INTRODUCTION The obstructive hypertrophy of the palatine and pharyngeal tonsils is associated with oral breathing and, when it happens at the stage of facial growth, it may cause important morphofunctional unbalance. The most frequent morphological characteristics in mouth breathing patients are well known: long and narrow face, labial incompetence, retrognathic mandible and maxilla, narrow and deep upper arch, and a lower tongue rest position. Linder-Aronson reported that adenotonsillectomy alone is not enough when other anatomical changes are present, since they impair breathing and prevent growth from happening in a balanced way1-3.
The facial orthopedic techniques used to correct maxillary deformities help reestablish shape and function. The fast maxilla expansion (FME) is a technique based on the cleavage of the median palatine suture by means of a screw which pushes the hemi-maxillae apart4-7.
Having in mind the very limitations of adenotonsillectomy in correcting anatomical and functional facial changes, it is known that the oral breathing child upon development must be treated by a multidisciplinary team. The goal of the present study is to consider growth changes in oral breathing children after adenotonsillectomy and study the importance of the fast maxilla expansion as part of the treatment.
MATERIALS AND METHODS The study was assessed and approved by the Ethics in Research Committee of the teaching institution where it was developed (report number 0427/04), and those responsible for the subjects in this study signed the Informed Consent Form.
Sample Made up by 53 children in the Pediatric Otorhinolaryngology Ward of the institution where it was conducted. Subjects between 6 and 12 years of age, from both genders, were broken down into:
Group 1 or Control: made up by 20 children, nine boys and 11 girls, with oral breathing proven by nasal endoscopy carried out in our institution, with a non-hypertrophic and non-obstructive pharyngeal tonsil occupying less than 40% of the choanal space8 and palatine tonsils level 0, +1 or level +29. We took off the study those children who had had a past of orthodontic treatment and/ or speech therapy, upper airways surgery and craniofacial malformation.
Group 2 or Oral: made up of 33 children with a nasal endoscopy diagnosis of obstructive hypertrophy of the pharyngeal tonsil (occupying 70% of the choanal space)8 and grades 3 or 4 of palatine tonsil hypertrophy (50 to 75% of air passage obstruction in the oropharynx, or more than 75% of air passage obstruction in the oropharynx)9. We took off the study those children who had craniofacial malformation; submitted to orthodontic treatment and/or speech therapy; prior surgery of the upper airways; persistent rhinitis and/or structurally modified concha; nasal septum deviation or any other upper airway obstacle that is not palatine and pharyngeal tonsil hypertrophy. After the diagnosis, all the patients in this group were submitted to adenotonsillectomy, by indication of the otorhinolaryngologist. After surgery, the group was randomly broken down into two subgroups.
Subgroup 2A: 16 children, six girls and 10 boys, not submitted to orthodontic treatment.
Subgroup 2B: 17 children, nine girls and eight boys, submitted to the Hyrax expansion device, installed 30 days after surgery. Initial activation was one complete turn (1.0mm) and during the 12 consecutive days it was one quarter turn in the morning and one quarter turn at night (0.5mm/day)10. The device was kept in place during four months10,11 all the way to the bone new growth at the median palatine suture, when the device was removed and a removable palatine retention plate was installed; left in place for eight months, making up a total of 14 months of retention11.
Cephalometric analysis Measures obtained by means of cephalometric radiographic measures in frontal and side views. Group 1 subjects were radiographed within a 14 month interval, and Group 2 subjects (a and b subgroups) were radiographed before and 14 months after surgery. The following measures were carried out:
Side view SN.Gn (Y growth axis): angle formed between the Saddle, Nasionn and Gnatio points, it establishes the vertical plane of facial growth - represented by Figure 1.
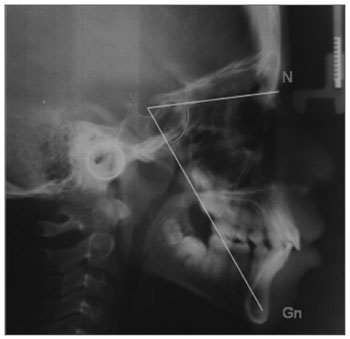
Figure 1. SN.Gn - Angle between the Saddle, Nasion and Gnatio points.
