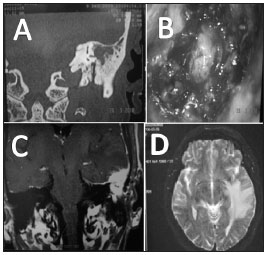
Figure 1. A: Temporal bone CT scan showing a lesion eroding the lateral semicircular canal; B: Tumor aspect during surgery; C: Contrasted skull T1 MRI showing left temporal lobe tumor invasion; D: T2 skull MRI in which we see an important cerebral edema.
We decided to perform a left-side tympanomastoidectomy, in which we noticed a granulous and infiltrative tumoral invasion of the mastoid antrum. We carried out an excisional biopsy of the lesion (Figure 1B). We did not find signs of the lesion extending to the mastoid tegmen into the intracranial region. The pathology report described it as a case of IMT.
Three months after the tympanomastoidectomy, the patient had intense headaches with an episode of seizure. We ordered an MRI of the skull, which showed the lesion next to the middle fossa meninx, hyperintense in gadolinium uptake, invading the left temporal bone, causing a major adjacent cerebral edema (Figure 1C-D). We treated the patient conservatively with deflazacort for an undetermined amount of time, managing to control tumor growth and reducing the brain edema, which maintains until today.
DISCUSSIONThe IMT is a distinct pseudosarcomatous lesion, of unknown etiology1, involving soft tissue and vicera, more frequent in children and young adults2. Temporal bone IMT is difficult to diagnose, since it has a large array of differential diagnostic possibilities, such as malignant external otitis, necrotizing bacterial osteomyelitis, fungal osteomyelitis, cholesteatoma, granulomatous diseases, other primary neoplasias and metastases. CT and MRI are of paramount importance to outline the lesion, because of the latter's capacity to destroy the temporal bone and cause intracranial invasion3,4.
In 2003, Williamsom et al.5 published a review of 10 temporal bone IMT cases. In nine of them they performed total surgical removal and, in one case, it was a subtotal removal. Two cases received steroids, one with a residual tumor and another because of meningeal involvement. In the case with residual tumor, they also used radiotherapy5.
In 2008, Montoya et al.6 published a case of a 75-year old man with a temporal bone IMT, with skull base invasion and involvement of cranial nerves VI, X, XI e XII. The patient was submitted to tympanomastoidectomy and had dura mater erosion and posterior cranial fossa invasion, and he died afterwards.
There is no consensus regarding the best treatment for temporal bone IMT; nevertheless, we have chosen to surgically remove the tumor whenever possible, saving steroids and radiotherapy for those cases in which it is impossible to operate. The decision to use steroids to control the cerebral edema and the symptoms has proven effective in the short run; however, it does not prevent disease progression. Radiotherapy is controversial, because besides the side effects and an unfavorable prognosis in these patients, it failed to prove survival improvements5.
We have seen an increase in the number of these temporal bone tumors in the past 10 years, and its etiology remains uncertain5. The reporting of our case is relevant because of its rarity, being the second report of intracranial invasion and the first with more than one year survival with the disease.
FINAL REMARKSIn summary, temporal bone IMT is rare and represents a very distinct clinical and pathological entity. Despite its benign characteristics, it is usually destructive, involving the middle and inner ears, which can cause bone erosion of the mastoid tegmen and consequent intracranial invasion.
REFERENCES1. Ereño C, López JI, Grande J, Santaolalla F, Bilbao FJ. Inflammatory myofibroblastic tumor of the larynx. J Laryngol Otol. 2001;115(10):856-8.
2. Corsi A, Ciofalo A, Leonardi M, Zambetti G, Bosman C. Recurrent inflammatory myofibroblastic tumor of the glottis mimicking malignancy. Am J Otolarynlol. 1997;18(2):121-6.
3. Patel PC, Pellitteri PK, Vrabec DP, Szymanski M. Tumefactive fibroinflammatory lesion of the head and neck originating in the infratemporal fossa. Am J Otolaryngol. 1998;19(3):216-9.
4. Gasparotti R, Zanetti D, Bolzoni A, Gamba P, Morassi ML, Ungari M. Inflammatory myofibroblastic tumor of the temporal bone. AJNR Am J Neuroradiol. 2003;24(10):2092-6.
5. Williamson RA, Paueksakon P, Coker NJ. Inflammatory pseudotumor of the temporal bone. Otol Neurotol. 2003;24(5):818-22.
6. Santaolalla-Montoya F, Ereño C, Zabala A, Carrasco A, Martínez-Ibargüen A, Sánchez-Fernández JM. Inflammatory myofibroblastic tumor of the temporal bone: a histologically nonmalignant lesion with fatal outcome. Skull Base. 2008;18(5):339-43.
1. MD. ENT Resident.
2. MD. Otolaryngologist; MSc student - Department of Otorhinolaryngology and Head and Neck Surgery - Medical School of the Federal University of São Paulo - UNIFESP.
3. PhD in sciences - UNIFESP; Adjunct Professor - Department Otorhinolaryngology and Head and Neck Surgery - UNIFESP).
UNIFESP.
Send correspondence to:
Gustavo Latorre Samencatti
Rua Agostinho Rodrigues Filho, 350, apto 171B. Vila Clementino
São Paulo - SP. CEP: 04026-040
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on June 14, 2011.
Accepted on September 25, 2011. cod. 8301.