SN.GoMe: angle formed between the anterior skull base (SN) and the mandibular plane (GoMe), it establishes the vertical plane of the facial growth - represented by Figure 2.
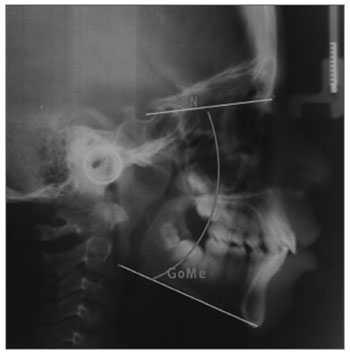
Figure 2. SN.GoMe - Angle between the anterior skull base (SN) and the mandibular plane (GoMe).
FMA: angle formed between the Frankfurt plane and the mandibular plane (GoMe), it establishes the vertical growth plane - represented by Figure 3.

Figure 3. FMA - Angle between the Frankfurt plane and the mandibular plane.
Co-A: linear distance between the condyle and point A, it establishes the effective length of the maxilla - represented by Figure 4.

Figure 4. CoA e CoGn - CoA, linear distance from the condile point all the way to point A; CoGn, linear distance from the condyle point all the way to the Gnatio point.
Co-Gn: linear distance between the condyle point all the way to the Gnatio point, it establishes the effective length of the mandible - represented by Figure 4. Nperp: linear distance from the point A all the way to the perpendicular Nasion line, it positions the maxilla in relation to N - represented by Figure 5.
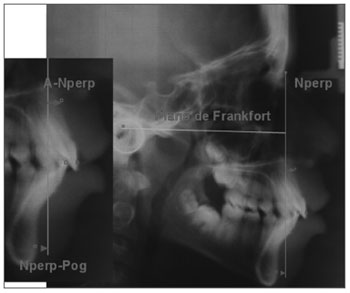
Figure 5. NperpA and NperpPg - NperpA, linear point from point A to the perpendicular Nasion line; NperpPg, linear distance from the Pog point all the way to the perpendicular Nasion line.
Nperp-Pg: linear distance from the Pog point all the way to the perpendicular Nasion line, it positions the mandible in relation to N - represented by Figure 5.
Frontal view Maxilla width: cross-sectional linear measure of JL - JR - represented by Figure 6.

Figure 6. Nasal and maxillary widths - maxillary width: cross-sectional linear measure from JL to JR; nasal width, cross-sectional linear measure from CN to NC.
Nasal width: cross-sectional linear measure of CN - NC - represented by Figure 6.
Statistical analysis The Kolmogorov-Smirnov test was employed in order to study the sample symmetry, which did not follow the Gauss curve. In order to assess possible differences between the initial measures of the control group and oral subgroups, we used the non-parametric test for correlated measures from Kruskal-Wallis. For the possible differences among the measures before and after the procedures within each subgroup, we used the Wilcoxon non-parametric test for correlate measures. For the differences between the groups, for each variable, we used the Kruskal-Wallis nonparametric test for independent groups, complemented by the multiple comparisons test (Δ%), which measures the percentage variation and checks to see which of the groups had the most pronounced improvement.
RESULTS Table 1 shows the average values of the cephalometric variables obtained at the beginning of the study, in the three groups. For the side view variables, there were statistically significant differences in values SN.Gn, SN.GoMe, FMA and Nper-Po; and there were no differences in Co-A, Co-Gn and Nperp-A; for the frontal view variables, there was a statistically significant difference in the maxilla width value and there were no differences in nasal width.
Table 2 compares the control group variables at the beginning and after 14 months of cephalometric follow up. We found significant differences in the following variables: Co-A, Co-Gn, Nperp-A, maxilla width and nasal width.
Table 3 compares the oral 2 A subgroup variables, which were submitted to adenotonsillectomy, without orthopedic intervention. The measures were obtained before and after surgery, within a 14-month time interval. There was a statistically significant difference in the following measures: Sn.GoMe, Co-A and Co-Gn, and there were no statistically significant differences in measures: FMA, SN.Gn, Nperp-Po and Nperp-A. The frontal view cephalometric measures showed statistically significant differences on nasal width and maxilla width.
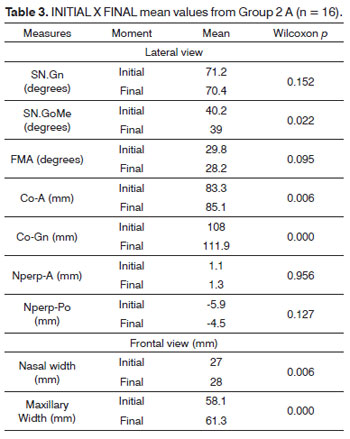
Table 4 compares the variables from subgroup oral 2 B, which was submitted to adenotonsillectomy, followed by the orthopedic maxilla expansion approach. The results showed that there was a statistically significant differences in measures SN.Gn, Co-A and Co-Gn and there were no statistically significant difference in measures FMA, SN.GoMe, Nperp-A and Nperp-Po. In the frontal view we found a statistically significant difference in the nasal width and maxilla width measures.
Table 5 compares the mean intergroup values of all the variables studied. There was a statistically significant difference in variable Co-A among the oral subgroups which were not submitted to ERM and those who were submitted to ERM. The variables: CoGn, Nperp-Po, Sn.Gn, SnGoMe, Nperp-A and FMA did not show statistically significant differences. In the frontal view, there was a statistically significant difference in the nasal width and maxilla width variables.
DISCUSSION The variables which express the facial growth pattern on the vertical direction (SN.Gn, SN.GoMe, FMA) had statistically significant differences when the control group was compared to the oral subgroups studied (Table 1), which means that mouth breathers had a vertical growth pattern vis-à-vis the control group before being submitted to surgery. This growth pattern seems to be a consensus among numerous authors in the literature1,12-25. The Nper-Po variable studies the sagittal proportions of the mandible and we noticed a significant retropositioning of the mandible in the oral groups upon study onset (Table 1), in agreement with the publications available1,12-26. For the frontal view variables, there were statistically significant differences insofar as the maxillary width is concerned, which stresses the maxillary atresia of the oral subgroups at the onset of the study. (Table 1). The mouth breathing children had maxillary atresia before the adenotonsillectomy, seen upon the frontal view cephalometric radiography, and this aspect is also in agreement with the related studies1,22,27.
As we compare the control group variables individually upon onset and after 14 months of cephalometric follow up, we found significant differences in variables: Co-A, Co-Gn and Nperp-A, maxillary and nasal widths. These results mean that the children in the study had the expected sagittal and cross-sectional facial growth, with a stability of the cross-sectional measures (Table 2).
As we studied the oral 2 A subgroup (Table 3), which was submitted only to adenotonsillectomy, without orthopedic intervention, we noticed a significant difference in the Sn.GoMe value, which shows that the vertical growth was controlled after surgery. The significant variables Co-A and Co-Gn indicate maxillomandibular sagittal growth, which occurred similarly to the control group, with indications of facial profile balance. In the frontal view, we found statistically significant differences in the nasal and maxillary widths, a very favorable result, since it points to maxillary atresia control.
As we compared the variables from subgroup oral 2B (Table 4), which was submitted to surgical treatment together with orthopedic intervention, we noticed that the vertical growth pattern was controlled (significant SN.Gn), and the maxillomandibular sagittal measures Co-A and Co-Gn were significantly changed, with a consequent improvement in facial profile. In the frontal view, we found a significant difference in maxillary width and nasal width measures, a cross-sectional gain sign - a very important aspect in reestablishing dental arch perimeters.
The intergroup analysis depicted on Table 5 compares the mean values from all the variables studied. Both oral subgroups had control over the vertical trend of growth seen upon the onset of the study. We found a statistically significant difference in the Co-A variable among the oral subgroups, indicating that the maxillary growth in the sagittal direction (Co-A) of the children submitted to adenotonsillectomy and treated with maxillary expansion was statistically lower when compared to the children submitted to surgery. This difference happened because of the expected orthopedic variations in remodeling the maxillary sagittal growth caused by the expansion device11. Considering the convex profile frequently seen in oral breathers, we understand that the ERM result showed an advantage for introducing efficient maxillary sagittal growth control. In the frontal view, the group treated in association with ERM was also significantly benefited by the cross-sectional gain. Studies published in the literature found nasal atresia in their series of oral breathers and reported that the device causes maxilla expansion and it also increases nasal cavity volume, which improves airflow and reduces oral breathing influence over skeletal structures4-6.
The most evidently modified cross-sectional and sagittal variables after treatment associated to ERM tend to provide more stability and balance to the remaining facial growth.
CONCLUSIONS Adenotonsillectomy balanced the facial vertical growth of patients with oral breathing in this study, even in the untreated group with fast maxilla expansion, and the bone remodeling adjusts induced by facial orthopedics in the cross-sectional and sagittal directions were more evident.
REFERENCES 1. Linder-Aronson S. Adenoids: their effect on mode of breathing and nasal airflow and their relationship to characteristics of the facial skeleton and the dentition. A biometric, rhino-manometric and cephalometro-radiographic study on children with and without adenoids. Acta Otolaryngol Suppl. 1970;265:1-132.
2. Linder-Aronson S. Effects of adenoidectomy on mode of breathing, size of adenoids and nasal airflow. ORL J Otorhinolaryngol Relat Spec. 1973;35(5):283-302.
3. Linder-Aronson S, Henrikson CO. Radiocephalometric analysis of anteroposterior nasopharyngeal dimensions in 6-to 12-year-old mouth breathers compared with nose breathers. ORL J Otorhinolaryngol Relat Spec. 1973;35(1):19-29.
4. Linder-Aronson S, Aschan G. Nasal resistance to breathing and palatal height before and after expansion of the median palatine suture. Odontol Revy. 1963;14(3):254-70.
5. Timms DJ. Rapid maxillary expansion in the treatment of nasal obstruction and respiratory disease. Ear Nose Throat J. 1987;66(6):242-7.
6. Picchi F, Fiorelli G, Bolognini E, Piccini A. Otorhinological evaluations of patients undergoing rapid disjunction of the median palatine suture. Minerva Stomatol. 1990;39(1):15-8.
7. Pérez-Vargas LF. Cambios esqueléticos verticales post-expansión rápida de la maxila en respiradores bucales con relación esquelética de clase II. Metodol Invest [Internet]. 2005 Fev 1 [citado 2008 Sep 29]:[8 p.]. Disponivel em: htttp://www.metodologia-unmsm.com/articulos/fev01/esquelet.htm.
8. Chami FAI. Avaliação nasofibroscópica e radiológica de pacientes com hiperplasia da amígdala faríngea [dissertação]. São Paulo: Universidade Federal de São Paulo; 1997.
9. Brodsky L. Modern assessment of tonsils and adenoids. Pediatr Clin North Am. 1989;36(6):1551-69.
10. Tanaka O, Orellana B, Ribeiro G. Detalhes singulares nos procedimentos operacionais da disjunção palatina. Rev Dental Press Ortodon Ortop Facial. 2004;9(4):98-107.
11. Capelozza Filho L, Silva Filho OG. Expansão rápida da maxila: considerações gerais e aplicação clínica. Parte II. Rev Dental Press Ortodon Ortop Maxilar. 1997;2(4):86-108.
12. Harvold EP, Vargervik K, Chierici G. Primate experiments on oral sensation and dental malocclusions. Am J Orthod. 1973;63(5):494-508.
13. Dunn GF, Green LJ, Cunat JJ. Relationships between variation of mandibular morphology and variation of nasopharyngeal airway size in monozygotic twins. Angle Orthod. 1973;43(2):129-35.
14. Klein JC. Nasal respiratory function and craniofacial growth. Arch Otolaryngol Head Neck Surg. 1986;112(8):843-9.
15. Kerr WJ, McWilliam JS, Linder-Aronson S. Mandibular form and position related to changed mode of breathing - a five-year longitudinal study. Angle Orthod. 1989;59(2):91-6.
16. Behlfelt K, Linder-Aronson S, McWilliam J, Neander P, Laage-Hellman J. Cranio-facial morphology in children with and without enlarged tonsils. Eur J Orthod. 1990;12(3):233-43.
17. Santos-Pinto CCM, Henriques JFC, Pinzan A, Freitas MR, Santos-Pinto A. Estudo radiográfico e de modelos, para a avaliação de alterações dentofaciais em função da redução do espaço nasofaringeano em jovens brasileiros leucodermas de 8 a 14 anos de idade. Ortodontia. 1993;26(2):57-74.
18. Vickers PD. Respiratory obstruction and its role in long face syndrome. Northwest Dent. 1998;77(5):19-22.
19. Faria PT, de Oliveira Ruellas AC, Matsumoto MA, Anselmo-Lima WT, Pereira FC. Dentofacial morphology of mouth breathing children. Braz Dent J. 2002;13(2):129-32.
20. Kawashima S, Peltomäki T, Sakata H, Mori K, Happonen RP, Rönning O. Craniofacial morphology in preschool children with sleep-related breathing disorder and hypertrophy of tonsils. Acta Paediatr. 2002;91(1):71-7.
21. Valera FC, Travitzki LV, Mattar SE, Matsumoto MA, Elias AM, Anselmo-Lima WT. Muscular, functional and orthodontic changes in pre school children with enlarged adenoids and tonsils. Int J Pediatr Otorhinolaryngol. 2003;67(7):761-70.
22. Bizetto MSP, Maruo H, Shimizu RH, Guariza Filho O. Estudo cefalométrico comparativo entre crianças respiradoras bucais e nasais nos diferentes tipos faciais. Rev Dent Press Ortodon Ortop Facial. 2004;9(1):79-87.
23. DiFrancesco RC, Bregola EGP, Pereira LS, Lima RS. A obstrução nasal e o diagnóstico ortodôntico. Rev Dental Press Ortodon Ortop Facial. 2006;11(1):107-13.
24. Peltomäki T. The effect of mode of breathing on craniofacial growth - revisited. Eur J Orthod. 2007;29(5):426-9.
25. Trotman CA, McNamara JA Jr, Dibbets JM, van der Weele LT. Association of lip posture and the dimensions of the tonsils and sagittal airway with facial morphology. Angle Orthod. 1997;67(6):425-32.
26. Lofstrand-Tideström B, Thi lander B, Ahlqvist-Rastad J, Jakobsson O, Hultcrantz E. Breathing obstruction in relation to craniofacial and dental arch morphology in 4-year-old children. Eur J Orthod. 1999;21(4):323-32.
27. Gray LP. Results of 310 cases of rapid maxillary expansion selected for medical reasons. J Laryngol Otol. 1975;89(6):601-14.
1. PhD in Sciences - UNIFESP-EPM (Adjunct Professor in Specialization Programs in Orthodontics).
2. Full Professor of Pediatric Otorhinolaryngology of the Department of Otorhinolaryngology and Head and Neck Surgery at the Medical School of the Federal University of São Paulo - UNIFESP - EPM (Head of the ENT-HNS Department of the UNIFESP - EPM).
3. PhD in Orthodontics - USP (Full Professor of Orthodontics - UNIP).
4. PhD in Sciences - UNIFESP - EPM (Researcher and Professor in Specialization Programs in Orthodontics).
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on August 8, 2011.
And accepted on December 13, 2011. cod. 8715.


